Cervical Radiculopathy Focus on Characteristics and Differential Diagnosis
Article information
Abstract
Cervical radiculopathy is characterized by neurological dysfunction caused by compression and inflammation of the spinal nerves or nerve roots of the cervical spine. It mainly presents with neck and arm pain, sensory loss, motor dysfunction, and reflex changes according to the dermatomal distribution. The most common causes of cervical radiculopathy are cervical disc herniation and cervical spondylosis. It is important to find the exact symptomatic segment and distinguish between conditions that may mimic certain cervical radicular compression syndromes through meticulous physical examinations and precise reading of radiographs. Non-surgical treatments are recommended as an initial management. Surgery is applicable to patients with intractable or persistent pain despite sufficient conservative management or with severe or progressive neurological deficits. Cervical radiculopathy is treated surgically by anterior and/or posterior approaches. The appropriate choice of surgical treatment should be individualized, considering the patient’s main pathophysiology, specific clinical symptoms and radiographic findings thoroughly.
Introduction
Cervical radiculopathy is characterized by neurological dysfunction caused by compression and inflammation of the spinal nerves or nerve roots of the cervical spine. The incidence and prevalence rate of cervical radiculopathy are unclear, and epidemiological data are limited. In a large-scale retrospective population-based study, the incidence rate was 83.2 per 100,000 people (107.3 men and 63.5 women), with the peak incidence in the fifth decade [1]. A recent US military study found an incidence of 1.79 per 1,000 person-years [2].
Depending on the segments involved and severity of neurological dysfunction, various signs and symptoms of cervical radiculopathy may manifest as neck and unilateral arm pain with numbness, weakness, or altered reflexes [3]. It is important to find the exact symptomatic segment and distinguish between conditions that may mimic certain cervical radicular compression syndromes through various provocation physical examinations and radiographs. Conservative or surgical treatments may be considered to reduce pain, improve neurological function, prevent recurrence, and allow the patient to return to daily life. In this review article, we address the pathophysiology, characteristics, differential diagnosis, and treatment options for cervical radiculopathy.
Pathophysiology
Cervical radiculopathy is the pathological process associated with the cervical spinal nerve or nerve root compression and inflammation. The most common causes of cervical radiculopathy are cervical disc herniation and cervical spondylosis.
Disc herniation is more commonly associated with lumbar radiculopathy than with cervical radiculopathy. Disc herniation is responsible for only 21.9% of cervical radiculopathy cases [1]. Cervical spondylosis refers to degenerative changes that result from aging in most adult populations. Disc degeneration with age leads to decreased disc height and foraminal narrowing. Decreased disc height causes the increased loads to the vertebral body and the intervertebral joints of Luschka (uncovertebral joints). This leads to osteophyte formation and bony hypertrophy. Hypertrophy of the uncovertebral and facet joints can cause foraminal stenosis and cervical radiculopathy [4,5].
Cervical radiculopathy is less commonly caused by tumors, trauma, synovial cysts, meningeal cysts, dural arteriovenous fistulae [6], or tortuous vertebral arteries [7]. It mainly presents with neck and arm pain, sensory loss, motor dysfunction, and reflex changes according to the dermatomal distribution.
Characteristics
1. Clinical diagnosis
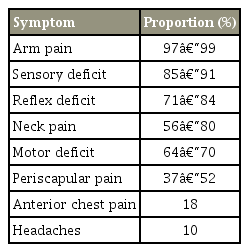
There are no universally accepted criteria for diagnosing of cervical radiculopathy. Generally, cervical radiculopathy patients have various signs and symptoms, such as neck and unilateral arm pain with numbness, weakness, or altered reflexes [3]. The main signs and symptoms of patients are arm pain in 97%–99%, sensory deficit in 85%–91%, reflex deficit in 71%-84%, neck pain in 56%-80%, motor deficit in 64%–70%, scapular pain in 37%–52%, anterior chest pain in 18%, and headaches in 10% (Table 1) [8-10]. The clinical diagnosis can be made based on the patient’s medical history and physical examination [11]. The diagnosis is then verified by radiographs or supported by surgical results [12].
There are several provocative tests to evaluate cervical radiculopathy, but only a few of them have reliably yielded statistically significant differences between patients and controls in research setting. The Spurling test has been demonstrated to have low to moderate sensitivity (30%–50%) and moderate to high specificity (74%–93%), neck traction test showed moderate sensitivity (44%) and high specificity (90%–97%), and Valsalva’s maneuver showed low sensitivity (22%) and high specificity (94%). The upper limb tension test had high sensitivity (72%–97%) and low specificity (11%–33%), while the shoulder abduction test had low to moderate sensitivity (17%–78%) and moderate to high specificity (75%–92%) (Table 2) [13-17]. Positive results for two or more simultaneous provocation tests are considered to increase the accuracy of the diagnosis of cervical radiculopathy.
2. Imaging studies
Conventional radiographs are commonly obtained to evaluate cervical lesions, including fractures, tumors, degenerative pathologies, etc. Although their usefulness is limited due to low diagnostic sensitivity, conventional radiographs are considered as an important screening tool. In particular, oblique views of the cervical spine are used to assess the patency of the intervertebral foramina [18]. They are inexpensive, reproducible, and facilitatory in evaluating fractures, instability, and deformity.
Computed tomography (CT) helps assess pathologies that cause neural compression, such as bony spurs, foraminal stenosis, facet hypertrophy, and ossification of the posterior longitudinal ligament. The diagnostic accuracy of CT has been shown to be moderate to high (72%–91%) [19]. CT myelography is an invasive study that may be more effective in distinguishing soft tissue from bony pathology. When combined with myelography (CT myelography), the accuracy has been reported to increase to 96% [20-23].
Magnetic resonance imaging (MRI) is the most common imaging method for detecting cervical spine pathologies because it can detect cervical neural lesions directly and non-invasively [24]. Brown et al. [25] reported that MRI predicted 88% of cervical lesions. MRI can be combined with CT or CT myelography to improve diagnostic accuracy. Recently, the importance of oblique MRI views of in the cervical spine has been increasingly emphasized for the assessment of foraminal stenosis [26,27] (Fig. 1).

A 53-year-old male patient’s radiographs of cervical spine. He complained severe left-side scapular medial border pain and weakness of left finger extension. Intervertebral disc space narrowing and posterior ostephytes were observed in multiple levels (A, yellow arrows) and large bony spur and foraminal stenosis were well presented at C6–7 segment of oblique X-ray (B, black arrow). The C6–7 and C7–T1 foraminal stenoses seems to be more clear in oblique coronal images of magnetic resonance imaging (C) than in axial computed tomography scans or magnetic resonance images (D).
3. Electrodiagnostic studies
Electrodiagnostic studies are useful for distinguishing cervical radiculopathy from other lesions that are not clear on physical examination. Electromyography (EMG) analyzes multiple muscles within the same myotome and in adjacent myotomes. Nerve conduction studies (NCS) are conducted to exclude peripheral neuropathy and measure amplitude, distal latency, and conduction velocity.
Abnormal findings, including positive sharp waves and fibrillation potentials, may not occur within 3 weeks of the onset of nerve compression [28]. EMG results may not be abnormal in the presence of mild radiculopathy or primarily sensory radiculopathy, and they are likely to be benign in patients without pronounced weakness. The efficacy of EMG as a tool to diagnose cervical radiculopathy accurately is estimated to be 57% to 90% [29-33]. Nardin et al. [31] retrospectively studied 47 patients with cervical and lumbar radiculopathy who were assessed by both EMG and spine MRI studies. They found that 55% of patients had EMG abnormalities and 57% had MRI abnormalities related to the clinically estimated level of radiculopathy. The modalities were concordant for the majority (60%) of patients, with findings of both normal for 11 and both abnormal for 17. However, the modalities were discordant in a significant minority (40%), suggesting that both EMG and MRI remain complementary diagnostic tools [31]. Therefore, EMG and NCS should be considered as supportive tools for a more accurate diagnosis of cervical radiculopathy and should not be considered definitive on their own.
Differential Diagnosis
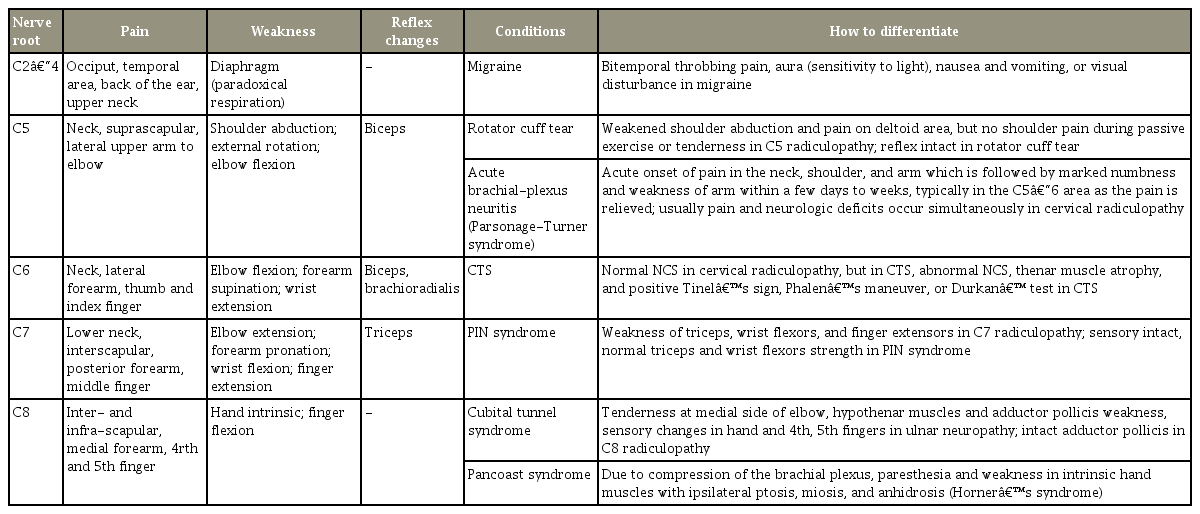
The expression of the patient’s symptoms is determined by the level at which the cervical nerve root is compressed. According to the previous literatures, peri-scapular pain also showed dermatomal distributions of lower cervical spinal nerves [34,35] (Fig. 2). It is important to distinguish between conditions that may mimic certain cervical radicular compression syndromes.
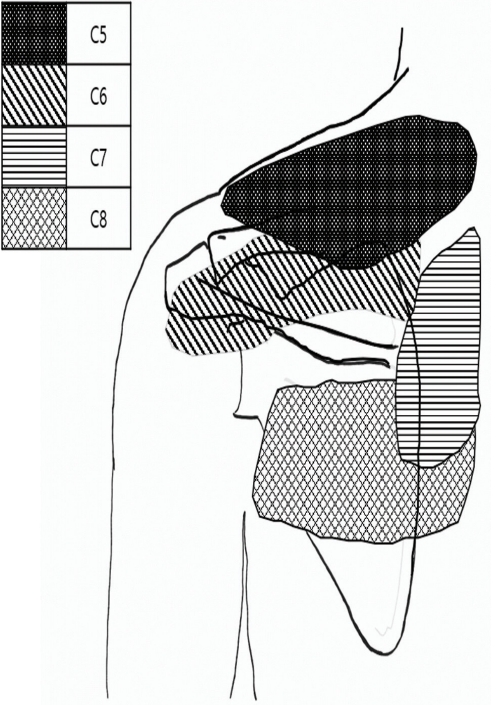
Differential diagnosis of peri-scapular pain in according to the dermatomal distribution of lower cervical spinal nerves. Pain on supra-scapular areas are associated with C5 or C6 radiculopathies, interscapular and infra-scapular pains are considered to be mainly from C7 and C8 radiculpathy, respectively.
C2–4 radiculopathy is not common. Patients often complain of occipital or temporal pain that extends to the back of the ear or side of the neck. This is difficult to distinguish from other causes of headache such as migraine [36]. Motor deficits generally may be hard to detect. The C3 and C4 nerve roots innervate the diaphragm, and these cervical radiculopathies can lead to diaphragmatic weakness and a pattern of breathing referred to as paradoxical respiration [37,38].
C5 radiculopathy leads to symptoms similar to that of a rotator cuff tear. While both can cause weakened shoulder abduction, C5 radiculopathy is not associated with shoulder pain during passive exercise or tenderness.
Carpal tunnel syndrome (CTS) mimics C6 radiculopathy. A patient with C6 radiculopathy usually feels pain or numbness from the neck to radial side of the biceps, forearm, the dorsal web space of the hand between the thumb and index finger, and to the tips of those fingers. However, CTS usually involves the radial three and a half digits and is manifested by thenar muscle atrophy. Tinel’s sign, Phalen’s maneuver, or Durkan’s test may be positive in patients with the CTS. Motor deficits of the wrist extensors and biceps are common in association with C6 radiculopathy. The brachioradialis and biceps reflexes may be changed.
The C7 nerve root is the most frequently involved by cervical radiculopathy. Entrapment of the posterior interosseous nerve may be mistaken for the motor component of the C7 radiculopathy causing weakness of triceps, wrist flexors and finger extensors. However, sensory changes are absent, and the triceps and wrist flexors have normal strength in posterior interosseous neuropathy. Usually, when patients explain their symptoms, patients with C6 radiculopathy or CTS show the volar side of their hands, but patients with C7 radiculopathy often express symptoms by pronating the forearms.
Additionally, ulnar entrapment at the level of the elbow (cubital tunnel syndrome) can cause clinical tenderness along the medial side of the elbow and hypothenar muscles, as well as adductor pollicis weakness, sensory changes in the hand and fourth and fifth fingers. Patients with C8 radiculopathy complain of profound weakness of the intrinsic hand muscles and difficulty using their hands in daily life [4,39-42] (Table 3).
Natural History
Lee and Turner reported that the natural history of cervical radiculopathy was generally favorable and self-limited. In mid- to long-term follow-up (2 to 19 years) of 51 patients with radiculopathy, 43.1% had no symptoms, 29.4% had mild or intermittent symptoms, and only 27.5% had persistent or worsening symptoms. Progressive neurologic deficits or myelopathic symptoms did not develop in any of radiculopathy patients at follow-up [43]. Significant improvement in pain and disability tends to occur within 4 to 6 months after onset. Eighty-three percent of patients took 2 to 3 years to fully recover and 22% had moderate pain recurrence 2 to 3 years, but not as severe as the initial pain onset [44,45]. Since the natural history of cervical radiculopathy often appears to be favorable in spite of soft disc herniation or osteophyte [46], conservative treatment is considered as the initial treatment of choice for most cases without progressive neurologic deficit or debilitating pain.
Treatment Options
1. Conservative treatment
The goals of treatment are to reduce pain, improve neurological function, prevent recurrences, and allow the patient to return to daily life. Initially, non-surgical treatments, such as immobilization (cervical collar), traction, massage, oral medication, physical therapy, cervical manipulation, and cervical steroid injection, are recommended. In the literatures, high-quality evidences for the effectiveness of these conservative treatments are lacking, and these are considered for symptomatic relief only [9]. There have been no randomized controlled trials (RCTs) supporting the use of immobilization, traction, and massage for patients with cervical radiculopathy, and oral medication use is also supported by limited evidence, except for the short-term use of oral corticosteroids [47]. Meanwhile, some cohort studies and RCTs have demonstrated significant benefits yielded by supervised and home-based physical therapy [48-50], but the efficacy of cervical manipulation for radiculopathy is not supported by sufficient evidence.
Cervical steroid injections can be considered for patients who do not respond to 4 to 6 weeks of other conservative management options. There is high-quality evidence supporting the use of cervical steroid injections for cervical radiculopathy caused by disc herniation, but fair evidence for spondylosis [51]. Although such injections are considered to be relatively safe, there are concerns about complications, such as dural puncture, epidural hematoma, nerve root injury, or cord infarction [46,52,53].
2. Surgical treatment
Surgery is applicable to patients with intractable or persistent pain despite sufficient conservative management for at least 6 to 12 weeks or to patients with severe or progressive neurological deficits. Cervical radiculopathy is treated surgically by anterior or posterior approaches [54]. For patients with cervical kyphosis [55], anterior procedures including cervical discectomy, corpectomy and cervical disc arthroplasty (CDA) are generally preferred by using bones, cages, and plates.
1) Anterior cervical discectomy and fusion
Anterior cervical discectomy and fusion (ACDF) is the most commonly performed procedure for cervical radiculopathy. It involves removing all disc material anteriorly from the uncinate process to adjacent uncinate process following placement of bone grafts or cages to maintain cervical disc height and prevent kyphosis resulting in indirect foraminal decompression. As a result, 87.8% of the patients were functionally and neurologically satisfied with results following ACDF. However, ACDF is known to be associated with complications, such as dysphagia, hoarseness, airway obstruction, hardware failure, nonunion, and adjacent segmental degeneration (ASD). Hilibrand and Robbins [56] described ASD as radiographic degeneration at the level adjacent to the previous fusion leading to new neurological sequelae. The expected incidence of new symptomatic adjacent-level disease increases by about 2.9% annually after fusion and is 25.6% at postoperative 10 years [57], but it is unclear whether ASD reflects the natural history of cervical spondylosis or is the consequence of cervical spinal fusion. Despite the risk of complications, ACDF is still considered the “gold standard” for cervical radiculopathy treatment in 1, 2, or 3 levels.
2) Cervical disc arthroplasty
CDA is performed through an approach similar to that of ACDF, but a prosthesis is placed in the decompressed disc space instead of graft materials. The advantages of CDA include the avoidance of nonunion and the prevention of ASD by motion preservation. Since the advent of CDA, many studies have shown that there is not much difference between the ACDF and CDA groups in terms of outcomes [58,59]. However, more recently, CDA was formally approved by the U.S. Food and Drug Administration for single- and two-level cervical degenerative disc disease [60]. Several reviews have concluded that CDA is superior to ACDF in long-term clinical success rates and better functional outcome measurements [61,62]. Until now, some controversial issues still remain unresolved, including surgical outcomes, ASD, heterotopic ossification, wear debris, and multi-level CDA. It is too early to draw definitive conclusions about the efficacy and costeffectiveness of CDA; such clarity will require further well-designed research and considerable time [63].
3) Posterior cervical foraminotomy
If the cervical lordosis is preserved without spinal cord compression, posterior cervical foraminotomy (PCF) can be considered for cervical radiculopathy. Since the 1940s, when the PCF was introduced, development of the technique has been remarkable, particularly in recent years. PCF has the advantages of avoiding fusion, preserving motion and preventing of ASD [64,65]. The main issues associated with complication after PCF are symptom recurrence at the surgical segment due to incomplete decompression, degeneration of the index level, and nerve root injury. In the literatures, the surgical outcomes of PCF generally reported as favorable. With a mean follow-up of 10 years, Church et al. [66] reported satisfactory surgical results in approximately 90% of their study patients, and 93% of patients were able to return to work. The recurrence of radiculopathy requiring reoperation was only 6.2% and the overall complication rate in this study was only 3.3% [66]. In terms of pain improvement, complications, and quality of life, short- and long-term postoperative outcomes of PCF are almost similar to those of ACDF [67,68]. For the appropriate indications, PCF is considered an important treatment with considerable merits, particularly for patients with multi-level radiculopathy or previous anterior operations [8,69,70] (Fig. 3, Table 4).
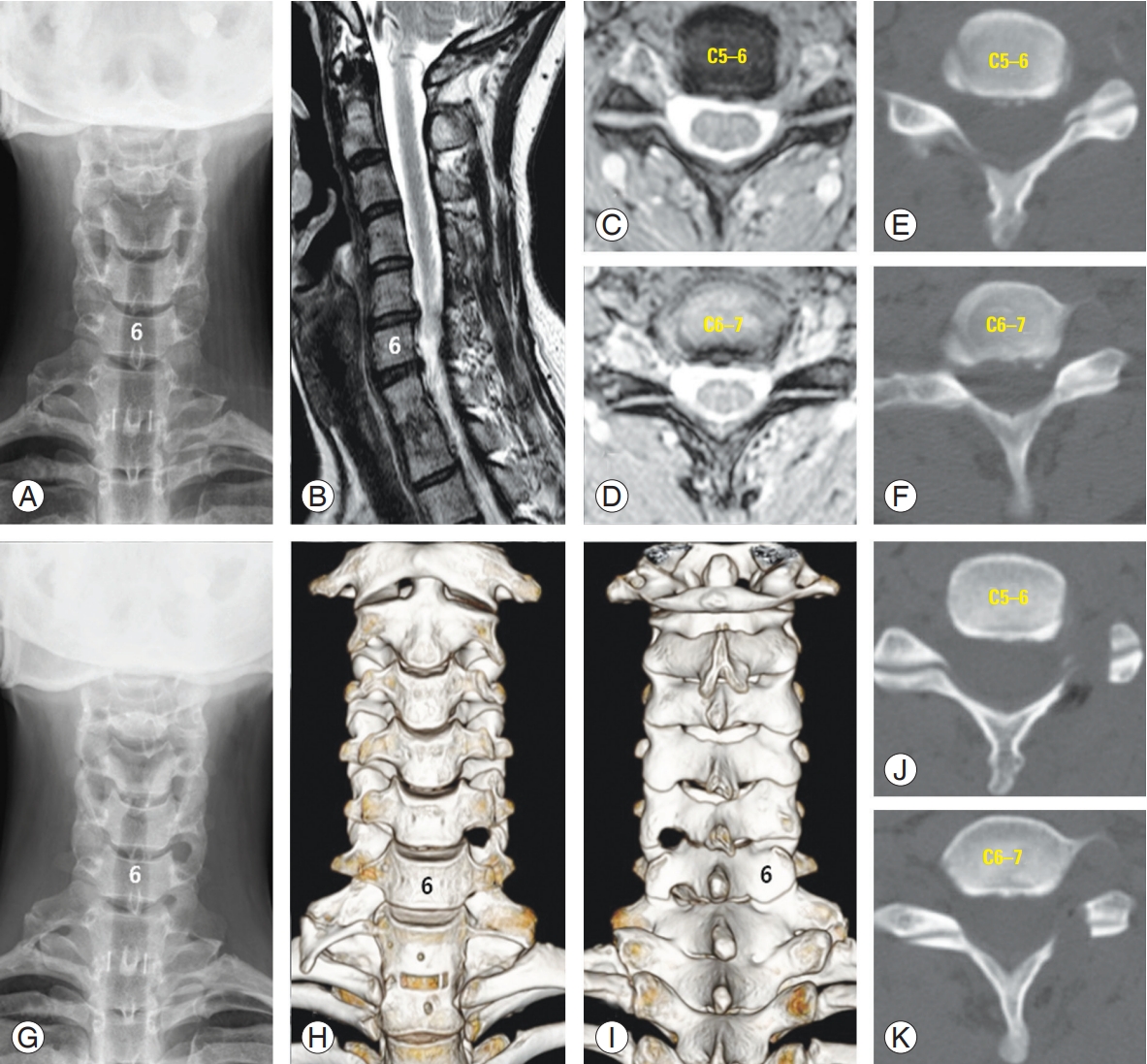
A 43-year-old right hand dominant female with a previous history of C7–T1 anterior cervical discectomy and fusion presented with significant pain on posterior neck, left side of supra-scapular area, radial side arm and 1st & 2nd fingers. (A) Plain radiograph of cervical spine showed the prior C7–T1 fusion. Magnetic resonance imaging (B) and CT revealed disc protrusion and foraminal stenosis at the left-side of C5–6 (C, E) and C6–7 (D, F) segments. The patient underwent left C5–6 and C6–7 PCF. The postoperative plain radiograph (G) and CT (H, I) showed the left-side PCF state on C5–6 (J) and C6–7 (K). After surgery, her radicular symptom was completely resolved. CT, computed tomography; PCF, posterior cervical foraminotomy.
Conclusions
Cervical radiculopathy often causes neck and arm pain as a result of disc herniation or cervical spondylosis. Thorough medical history taking and physical examination, along with radiographic and electrodiagnostic studies can help identify pathologies and exclude other causes of upper limb dysfunction. Cervical radiculopathy is initially treated conservatively. When the patient suffers from intractable pain or progressive neurology, operative treatment can be considered. Either anterior or posterior approaches should be determined under appropriate circumstances, understanding that each technique has its own advantages and disadvantages.
Notes
No potential conflict of interest relevant to this article was reported.