Postoperative Increase in Occiput–C2 Angle Negatively Impacts Subaxial Lordosis after Occipito–Upper Cervical Posterior Fusion Surgery
Article information
Abstract
Study Design
Retrospective case series.
Purpose
To elucidate the impact of postoperative occiput–C2 (O–C2) angle change on subaxial cervical alignment.
Overview of Literature
In the case of occipito–upper cervical fixation surgery, it is recommended that the O–C2 angle should be set larger than the preoperative value postoperatively.
Methods
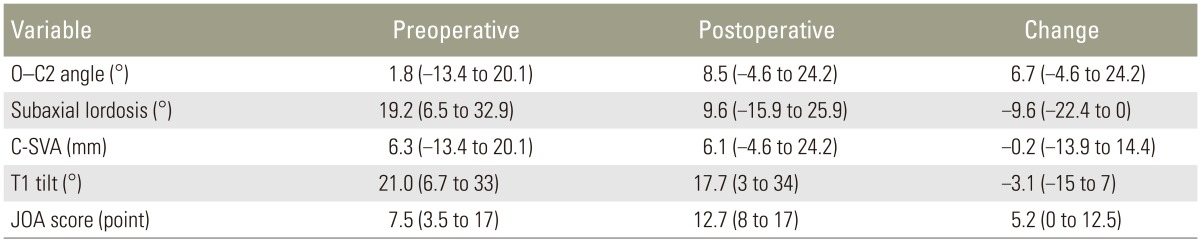
The present study included 17 patients who underwent occipito–upper cervical spine (above C4) posterior fixation surgery for atlantoaxial subluxation of various etiologies. Plain lateral cervical radiographs in a neutral position at standing were obtained and the O–C2 angle and subaxial lordosis angle (the angle between the endplates of the lowest instrumented vertebra (LIV) and C7 vertebrae) were measured preoperatively and postoperatively soon after surgery and ambulation and at the final follow-up visit.
Results
There was a significant negative correlation between the average postoperative alteration of O–C2 angle (DO–C2) and the average postoperative alteration of subaxial lordosis angle (Dsubaxial lordosis angle) (r=–0.47, p=0.03).
Conclusions
There was a negative correlation between DO–C2 and Dsubaxial lordosis angles. This suggests that decrease of mid-to lower-cervical lordosis acts as a compensatory mechanism for lordotic correction between the occiput and C2. In occipito-cervical fusion surgery, care must be taken to avoid excessive O–C2 angle correction because it might induce mid-to-lower cervical compensatory decrease of lordosis.
Introduction
Occipito–upper cervical posterior fusion surgery using an occipital plate and screw–rod system provides rigid and secure fixation for various kinds of lesions with clinical instabilities around the craniocervical junction [1]. In the case of occipito–upper cervical fixation surgery, caution should be paid to avoid an inadequate fixation angle between the occiput and upper cervical spine, because an inadequate angle can cause dysphagia and respiratory disturbance [2]. It is recommended that the occiput–C2 (O–C2) angle, which is the angle between the McGregor line and the lower endplate of C2 vertebra, should be set larger than the preoperative value postoperatively. In other words, postoperative alignment between the occiput and upper cervical spine should be more lordotic to avoid dysphagia and respiratory disturbance [3]. It is not clear how the alteration of the O–C2 angle affects subaxial cervical spine alignment.
The aim of the present study was to elucidate the impact of postoperative O–C2 angle change on subaxial cervical alignment.
Materials and Methods
The present study included 17 patients who underwent occipito–upper cervical spine (above C4) posterior fixation surgery for atlantoaxial subluxation of various etiologies in our institute from May 2000 to November 2012. The present case series included 8 male and 9 female patients; the average age at surgery was 55.7-year-old (range, 16–84 years). The average follow-up period was 67.2 months (range, 5–126 months). The clinical diagnosis was upper cervical anomaly in 7 cases, rheumatoid arthritis in 4 cases, atlantoaxial subluxation in 4 cases, Down syndrome in 1 case, and pseudarthrosis after dens fracture in 1 case. The fusion level was O–C2 in 8 cases, O–C3 in 5 cases, and O–C4 in 4 cases (Table 1). If the C2 pedicle screw could not insert because of high-riding vertebral artery or there was obvious osteoporosis, the fusion level was extended to caudally. Surgery was performed in the neutral position using a Mayfield skull cramp or Halo-vest. After insertion of screws and occiput plate, alignment was adjusted to extension position and the skull was sagittally rotated to obtain appropriate O–C2 angle and upper cervical alignment.
Recovery rate (Hirabayashi) and change in Japanese Orthopedic Association (JOA) score were assessed as clinical outcome measures. Perioperative complications were assessed using clinical records.
Plain lateral cervical radiographs in a neutral position at standing were obtained and the O–C2 and subaxial lordosis angles were measured preoperatively and postoperatively soon after surgery and ambulation and at the final follow-up visit. The O–C2 angle was measured as the angle between the McGregor line and lower endplate of the C2 vertebra [45]. A positive value indicates lordosis between the occiput and C2, and a negative value indicates kyphosis between the occiput and C2. The subaxial lordosis angle was defined as the angle between the endplates of the lowest instrumented vertebra (LIV) and C7 vertebrae, an indicator of cervical spine alignment. A positive value indicates lordosis between LIV and C7, and a negative value indicates kyphosis between LIV and C7. Change of the O–C2 angle was defined as DO–C2 and change of the subaxial lordosis angle was defined as Dsubaxial lordosis. A positive value in DO–C2 and Dsubaxial lordosis angles indicates increase of lordosis, and negative value in DO–C2 and Dsubaxial lordosis angles indicates decrease of lordosis. The cervical sagittal vertical axis (C-SVA) was measured as the deviation of the center of gravity head–plumb line (extending from the anterior margin of the external auditory canal) from the posterior superior endplate of C7. T1 tilt was measured as the angle between the superior endplate of T1 and horizontal line [45].
Preoperative and postoperative O–C2 angle, subaxial lordosis angle, C-SVA, and T1 tilt at final follow-up were compared using a Tukey–Kramer honestly significant difference (HSD) test. DO–C2 and D subaxial lordosis angle correlation was determined using Pearson's correlation coefficient. A p<0.05 was considered significant.
Results
The average JOA score was 7.2 points preoperatively and 11.4 postoperatively, showing a change of 4.2 points and 43% recovery. Perioperative complications included postoperative reintubation in one case, cerebellum hemorrhage in 1 case, and dysphagia in 2 cases.
There was significant difference between preoperative and postoperative subaxial lordosis angle, and postoperative and final follow-up subaxial lordosis angle (p=0.04, respectively) (Table 2). The average DO–C2 angle was 6.7°±4.0° and the average Dsubaxial lordosis angle was –9.5°±6.4°. There was a significant negative correlation between DO–C2 and Dsubaxial lordosis angles (r=–0.47, p=0.03) (Figs. 1, 2).
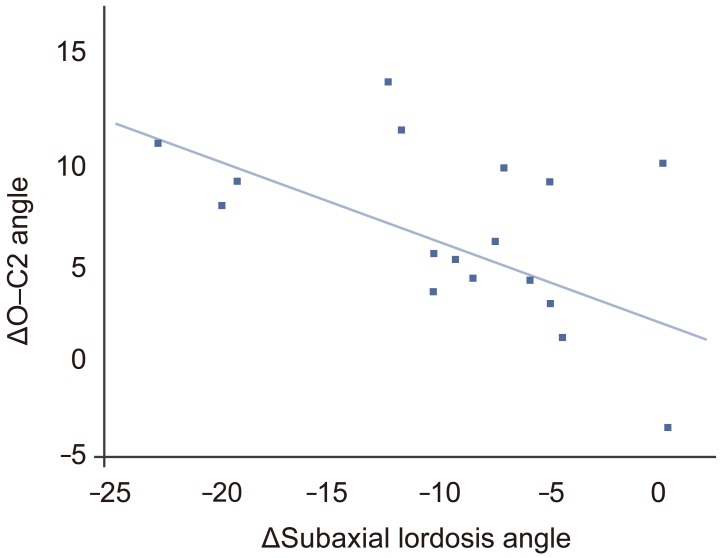
Relationship between the change of the O–C2 angle (DO–C2 angle) and change of the subaxial lordsis angle (Dsubaxial lordosis angle). There was a significant negative correlation between DO–C2 and Dsubaxial lordosis angles (r=-0.47, p=0.03). O–C2, occiput–C2.
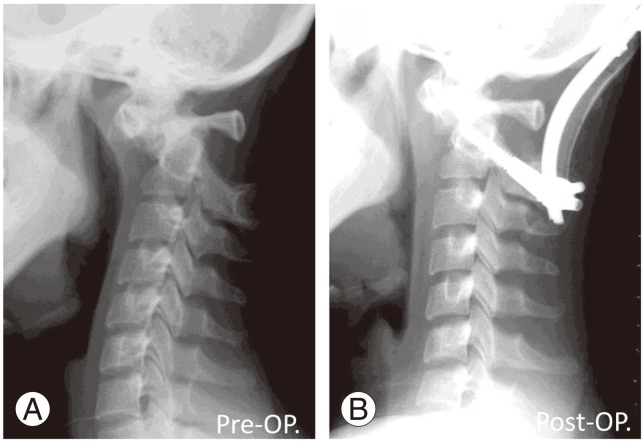
Representative case involving a 17-year-old female with atlanto-axial subluxation due to Down's syndrome. Preoperative X-ray shows irreducible atlanto-axial subluxation (A). After O–C2 fusion surgery, increase of O–C2 angle and decrease of subaxial lordosis was observed (B). O–C2 angle was –13° preoperatively and –2° postoperatively. C2–7 angle was 9° preoperatively and –11° postoperatively. O–C2, occiput–C2; Pre–OP, preoperative; Post–OP, postoperative.
The average C-SVA was 6.3±14.3 mm preoperatively, 6.1±12.6 mm postoperatively and 7.2±11 mm at final follow-up. The average T1 tilt was 21.0°±7.1° preoperatively, 17.7°±7.5° postoperatively, and 19.7°±10.4° at final follow-up visit. There was no significant difference between preoperative, postoperative, and final follow-up C–SVA and T1 tilt (Table 2).
Discussion
The present results demonstrate a negative correlation between DO–C2 and Dsubaxial lordosis angles. This suggests that decrease of mid- to lower-cervical lordosis acts as a compensatory mechanism for lordotic correction between the occiput and C2. This compensatory alignment change occurred immediately after ambulation and was maintained for follow-up. To avoid dysphagia, it is strongly recommended to fuse the occiput–cervical spine in a lordotic alignment, in which the O–C2 angle is more positive than preoperatively [2].
There is a compensatory mechanism for spinal sagittal deformity to maintain horizontal gaze. For example, deformity of the thoracolumbar spine can induce cervical deformity [6]. Patients with a positive sagittal malalignment tend to compensate with abnormal cervical hyperlordosis to maintain a horizontal gaze, and surgical correction of the thoracolumbar sagittal malalignment results in attenuation of the cervical hyperlordosis via reciprocal change [7]. This spontaneous correction of cervical deformity after correction of global sagittal balance by lumbar pedicle subtraction osteotomy has been reported [8]. Corrective fusion surgery for marked cervical kyphosis results in attenuation of compensatory hyperlordosis of the thoracolumbar spine [9]. The present results are consistent with those compensatory mechanisms.
Incidentally, T1 tilt showed no apparent change after occipitocervical fusion surgery in the present case series. Presently, there was no significant change in C-SVA after surgery. These lines of evidence suggest that an increase in the O–C2 angle had no significant impact on the sagittal balance of the thoracolumbar spine and the compensatory mechanism for O–C2 angle change within the cervical spine. Guo et al. [10] reported negative correlation between O–C2 angle and C2–7 angle in asymptomatic population. Passias et al. [11] reported that O–C2 angle and subaxial lordosis angle negatively correlated preoperatively and postoperatively. Those previous reports showed that the compensatory mechanism between occiput-upper cervical region and aubaxial cervical spine.
In occipitocervical fusion surgery, care must be taken to avoid excessive O–C2 angle correction because it might induce mid-to-lower cervical compensatory decrease of lordosis. If there is preoperative kyphosis or anterior slip in the mid-to-lower cervical spine, excessive correction of the O–C2 angle (hyperlordosis) might lead to deterioration of mid-to-lower cervical spine alignment [12]. In the case of occipitocervical fusion in combination with cervical laminoplasty, postoperative mid-to-lower cervical alignment prediction is important because lordosis is essential for spinal cord decompression by laminoplasty. Therefore, excessive correction of the O–C2 angle might be avoided in such cases. Optimal correction of the O–C2 angle remains unclear. Further exploration is needed to clarify this issue.
Conclusions
Change of O–C2 angle negatively correlates with change of subaxial cervical lordosis in occipitocervical fusion surgery.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.