Cross-Cultural Adaptation, Validation, and Reliability Testing of the Modified Oswestry Disability Questionnaire in Persian Population with Low Back Pain
Article information
Abstract
Study Design
Prospective study.
Purpose
We aimed to validate the Persian version of the modified Oswestry disability questionnaire (MODQ) in patients with low back pain.
Overview of Literature
Modified Oswestry low back pain disability questionnaire is a well-known condition-specific outcome measure that helps quantify disability in patients with lumbar syndromes.
Methods
To test the validity in a pilot study, the Persian MODQ was administered to 25 individuals with low back pain. We then enrolled 200 consecutive patients with low back pain to fill the Persian MODQ as well as the short form 36 (SF-36) questionnaire. Convergent validity of the MODQ was tested using the Spearman's correlation coefficient between the MODQ and SF-36 subscales. Intraclass correlation coefficient (ICC) and Cronbach's α coefficient were measured to test the reliability between test and retest and internal consistency of all items, respectively.
Results
ICC for individual items ranged from 0.43 to 0.80 showing good reliability and reproducibility of each individual item. Cronbach's α coefficient was 0.69 showing good internal consistency across all 10 items of the Persian MODQ. Total MODQ score showed moderate to strong correlation with the eight subscales and the two domains of the SF-36. The highest correlation was between the MODQ and the physical functioning subscale of the SF-36 (r=–0.54, p<0.001) and the physical component domain of the SF-36 (r=–0.55, p<0.001) showing that MODQ is measuring what it is supposed to measure in terms of disability and physical function.
Conclusions
Persian version of the MODQ is a valid and reliable tool for the assessment of the disability following low back pain.
Introduction
Self-reported measures of disability are widely used to measure the outcome of the treatment received for low back pain [1]. Modified Oswestry low back pain disability questionnaire (ODQ) is a well-known condition-specific outcome measure that helps quantify disability in patients with lumbar syndromes [2]. Because of the low response rate to items asking about gender, Fritz and Irrgang [3] made this modification on the original questionnaire. They replaced the gender item with an item describing employment and homemaking. The modified ODQ consists of 10 items each scored from 0 to 5. The total is calculated through multiplying the sum of the scores by 2, giving a range of 0 to 100; a higher score reflects higher disability.
Persian is one of the most commonly spoken languages in the middle-east region including Iran, Afghanistan, Tajikistan, and some parts of Iraq and Pakistan. Asking patients about their sexual behavior may not be acceptable in some cultures in these countries. However, to protect the psychometric properties of this tool, cross-cultural adaptation is necessary [45]. Thus, we aimed to validate and cross-culturally adapt the translated Persian version of the modified ODQ for Persian-speaking population in gauging treatment outcome for low back pain.
Materials and Methods
1. Patients
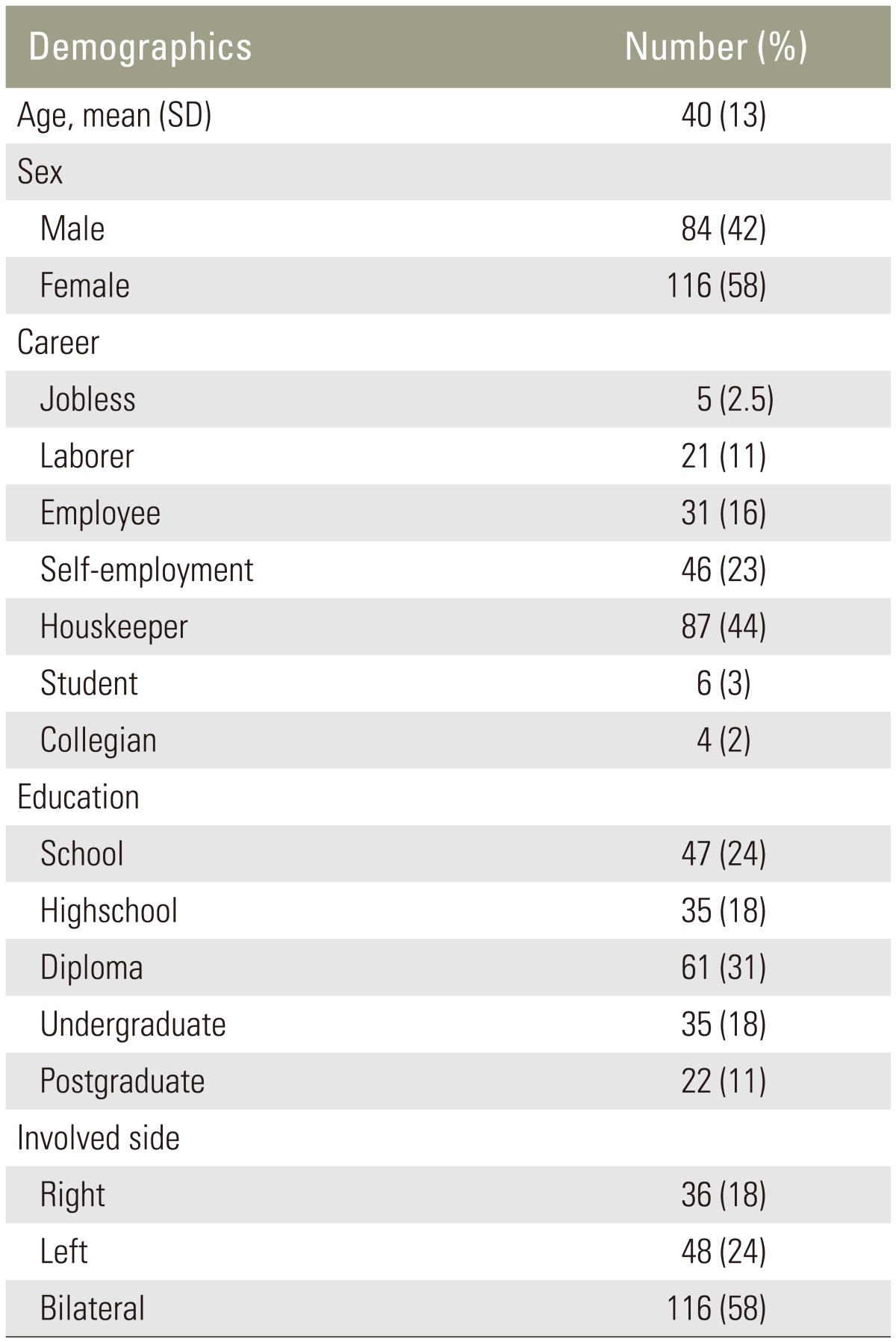
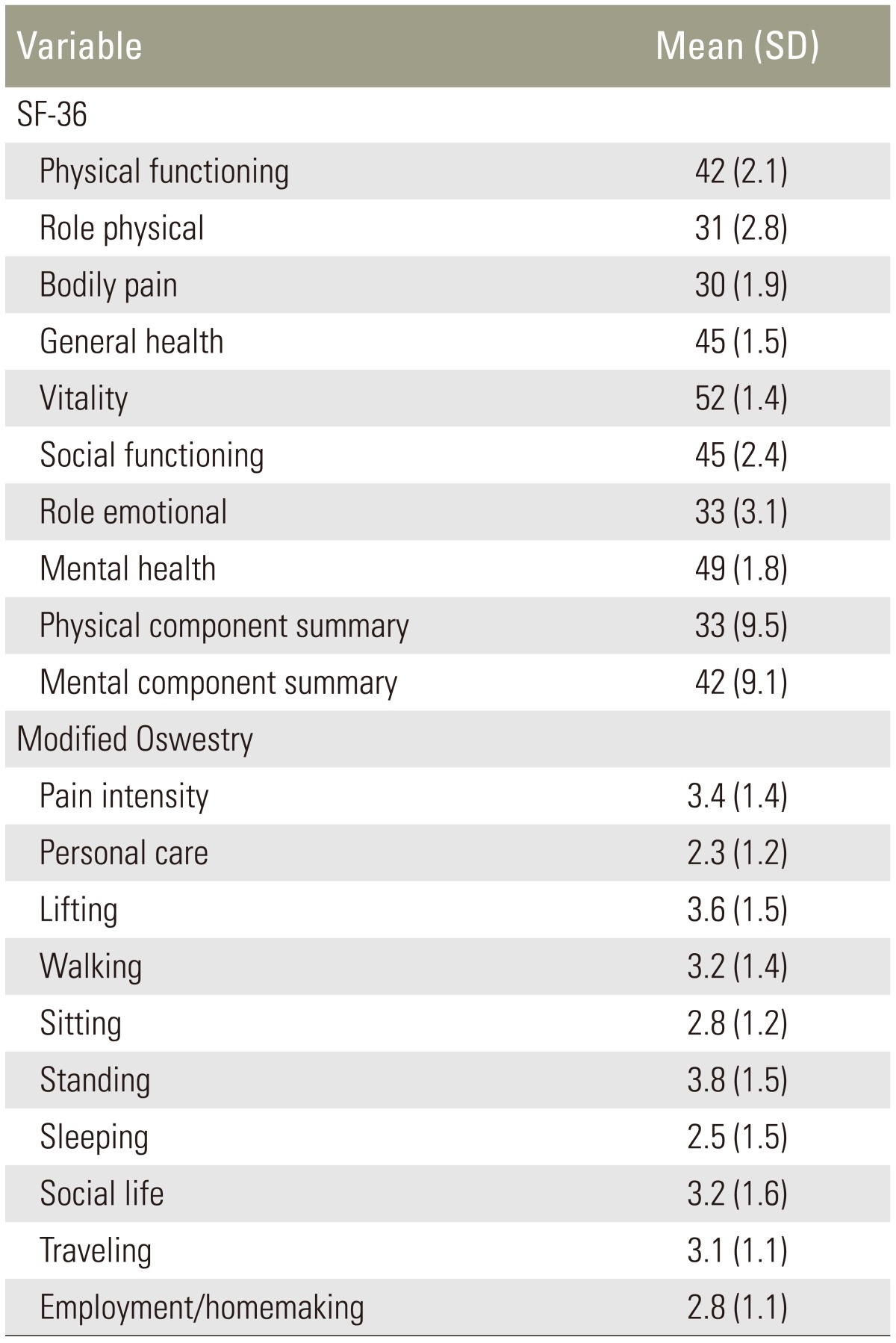
In this Institutional Review Board approved study, we enrolled 200 consecutive patients from the spine clinic from September 2014 to February 2015. Patients with low back pain, aged 18 years or older, with symptom duration of more than 2 months were included in this study. Patients with neoplasm, radiating pain from other sites, infection, and systemic inflammatory disease were excluded (Tables 1, 2). All participants were literate native Persian speakers.
2. Translation
Following Beaton's guidelines for cross-cultural adaptation of the modified ODQ, three independent Persian-speaking individuals including two general orthopedic surgeons and one professional English tutor with no medical background translated the original English version of the modified ODQ to Persian (also known as Farsi) [4]. These three translations were then reviewed and reconciled into a single Persian modified ODQ version. In the next step, a native American English speaker fluent in Persian that was not aware of the original English version of the MODQ translated this Persian version back into English and the conformity this version with the original English version of the MODQ was measured.
Agreement of the Persian and the original English modified ODQ was evaluated in the presence of the authors and professional translators addressing the "back to English" translation. After this, we reached a consensus for the penultimate version of our Persian MODQ. To test the validity of this version in a pilot study, this Persian modified ODQ was administered to 25 individuals with low back pain. Minimal obstacles in understanding the questionnaire were rectified and the final version was designed (Suppl. Fig. 1).
3. Modified Oswestry disability questionnaire
In 1980, Fairbank et al. [2] created and introduced the Oswestry low back pain disability index. This questionnaire was applied for many years and was reported to be reliable, valid, and compatible with conditions with low back pain [26]. However, several modifications have been done on this tool [36]. Because of the low response rate to questions about sex life, the last modified ODQ replaced these questions with the ones for employment/home making [7]. This tool is a self-administered 10-item questionnaire that takes less than 5 minutes to complete. Items are mainly questioning about pain intensity related to the activities of daily living. Each item is responded using six statements describing an escalating level of severity to a particular activity scoring from 0–5. To report the raw scores in percentage, all items must be added together and multiplied by 2 to show the percentage of disability with the higher score representing higher pain intensity and disability [2].
4. Psychometric properties
Intraclass correlation coefficient (ICC) and Cronbach's α coefficient were used to test the reliability between test and retest and internal consistency of all items, respectively. Convergent validity of the modified ODQ was tested by using the validated Persian short form 36 (SF-36) survey and applying the Spearman's correlation coefficient between the modified ODQ and SF-36 subscales [8].
Results
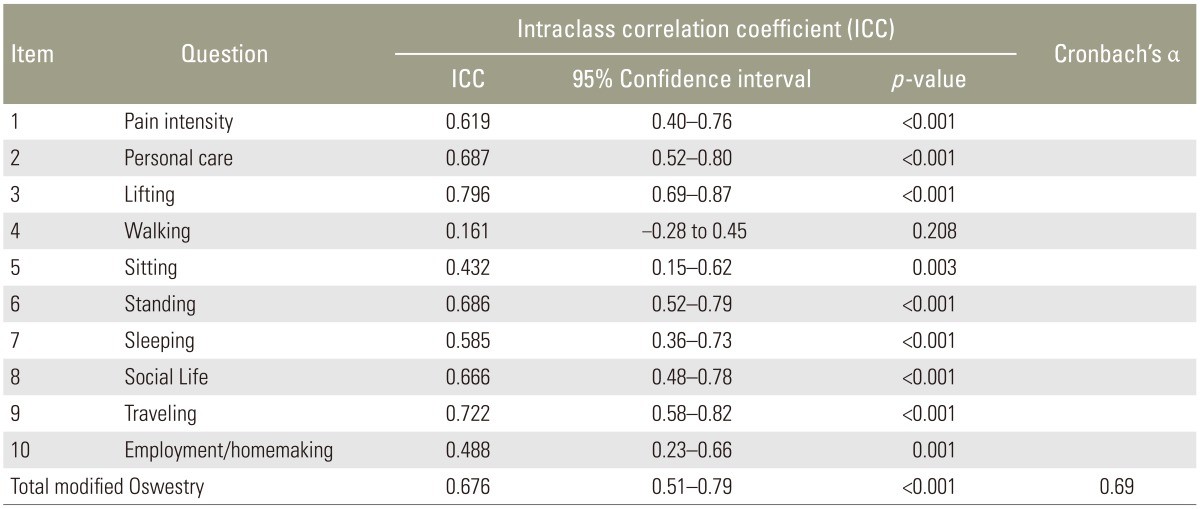
The total modified ODQ score showed good reliability with a high and significant ICC between test and retests (Table 3). ICC for individual items mainly ranged from 0.43–0.80 showing a good reliability and reproducibility of each individual item (Table 3).
Cronbach's α coefficient was 0.69 showing good internal consistency across all 10 items for the Persian modified ODQ. Cronbach's α was almost the same at the first and second visit for the total measure (Table 3).
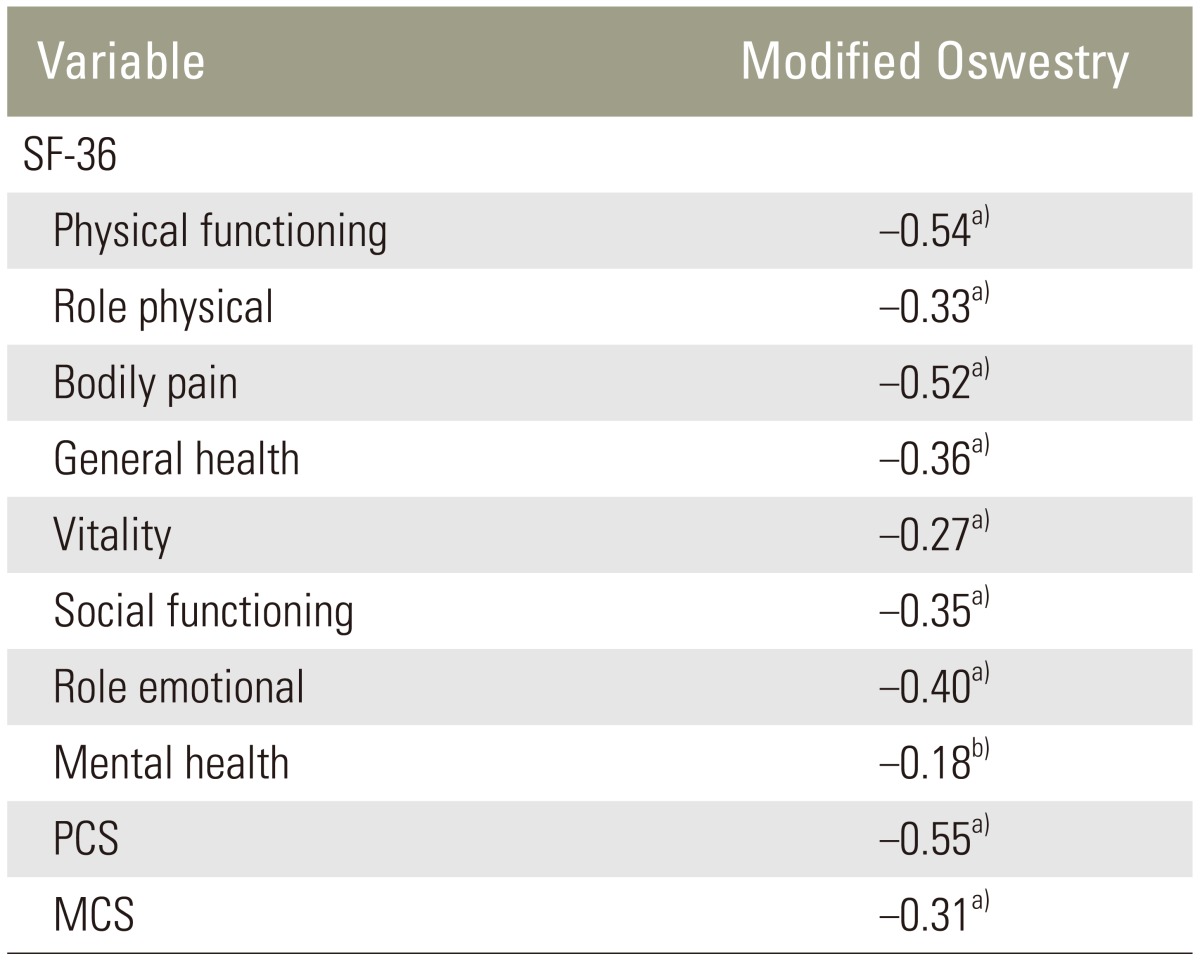
Total modified ODQ showed moderate to strong correlation with the eight subscales and the two domains of the SF-36. The highest correlation was between the modified ODQ and the physical functioning subscale of the SF-36 (r=–0.54, p<0.001) and the physical component domain of the SF-36 (r=–0.55, p<0.001) showing that a high dependability of MODQ in measuring disability and physical function (Table 4).
Discussion
The aim of our study was to test the validity and reliability of the Persian version of modified ODQ for the Persian speaking population with low back pain conditions. We confirmed the validity and reliability of the Persian modified ODQ and usefulness of this instrument in quantifying the functional disability.
One of the limitations to our study is that we administered the modified ODQ to patients who previously had lumbar surgery regardless of the time passed after the surgery. Another limitation of our current study is that we validated the region-specific modified ODQ in respect to a more general measure such as SF-36. However, SF-36 is an appropriate patient-based questionnaire proved to be useful in validating the questionnaires while representing the quality of life [9].
The thorough questionnaire demonstrated good reliability, good internal consistency, and confirmed convergent validity. By comparing the modified ODQ with the SF-36 questionnaire, the convergent validity was tested that showed a moderate to strong correlation. Both reliability and validity level of the Persian version were as high as the original English version. The high and significant correlation between modified ODQ and subscales of function in SF-36 demonstrated the conformity of their context in that both are measuring what they are supposed to measure namely disability and physical function.
Good test-retest reliability of the present study strongly corresponded to previous studies of the Modified version of the ODQ [310]. Baker et al. [11] reported high reliability of the modified ODQ (r=0.89). Comparing the modified ODQ and the Quebec back pain disability scale (QUE), Fritz and Irrgang [3], showed superior reliability of the modified ODQ with ICC for the modified ODQ of 0.90 (95% confidence interval [CI ], 0.78–0.96) and for the QUE of 0.55 (95% CI, 0.20–0.78). The ICC for testing the reliability of individual items of the Thai version ranged from 0.82–0.99 and the ICC for the total score was 0.98 showing excellent reliability [10].
Conclusions
Similar to those of prior validation studies, Persian version of modified ODQ was found to be valid and reliable for low back pain disability assessment in an Iranian population. For a patient centered tool, slight differences tailored for cultural adaptation are acceptable as far as the results prove to be valid and reliable [12].
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
Supplementary Materials
Suppl. Fig. 1
Persian version of the modified Oswestry disability questionnaire is shown that is validated. Supplementary material can be found at http://www.asianspinejournal.org/src/sm/asj-10-215-s001.pdf.