The Relationship between the Progression of Kyphosis in Stable Thoracolumbar Fractures and Magnetic Resonance Imaging Findings
Article information
Abstract
Study Design
Retrospective study.
Purpose
To investigate the relation between the progression of kyphotic deformity and magnetic resonance imaging (MRI) findings in conservatively treated stable thoracolumbar fractures.
Overview of Literature
When treated conservatively, excessive progression of kyphotic deformity and vertebral compression can emerge during follow-up. We sought to identify predictors of vertebral body deformation using MR images.
Methods
The presence in MR images of anterior longitudinal ligament (AL) or posterior longitudinal ligament (PL) injury, superior or inferior endplate disruption, superior or inferior disc injury in fractured vertebral bodies, the existence of low signal intensity on T2 weighted images, and bone edema of intravertebral bodies were assessed.
Results
The presence of superior endplate disruption and a higher level of bone edema were found to cause the progressions of kyphotic angle (KA), wedge angle (WA), and anterior vertebral compression (AVC) rate. When AL or superior disc injury was observed, only KA increased meaningfully. When low signal intensity was present on T2 weighted images WA and AVC increased significantly, but PL injury, inferior endplate disruption, and inferior disc injury showed no notable correlation with kyphotic deformity progression. The risk factors found to be associated with an increase of KA to >5° were AL injury, superior endplate disruption, superior disc injury, and a bone edema level of over 1/3, and their associated risks versus no injury cases were 14.1, 3.7, 6.8, and 10.4-fold, respectively.
Conclusions
AL injury, superior endplate and disc injury, or a high level of bone edema, were critical factors that determine kyphotic deformity progression.
Introduction
A stable vertebral fracture generally indicates a fracture with kyphotic angle of <30° and vertebral compression of <50% not associated with posterior column injury [1,2,3]. For these stable thoracolumbar spine fractures invasive treatments can be considered, but conservative treatments have been reported to provide good results [2,4,5,6,7]. Furthermore, if a satisfactory outcome can be expected after conservative treatment, it represents a better option than surgical treatment in terms of cost and the risks of complications. However, when treated conservatively, excessive progression of kyphotic deformity and vertebral compression can emerge during follow-up with subsequent developments of back and flank pain, and neurological complications [8,9,10,11].
Therefore, we considered that the identification of reliable predictors of the progression of vertebral body deformation would be useful. Magnetic resonance imaging (MRI) is a clinically and experimentally verified diagnostic tool in cases of thoracolumbar injury for detecting injury levels in ligaments, discs, endplates, and vertebral bodies [12]. In the present study, we sought to identify predictors of vertebral body deformation using MR images and to utilize them clinically.
Materials and Methods
1. Materials
One hundred and eleven patients that visited our hospital from September 2007 to April 2014 with a compression fracture or a stable thoracolumbar burst fracture with no neurological involvement based on McAfee's et al. [13] thoracolumbar injury classification and with over 3 months of follow-up after conservative treatment using a thoracic-lumbar-sacral orthosis (TLSO) brace were the subjects of the present study. The cohort consisted of 47 males and 64 females of overall average age 49.1 years (range, 22-67 years). 47 (42%) were injured in traffic accidents and 37 (33%) in a fall. These patients were selected after confirming acute fracture by MRI. However, those with an osteoporotic fracture, a pathological fracture, or multiple fractures were excluded.
2. Methods
The presence of the anterior and posterior longitudinal ligament injury, superior or inferior endplate fracture, superior or inferior disc injury in the fractured vertebral body, the existence of low signal intensity on T2 weighted images, the bone edema level of the intravertebral body were assessed by examining initial MR images taken within 48 hours of injury. Patients were allocated to groups as follows.
For anterior and posterior longitudinal ligament injuries, group AL (PL) 1 with no evidence of injury, or group AL (PL) 2 with no discontinuity but with slackening, stripping, or rupture of the longitudinal ligament.
For endplates superior and inferior, group EP S (EP I) 1 with plastic deformity only without disruption, or group EP S (EP I) 2 with evident disruption.
For vertebral discs superior and inferior, group DI S (DI I) 1 with no evidence of injury, or group DI S (DI I) 2 with evident rupture or debris.
For bone edema level of the intravertebral body on T1 weighted images, group VB 1 with an edema level under 1/3, group VB 2 with an edema level of 1/3 to 2/3, or group VB 3 with an edema level over 2/3.
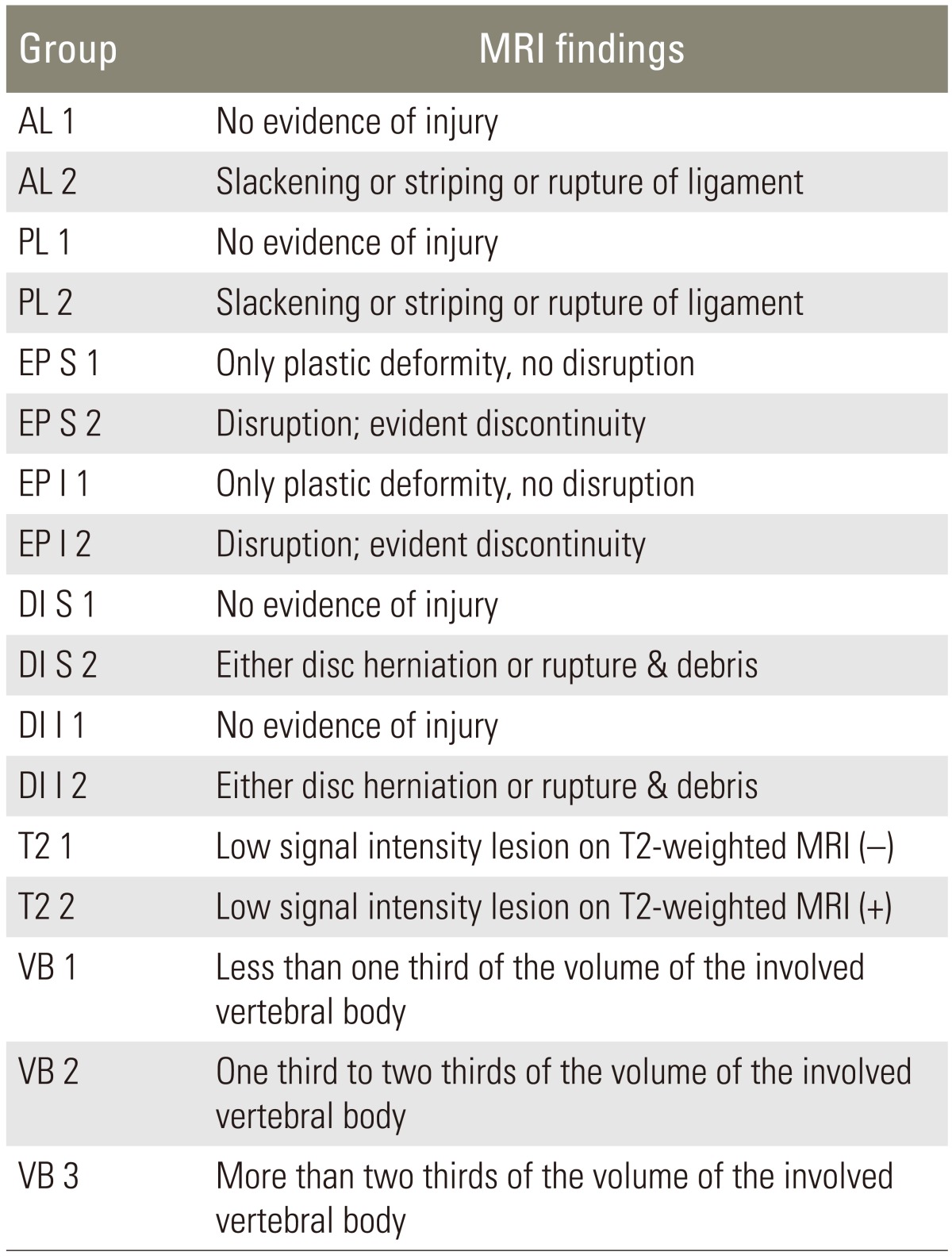
For the low signal lesions on T2 weighted images, group T2 1 with no presence of low signal intensity or group T2 2 with the presence of low signal intensity (Table 1, Fig. 1).

Features of ligament, disc, endplate and vertebral bodies on magnetic resonance images. AL 2: slackening, striping, or rupture of the anterior longitudinal ligament, PL 2: slackening, striping, or rupture of the posterior longitudinal ligament, DI 2: disc herniation or rupture, EP 2: endplate disruption or evident discontinuity, T2 2: low signal intensity lesion +, VB 2: bone edema level >1/3 and <2/3, VB 3: bone edema level >2/3.
On confirming acute fractures, TLSO braces were manufactured and immediately applied, and then patients were allowed upright ambulation and daily activities. Kyphotic angles, wedge angles, and anterior vertebral body compression rates on lateral radiographs were measured and used to calculate vertebral deformity. Kyphotic angle was defined as the angle formed between a line drawn parallel to the superior endplate of the vertebrae above the fractured body and a line drawn parallel to the inferior endplate of the vertebrae below the fractured body, using Cobb's method. Wedge angle was defined as the angle made by the superior and inferior endplates of the fractured vertebral body. Anterior vertebral compression rate was obtained by expressing the anterior height loss of the fractured vertebrae as a percentage of the average anterior height of adjacent upper and lower vertebrae (Fig. 2). The statistical analysis was executed using SPSS ver. 21 (IBM Co., Armonk, NY, USA). The Student's t-test and one-way analysis of variance were used to analyze categorical MRI variables. Variables were considered statistically significant when their significance levels were <0.05. Logistic regression analysis was used to identify risk factors of an increase of kyphotic angle to >5° and their odds ratios.
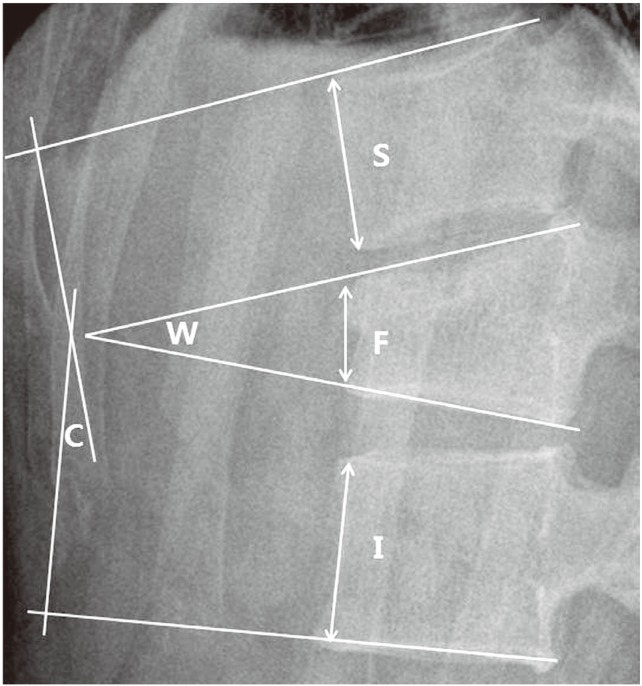
Measurement of radiological parameters. C°, kyphotic angle by Cobb's method; W°, wedge angle, anterior vertebral compression rate (%): 100 (1-2F/[S+I]); S, anterior vertebral height superior to the fractured body; I, anterior vertebral height inferior to the fractured body; F, anterior vertebral height of the fractured body.
Results
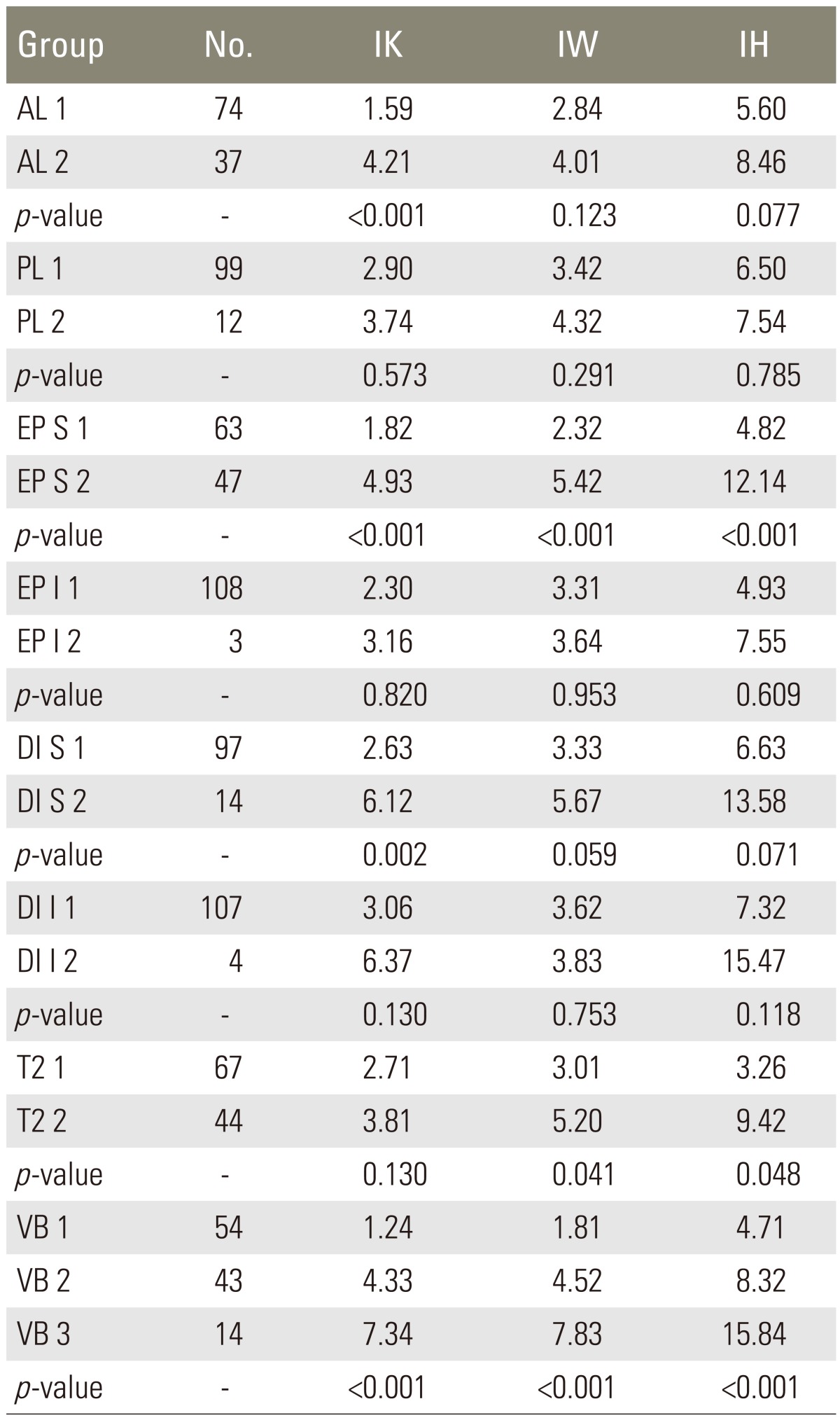
Regarding fracture sites, there were 7 cases involving the seventh-tenth thoracic vertebrae, 69 cases involving the thoracolumbar junction (eleventh thoracic vertebrae-first lumbar vertebrae), and 35 cases involving the second-fifth lumbar vertebrae. The average follow-up was 12 months (range 3.5-78 months). There were 37 cases of anterior longitudinal ligament injury (AL 2), 12 cases of posterior longitudinal ligament injury (PL 2), 47 cases of superior endplate injury (EP S), and 3 cases of inferior endplate injury (EP I). And there were 14 cases of superior disc injury at the fractured vertebral body (DI S) and 4 cases of inferior disc injury (DI I). In addition, 44 cases had low signal intensity lesion on T2 weighted images (T2 2), 43 cases had an intravertebral bone edema level of 1/3-2/3 (VB 2) and 14 had a bone edema level of over 2/3 (VB 3) (Table 2). In all patient groups average progressions of kyphotic angle and wedge angle were 3.1° (range, -3.8 to 13.1°) and 3.6° (range, -3.5° to 13.3°), respectively, and average anterior vertebral compression progressed by 7.5% (range, -6.1% to 45.6%).
In cases of superior endplate disruption or a higher bone edema level in the intravertebral body, kyphotic angle, wedge angle, and anterior vertebral compression proceeded significantly. Average progressions of kyphotic angle, wedge angle, and anterior vertebral body compression were 1.8°, 2.3°, and 4.8%, respectively, when there was no superior endplate disruption (EP S 1), and in contrast, were 4.9°, 5.4°, and 12.1%, respectively, when superior endplate disruption existed (EP S 2). And they were 1.2°, 1.8°, and 4.7%, respectively, when the bone edema level in the intravertebral body was under 1/3, 4.3°, 4.5°, and 8.3% when the bone edema level was 1/3 to 2/3, and 7.3°, 7.8°, and 15.8% when the bone edema level was over 2/3 (Table 2).
When an AL injury or superior disc injury was present, only the kyphotic angle increased significantly. The average progression of kyphotic angle in the presence of AL injury (AL 2) was 4.2°, but was 1.6° in the absence of AL injury (AL 1). For the superior disc injury, average progressions of kyphotic angle in the presence or absence of superior disc injury were 6.1° (DI S 2) and 2.6° (DI S 1), respectively (Table 2).
Regarding low signal intensity lesions on T2 weighted images, the progression of wedge angle and anterior vertebral compression in its presence and absence were 5.20° and 9.42% (T2 2), 3.01° and 3.26% (T2 1), respectively (Table 2).
For posterior longitudinal ligament injury, inferior endplate disruption and inferior vertebral disc injury showed no notable correlation with kyphotic deformity or the progression of vertebral compression.
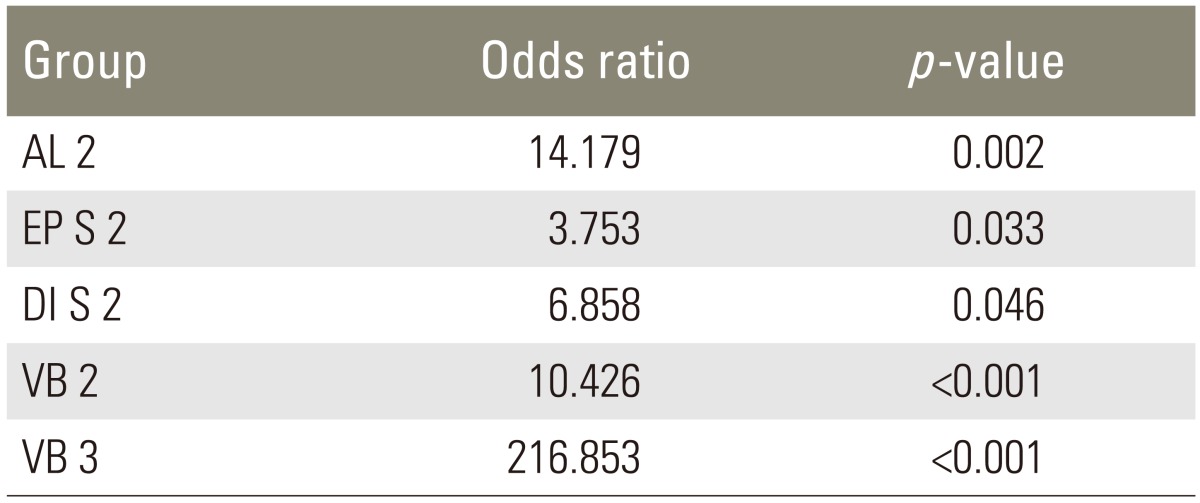
The risk factors associated with an increase of kyphotic angle to >5° were the presence of AL injury, superior endplate disruption, superior disc injury, and an intravertebral edema level of over 1/3, and their associated risks versus no injury cases were 14.1, 3.7, 6.8 and 10.4-fold, respectively. Notably, the risk was enhanced up to 200-fold when the edema level was over 2/3 (Table 3).
Discussion
Spine surgeons are still confused about choosing the proper therapeutic options for stable burst fractures. It has been reported that surgical treatments result in better functional outcomes and that conservative treatments are at risk of the development of neurological complications [8,14] and of complications like thrombosis, embolism, and urinary tract infection [2,10,15].
On the other hand, the conservative treatments may yield fully satisfactory results without any functional deficit [5,10]. It has been reported that the difference between the final follow-up kyphotic deformity after conservative treatment and those that occurred just after injury was not strongly supported statistically, and most of the resultant vertebral column deformity takes place at the time of injury [4]. Furthermore, the risk of equipment failure or kyphotic deformity recurrence can be as high as 56% after surgical management [11,16,17,18,19].
Generally, for compression fractures and stable burst fractures, as defined by the McAfee classification [13], with no posterior ligament complex injury, surgical treatment is performed when vertebral compression is >50%, kyphotic angle is >30°, or canal encroachment is >50%. Compression and burst fractures with no neurological involvement, vertebral compression <50%, and a kyphotic angle <30° are considered stable fractures, and in these fractures, conservative treatment with braces also produces good outcomes [2,5,6,7]. However, anterior vertebral height loss and kyphotic deformity may occur during follow-up. Those radiological findings of vertebral body deformation are not necessarily related to clinical or functional results [2,10,20,21], but the progression of vertebral body compression and kyphotic deformity may aggravate back or lumbar pain, and cause neurological symptoms [8,10,11,22,23]. However, few studies have addressed relations between factors related to the progression of vertebral body deformation, and therefore, efforts should be made to identify reliable predictors of this progression.
MR images enable the multilevel visualization, as on sagittal and axial planes, of vertebral alignments, the injury states of discs and ligaments, fracture edema levels, and of the status of epidural hematoma, and can provide information about the spinal cord. Although MRI may be less sensitive for cortical bone fractures than computerized tomography (CT), because relatively few mobile protons are present in cortical bone, bone marrow changes induced by fractures provide considerable sensitively. In particular, MRI is being used clinically for the evaluation of disc and ligament injuries, including injuries of the posterior ligament complex [12].
The present study was initiated by asking the question 'Whether the progression of kyphotic deformity and vertebral body compression can be predicted by MRI for vertebral fractures?', that is, by utilizing radiological findings of the anterior and posterior longitudinal ligaments, the superior and inferior disc and endplates, bone edema level, and low signal intensity lesions on T2 weighted images.
The most important factor regarding stability and the prevention of kyphotic deformity in stable burst fractures (McAfee classification [13]) is the condition of the posterior ligament complex, and for injuries of this structure, operative treatments have been reported to yield better outcomes than conservative treatments [24,25]. At our hospital, patients with posterior ligament complex injuries are treated surgically, too, and therefore, were not included in the present study.
AL injuries can be caused by a rotational or shear force, or by a force bursting out of a vertebral body or disc [24,26]. PL injuries are mostly caused by flexion force or by a force bursting out of an endplate or disc, and the PL is known to be an important structure for the indirect reduction of encroaching fracture fragments. If there is unrecognized ligamentous injury in conservatively treated patients, kyphotic deformity can progress and persistent pain can develop [24]. In the present study, kyphotic angles increased significantly by 4.2° on average in the presence of AL injury, and AL injury was confirmed to be an important cause of kyphotic deformity, since it was found to increase the risk of kyphotic angle.
The presence of endplate disruption or bone edema of over 1/3 into the vertebral body on MR images may significantly affect kyphotic deformity progression [24]. In addition, when there are superior endplate fractures, an acted external force may be high and when the edema level exceeds 1/3 on MR images, damage to the trabecular bone in the intravertebral body may be extensive [27]. In such cases, excessive kyphotic angle deformation can be expected to advance [27]. In the present study too, when superior endplate disruption was present or the edema level exceeded 1/3 of the intravertebral body, kyphotic angle, wedge angle and anterior vertebral compression rate were observed to increase significantly, which confirmed that these two factors determine the progression of kyphotic deformity. In particular, the risk of the kyphotic angle increasing by more than 5° was 3.7-fold higher when the superior endplate was disrupted, 10.4-fold higher when the bone edema level was between 1/3 and 2/3, and notably 216-fold higher when the bone edema level was >2/3, than in cases without injury, which showed the bone edema level of over 2/3 is a critical factor in determining kyphotic deformity progression.
When an external force is applied to the disc, its morphology is altered and tissue redistribution takes place. Therefore, gradual settlement of the vertebral disc into the injured superior endplate and vertebral body is considered an important factor in the progression of kyphotic deformity, along with compression of the vertebral body per se [11,28]. In the present study, significant increases in kyphotic deformity caused by the disc settlement into the vertebral body were observed in cases of superior disc injury in fractured vertebral bodies. Furthermore, the risk of progression of kyphotic angle to >5° was found to be 6.8-fold higher for a superior disc injury as compared with no disc injury. Wedge angle and anterior vertebral compression also tended to be enhanced in the presence of superior disc injury, but this was not statistically meaningful. This seems to be why in some patient groups, only kyphotic angle progressed in the presence of disc injury and vertebral compression did not.
For the fractures induced by axial compression, vertebral body deformation may be the result of trabecular bone impaction [29]. In addition, for thoracolumbar fractures a low signal intensity lesion on T2 weighted images has been reported to coincide with the site of trabecular bone impaction visualized as hematoma by CT [27]. Accordingly, low signal intensity lesions on T2 weighted images are presumed to importantly promote the later progression of vertebral body compression. In the present study, wedge angle and anterior vertebral compression were observed to increase significantly in such cases. Kyphotic angle also increased by an average of 3.8°, that is, kyphotic angle increased by an average of 1.1° more than in those not exhibiting low signal intensity lesion, although this was not statistically significant. We consider that this is because total spine sagittal alignment was partly recovered by hyperextension of the disc space in some patient groups, when sagittal imbalance appeared to be due to the progression of wedge angle and anterior vertebral compression.
PL injury, inferior endplate disruption, and inferior disc injury did not show any meaningful correlation with the progressions of kyphotic deformity or vertebral compression. We believe these findings were due to the retrospective nature of the study, the exclusion of surgically treated patients, which led to the inclusion of only 12 patients with PL injury, because most patients with PL injury also had posterior ligament complex injury, and to the inclusion of only 3 and 4 patients with inferior endplate disruption and disc injury, respectively, because both are usually associated with unstable fractures. In addition, we did not investigate relations between radiological factors, which are related to the progression of kyphotic deformity and clinical functional outcomes, age, brace compliance, or bone density.
Conclusions
The study shows that when anterior longitudinal ligament injury, superior endplate and disc injury, or a high level of edema are depicted by MRI, the risk of kyphotic deformity is enhanced even for stable thoracolumbar fractures. In particular, a bone edema level of over 2/3 is a more critical factor in determining kyphotic deformity progression. Therefore, more positive follow-ups and treatments are required in such cases.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.