The Effect of Discharging Patients with Low Hemoglobin Levels on Hospital Readmission and Quality of Life after Adult Spinal Deformity Surgery
Article information
Abstract
Study Design
Retrospective cohort.
Purpose
This study aims to evaluate the impact of anemia on functional outcomes, health-related quality of life (HRQoL), and early hospital readmission (EHR) rates after adult spinal deformity (ASD) surgery at the time of discharge from the hospital.
Overview of Literature
Concerns with risks of transfusion, insufficient evidence for its benefits, and the possibility of associated adverse outcomes have led to restrictive transfusion practices. Therefore, patients are discharged according to patient blood management programs that are implemented in hospitals nationwide to reduce unnecessary blood transfusions. However, not many comprehensive kinds of studies exist on the effect of postoperative anemia on functional life and complications.
Methods
Anemia severity was defined following the 2011 World Health Organization guidelines. All patients had HRQoL tests as well as complete blood counts pre- and postoperatively. EHR is the admission within 30 days of discharge and was used as the dependent parameter.
Results
This study comprised 225 surgically treated ASD patients with a median age of 62.0 years, predominantly women (80%). Of the 225 patients, 82, 137, and six had mild, moderate, and severe anemia at the time of discharge, respectively. Seventeen of the patients (mild [11, 64.7%]; moderate [5, 29.4%]; severe [1, 5.9%]) were readmitted within 30 days. The mean hemoglobin values were higher in readmitted patients (p=0.071). Infection was the leading cause of readmission (n=12), but a low hemoglobin level was not observed in any of these patients at the time of discharge. Except for Scoliosis Research Society-22 questionnaire, HRQoL improvements did not reach statistical significance in early readmitted patients in the first year after surgery.
Conclusions
The results of this study demonstrated that the occurrence and the severity of postoperative anemia are not associated with EHR in surgically treated patients with ASD. The findings of the current research suggested that clinical awareness of the parameters other than postoperative anemia may be crucial. Thus, improvements in HRQoL scores were poor in early readmitted patients 1 year after surgery.
Introduction
The circulatory and hematopoietic systems have evolved to bridge the gap between the outside world, where resources are plentiful, and the immediate vicinity of the cells. Any condition compromising this long and tightly regulated chain of supply can result in significant harm. Anemia, the oxygen-carrying capacity of the blood, and its rheological characteristics are compromised in one such condition [1,2].
Nature does not necessarily comply with the human desire to often categorize using arbitrary criteria. Anemia is a good example because the search for the physiologic hemoglobin (Hb) threshold to define anemia remains unfulfilled [3].
Anemia has been associated with increased mortality, higher incidence of cardiovascular disease, cognitive impairment, and increased risk of falls and fractures [4,5]. Major surgeries, e.g., adult spinal deformity (ASD) surgery, are associated with significant blood loss, and often result in postoperative anemia [6]. Concerns with risks of transfusion, insufficient evidence for its benefits, and the possibility of associated adverse outcomes have led to restrictive transfusion practices. Therefore, patients are discharged according to patient blood management programs that are implemented in hospitals nationwide to reduce unnecessary blood transfusions [2,7]. Moreover, patients undergoing spinal deformity surgery are asked to ambulate as soon as possible. This circumstance increases metabolic demand. Moreover, anemia could also affect functional recovery after major orthopedic surgery by decreasing postoperative vigor and quality of life (QoL) [8,9].
Evident literature is insufficient to demonstrate whether low Hb values at discharge may affect readmission rates and functional outcomes after ASD surgery. Thus, this study aims to identify the impact of anemia on QoL and early hospital readmission (EHR) rates from any cause after ASD surgery.
Materials and Methods
This retrospective study was conducted on a prospectively collected multicenter ASD database. The criteria for database inclusion were defined as having any or any combination of thoracic kyphosis exceeding 60°, coronal deformity exceeding 20°, pelvic tilt exceeding 25°, and sagittal vertical axis exceeding 50 mm. All patients were enrolled into an institutional review board-approved protocol in the respective sites. This study was approved by the Clinical Research Ethics Committee of Vall d’Hebron University (approval no., 181-10/2010). Moreover, the patients consented to be enrolled in the database as well as in the present study. Baseline demographic data (age, gender, comorbidities, and body mass index), health-related QoL (HRQoL) parameters (The Core Outcome Measures Index, The Oswestry Disability Index [ODI], 36-item Short-Form Health Survey [SF-36] mental component summary, SF-36 physical component summary [PCS], and Scoliosis Research Society-22 questionnaire [SRS-22]), and radiological features (sagittal vertical axis, T2–T12 kyphosis, coronal balance, major curve Cobb angle, lordosis gap [10], global tilt [11], and T1 sagittal tilt [12]) were included. Patients were also stratified according to the etiology of their deformity (i.e., idiopathic, degenerative, and others). Demographical, clinical, and radiological characteristics and HRQoL parameters at baseline and 1 year postsurgery were extracted. Reports of research followed the principles of the Declaration of Helsinki.
1. Hemoglobin evaluation
Anemia severity was defined following the 2011 World Health Organization (WHO) guidelines [3]. The WHO defined three levels according to Hb concentrations, i.e., mild (11–11.9 g/dL in adult females; 11–12.9 g/dL in adult males), moderate (8–10.9 g/dL in adult females or males), and severe (<8 g/dL in either gender). Patients who had complete blood counts at the latest time during hospitalization for surgery or at the time of discharge were assessed.
2. Readmission
EHR, defined as the readmission within 30 days of discharge, was used as the dependent parameter because the more time that passes between readmission and discharge, the less likely it is to be associated with a negative condition at discharge [13].
3. Statistical analysis
Nonparametric test statistics were used to evaluate the relationship between variables. Spearman’s rho correlation coefficient was used to test the correlation between continuous variables. The Mann-Whitney U-test and the Kruskal-Wallis test were used to compare two and more than two groups, respectively, according to Hb values. Linear regression was used to predict Hb level for gender categories. Furthermore, dummy coding was used to take gender as an independent variable. The type-I error rate was taken as α=0.05 for statistical significance. IBM SPSS for Windows ver. 21.0 (released 2012; IBM Corp., Armonk, NY, USA) was used for analyses.
Results
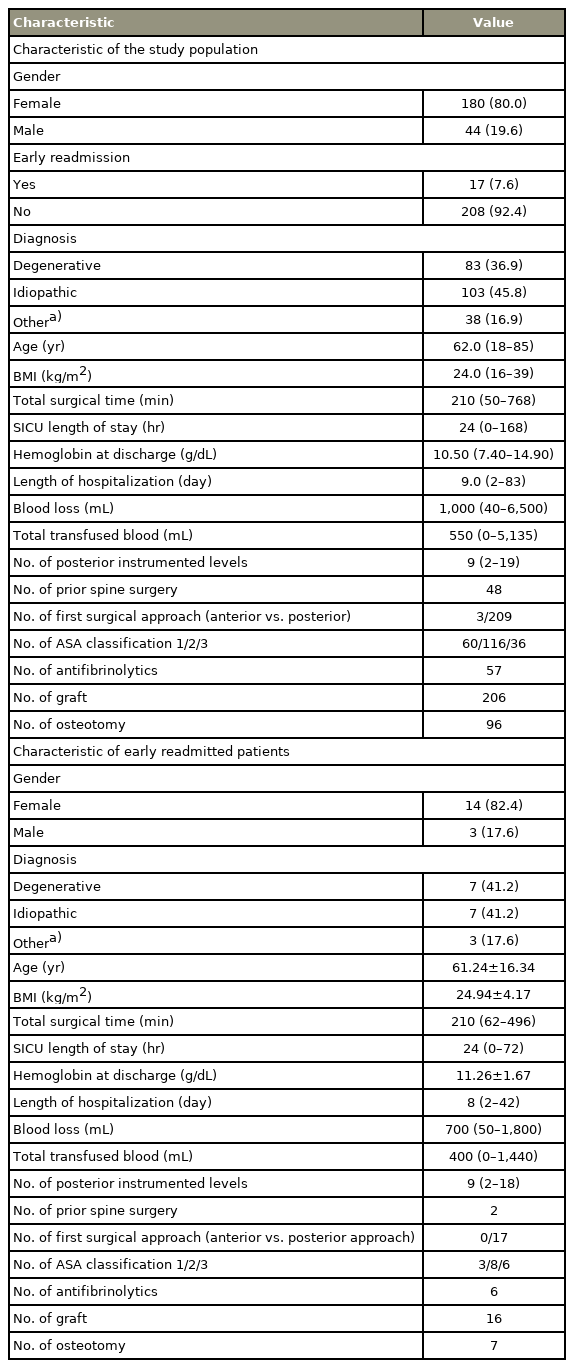
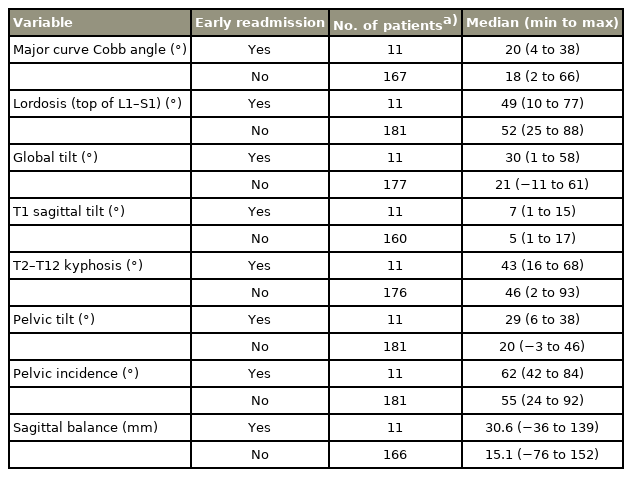
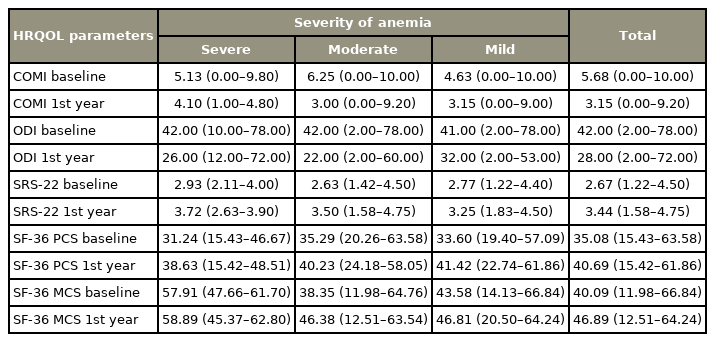
This study comprised 225 surgically treated ASD patients with a median age of 62.0 years, predominantly women (80%). Of the 225 patients, 82, 237, and six had mild, moderate, and severe anemia at the time of discharge, respectively. Of these, 17 patients (mild [11, 64.7%]; moderate [5, 29.4%]; severe [1, 5.9%]) were readmitted within 30 days. The mean Hb values at discharge were higher in readmitted patients (p=0.071). Demographical, radiological, and surgical characteristics of the study population, early readmitted patients, mean Hb values of the patients at discharge, and comparison among groups are detailed in Tables 1–5. In univariate analysis, only gender was found to be a statistically significant variable. Moreover, the linear regression model, including gender, showed that higher levels of Hb were associated with the male gender (p=0.017) (Table 6). Furthermore, infection was the leading cause of readmission (n=12), followed by neurological deficit (n=6), severe back pain (n=3), pleural effusion (n=1), hematoma (n=1), radicular pain (n=1), and implant (screw) failure (n=1). Statistically significant improvements were discovered in HRQoL parameters using ODI, SF-36 PCS, and SRS-22 1 year postsurgery for the entire study population (p<0.001). However, except for SRS-22, HRQoL improvements did not reach statistical significance in early readmitted patients in the first year of postsurgery (Table 7).
Discussion
The results of this study demonstrated that low Hb values at discharge did not have any impact on EHR rates in surgically treated patients with ASD. Moreover, it also showed that EHR was associated with poor improvements in QoL parameters within 1 year of postsurgery. The findings of the current research suggested that clinical awareness of the parameters other than anemia may be more important at the time of early readmission.
This study is a rare example evaluating the effect of “anemia at discharge” on QoL and EHR in patients who underwent major spinal surgery. The results are consistent with prior studies investigating the role of anemia in spinal surgery [14–16].
Anemia may be an adaptive response to illness and/or a marker of illness, and assessing the linkage between Hb concentration and treatment outcomes is difficult when more time elapses between the anemia duration and the event [17]. Nonetheless, this potentially harmful effect could be associated with increased 30-day hospital readmissions if postoperative anemia resulted in tissue hypoxia. The results of the current study did not show any association between the low Hb values at discharge, EHR from all causes, and readmissions. However, the sample size was relatively small. Cho et al. [18] and Shehata et al. [19] evaluated the patients undergoing major surgical procedures and found that discharge Hb concentration was not associated with 30-day readmissions. In contrast, Koch et al. [20], Muzarelli et al. [21], and Rubel et al. [22] demonstrated that postoperative low Hb levels markedly affect postoperative readmission rates.
Improving exercise tolerance and facilitating functional recovery during the rehabilitation period to have high Hb levels is recommended [8]. A patient with low Hb with good iron reserves may recover much faster than those with suboptimal iron reserves [23]. Thus, Halm et al. [2] concluded in a cohort study of 551 patients that transfusion after hip fracture surgery reduced the risk of readmission but did not decrease mortality or improve mobility. Postoperative intravenous iron administration found that its use significantly reduced the percentage of patients receiving a transfusion [24]. In addition, Jans et al. [25] reported that moderate anemia has no or only a negligible effect on early functional recovery after major orthopedic surgery. HRQoL parameters have become increasingly important in the evaluation of surgical outcomes in ASD. Moreover, the present study did not find any correlation between low Hb levels on discharge and HRQoL parameters in a relatively few patients (Table 8). When early readmitted patients were taken apart, only improvements in SRS-22 reached statistical significance, and the current findings suggested poor improvements in early readmitted patients usinf HRQoL parameters at 1-year follow-up.
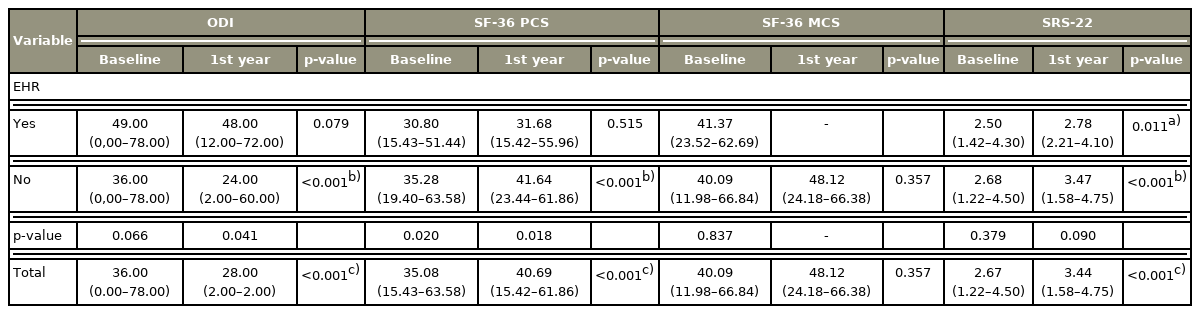
The comparison between baseline and one year follow-up scores of health-related quality of life parameters in surgically treated adult spinal deformity patients whether early readmitted to hospital or not
This study has several limitations inherent to its retrospective design and the associated possibility of bias. The occurrence and duration of anemia (how long a patient spent at a given Hb level; iron deficiency) is likely as important as or may be more important than the level of anemia. Any degree of preoperative anemia and the application of blood transfusion may be associated with increased length of hospital stay and EHR after controlling for other variables [14,26–28]. Moreover, valuable intraoperative characteristics such as the existence of acute blood loss, intra- or postoperative hypotension, and electrocardiographic changes may influence treatment outcomes [29,30]. The Hb level at discharge may only be a transient representation of the anemia severity. Iron studies may be a more reliable indicator of the anemia status. A patient with low Hb with good iron reserves may recover much faster than those with suboptimal iron reserves [24]. In addition, malnutrition in older patients is a significant predictor of readmission or mortality in both the very early and in the late periods following hospital discharge other than anemia [31,32]. As those parameters were unreachable through a multicenter database at the time of the present research, their effects that may have had beneficial scientific contributions were not evaluated. Furthermore, a small number of patients were discharged with severe anemia. Thus, the results do not necessarily indicate causality because of the possibility that anemia is a surrogate marker of intraoperative events or procedural complexity that eventually resulted in complications. Although 225 patients were included in the entire study sample, patients discharged with Hb values of 8 g/dL represented only 2.7% of the sample making the study underpowered in this sense (the achieved power of this study is 0.32 [rho=0.10, α=0.05] while taking 225 patients). The propensity score-matched analyses may have been affected by a relatively small sample size, which further highlights the need for validation of these findings in a larger sample.
Conclusions
The results of this study demonstrated that the occurrence and the severity of anemia at discharge are not associated with EHR in surgically treated patients with ASD. Although the number of the early readmitted patients was fairly low to perform any further statistical analysis, the findings of the current research suggested that clinical awareness of the parameters other than anemia may be more important at the time of early readmission. Thus, improvements in HRQoL scores were poor in early readmitted patients 1 year postsurgery. These consequences present the merit of future investigations with a more detailed and larger data set.
Notes
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conception and design: VN, SA, FSPG, EA; conception: FP, AA, IO, FK, European Spine Study Group; data acquisition: VN, AVC, FP, FSPG, AA, IO, FK, EA; analysis of data: SY; drafting of the manuscript: VN, SA, PA, EA; critical revision: VN, SA, EA; and obtaining funding, administrative support, supervision: European Spine Study Group.
Acknowledgements
European Spine Study Group is a clinical research group funded by a research grant from DePuy-Synthes.