Recurrent Echinococcal Infection of the Lumbar Spine: An 11 Year Follow-up
Article information
Abstract
Spinal hydatid cyst is a rare occurrence in non endemic countries. We present a case of recurrent lumbar hydatid disease in a 21-year-old male who following initial treatment had a good functional outcome and healing for 8 years, following which he came back with complaints of low back ache and neurological deficit. Patient underwent a second surgery with global debridement of L3-L5 vertebrae followed by medical management for two years. He had a good surgical outcome with recovery from the neurological deficit. Patient has returned to his routine activities and is being reviewed every year; there is no evidence of recurrence in the past 3 years. To the best of our knowledge recurrence after 8 years of initial treatment, followed by good clinical and radiological outcome for 3 years after surgery and treatment of the recurrence has not been reported in literature.
Introduction
Human Echinococcosis is a zoonotic infection caused by larval cyst of the dog tapeworm Echinococcus granulosus (E. granulosus) and involves mostly the liver and the lungs. The parasite has two forms E. granulosus and E. multilocularis. E. granulosus uses man, sheep and cattle as an intermediate host. The dog is the common definitive host, transmitting it to humans by direct contact. Hydatidosis affecting the spine comprises less than 1% of the total cases of hydatid disease [1]. A patient with recurrence remains a challenging problem due to its poor prognosis. This case report is unique because 1) recurrences after eight years of symptom free period have not been reported, and 2) the recurrence was managed successfully with combined radical surgical debridement and medical treatment, 3) patient had good functional and radiological outcome and returned to his routine activities. We present a case of hydatid disease of the lumbar spine recurring after 8 years of initial treatment with a good 3 year outcome following second surgery.
Case Report
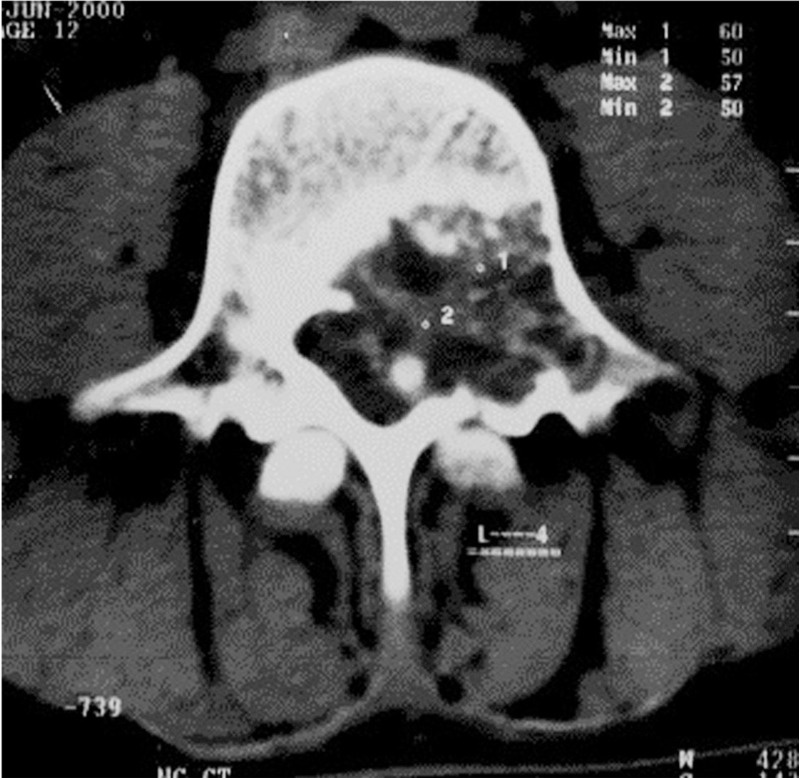
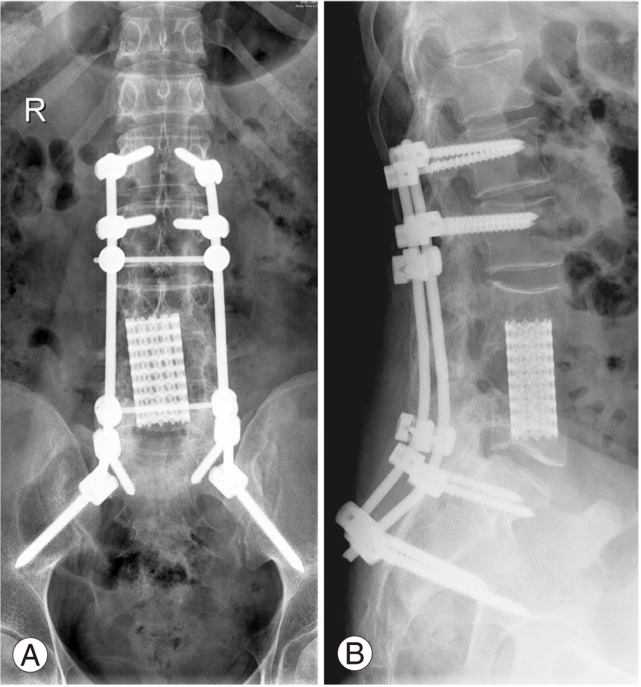
A 21-year-old male presented to the primary physician with complaints of low back ache with radicular pain to both legs without any neurological deficit eleven years ago. He was empirically started on Anti tuberculosis drugs by the primary treating surgeon. After 5 months of treatment he developed worsening of symptoms and was referred to us for further management. He came with low back ache and bilateral lower limb radiating pain. On examination he had hypoesthesia at L4 and L5 dermatome with no motor and autonomic disturbances. Computed tomogram showed bony destruction of L4 vertebrae (Fig. 1) and magnetic resonance imaging (MRI) scan with contrast showed well defined lesions involving the L4 vertebral body, more on the left side and lower end plates of L3 and upper end plates of L5 vetebrae. The lesion measured 4×3 cm and had fluid intensity with no septation, hypo intense on T1 weighted sequence, hyperintense on T2 weighted sequences and did not show any enhancement with gadolinium (Fig. 2). The differential diagnosis was of giant cell tumor, aneurysmal bone cyst and hydatid cyst of L4 vertebra Chest radiograph and ultrasound abdomen was done to rule out involvement of the lungs and liver. Anterior debridement of L3-L5 vertebral body and L3 to L5 tricortical iliac crest bone grafting via anterolateral retroperitoneal approach was done. Then posterior stabilization with mono-axial screws and bone grafting of L3 to L5 was done under general anesthesia. Intra operatively the wound was washed with betadine and 20% hypertonic saline. Histopathological examination showed viable and necrotic lamellar bone enclosing fibrocellular tissue with fibrosis and necrosis. Fragments of laminated membrane lined focally by degenerate germinal layer were seen. Post surgery he recovered without complication. He was started on oral albendazole 400 mg twice a day for four weeks and this regimen was continued for 3 more cycles with 2 week interval between each cycle [2] with regular monitoring of Liver Function test. Patient was reviewed at 3rd month and 6th month and thereafter annually and was asymptomatic, implant was in good position with full recovery from hypoesthesia. Eight years after the surgery he presented with low back pain and bilateral leg pain, more on the right side aggravated by walking (Fig. 3). He had motor power of 2/5 of the right L4, L5 myotome. Since the stainless steel implant was in situ, computerized tomogram (CT) myelography was done (Fig. 4). This showed soft tissue lesion involving L3, L4, and L5 vertebrae extending posteriorly into the spinal canal impinging the thecal sac and exiting L3, L4 nerve root on the right side and L4 nerve root on the left side. Soft tissue mass with a thin calcified capsule and few hypodense areas were suggestive of recurrence of the hydatid disease. Implant removal, debridement and wash out of infected tissue and posterior stabilization with poly-axial screw from L1, L2, S1, and iliac were done. He was started on oral albendazole 400 mg twice daily for 4 weeks. One month post implant exit, MRI (Fig. 5) was done to delineate the extent of soft tissue lesion. A month later anterior retroperitoneal debridement, L4 corpectomy, L3 to L5 fusion with titanium polyaxial screws and cages and postero-lateral bone grafting was carried out. Histopathology showed that in some areas bone and marrow was replaced by amorphous granular eosinophilic necrotic tissue containing few structures resembling degenerated hydatid cyst wall with fragments of laminated membrane lined focally by degenerate germinal layer. Presence of hooklet bearing scolices confirmed the diagnosis of hydatid cyst. Postoperatively he recovered without complications and his neurological deficit improved completely. Postoperatively patient was started on oral albendazole 400 mg twice a day for four weeks, repeated after 2 weeks for two years, monitoring Liver Function once in three months. Patient was reviewed every year after surgery and at the end of 3 years plain radiograph showed implants (Fig. 6) in good position and CT scan showed sound posterolateral fusion. MRI showed no signs of residual lesion. In view of the possibility of further recurrence patient has been advised a yearly follow-up.
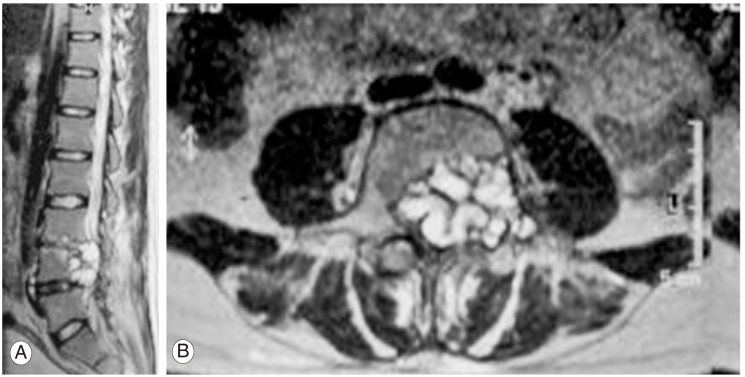
T2 weighted magnetic resonance (MR) image demonstrating multiple cyst with severe canal compromise. (A) T2 weighted MR saggital image showing multiple cyst at L4 vertebrae. (B) T2 weighted axial MR image demonstrating hydatid cyst with canal comprimise.
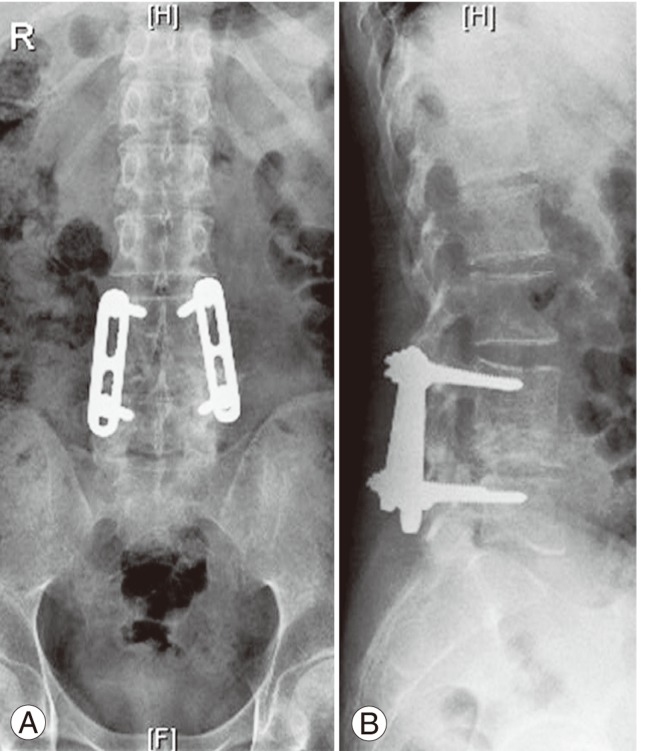
Plain radiograph at 8 years follow-up. (A) Anteroposterior view loss of height of L4 vertebrae with Steffee's plate in situ. (B) Lateral view showing complete destruction of L4 vertebrae .
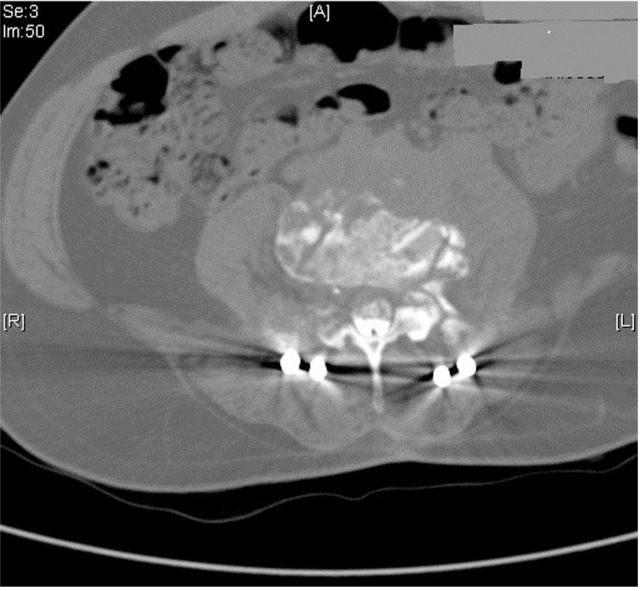
Computed tomography myelogram 8 years after first surgery showing recurrence of hydatid cyst with moderate canal compromise.

T2 weighted magnetic resonance image at 8 years follow-up demonstrating recurrences of cyst at L3-L5 segments with near total destruction of L4 vertebrae. (A) Saggital view. (B) Axial view.
Discussion
Recurrence remains a major problem in spinal hydatidosis. Radiological findings are not a sensitive method in diagnosis; hence CT and MRI are thus used. The literature recurrence ranges from 30% to 100%. This is because of the difficulty in removing the cyst due to its limited access and the vital structures around the vertebrae. The other reason of recurrence is the rupture of the cyst while removing. Surgery is the most common initial treatment for hydatid disease, with total removal of the cysts being the primary goal. In our case both anterior and posterior surgery was done due to circumferential involvement of the vertebra. Chemotherapy is used in conjunction with surgery to prevent recurrence and to protect the patient from dissemination of a ruptured cyst. Albendazole and mebendazole are the two most commonly used antihelminthic drugs. Studies have indicated that prolonged albendazole treatment appears to be safe and effective in of late recurrences after spine hydatidosis surgery [3]. Prabhakar et al. [4] treated recurrence spinal hydatid cyst in three patients with 400 mg of oral albendazole thrice daily for one year. Maity et al. [5] have used albendazole 400 mg daily for 3 months. So far no standard regimen has been postulated for the treatment of recurrences. In our case we continued oral albendazole 400 mg twice daily for 2 year after the second surgery in view of late recurrence. Chaudhary et al. [6] described a case of paraplegia due to recurrent hydatid cyst of spine where there was a recurrence 2 years post surgery, with no recurrence at four years follow-up. Ozdemir et al. [7] in their retrospective study have followed up 3 patients with spinal hydatid, the longest being for 145 months with an average remission time of 37 months but the patients did not have complete neurological recovery. Sapkas et al. [8] presented a case with recurrent paraplegia of thoracic spine, with recurrence within a year of surgery with a poor outcome where the patient refused treatment and died in 2 years. Kaen et al. [9] reported a case of intradural extramedullary spinal hydatosis treated for more than twenty years with the disease affecting the liver and the lungs, following which involvement of thoracic spine with neurological deficit was noted and surgically treated with a recurrence within 6 months with minimal improvement in his neurological status. Hence studies have concluded that the recurrence rate was 100%. We present this case of late recurrence of lumbar hydatid infection after 8 years of initial treatment with good functional and radiological outcome. Late recurrences after eight years of symptom free period have not been reported in literature to our knowledge. We have managed the recurrence with a combination of surgery and prolonged anthelmintic therapy with a follow-up for three years with good clinical and radiological outcome. Medical management and radical surgical debridement of involved vertebrae has an important role in effective removal of lesion and reducing the load of organism and thereby possible cure of the disease. Long term regular follow-up is required for early diagnosis of recurrences. Standard medical regimen for the treatment of recurrent hydatid cyst is debatable. Hence it remains a topic for discussion as the outcome of patients having a recurrence has been poor either due to incomplete treatment or due to the spillage of the cyst. Though complete cure is hard to achieve or prove early diagnosis, prompt surgical debridement with adequate and appropriate anthelmintic therapy with regular follow-up are mandatory to eradicate the disease and in providing longer symptom free periods with good outcome.
Notes
No potential conflict of interest relevant to this article was reported.