Single-Level Cervical Artificial Disc Replacement Compared with Cage Screw Implants: 2-Year Clinical and Radiological Outcomes Especially Adjacent Level Ossification
Article information
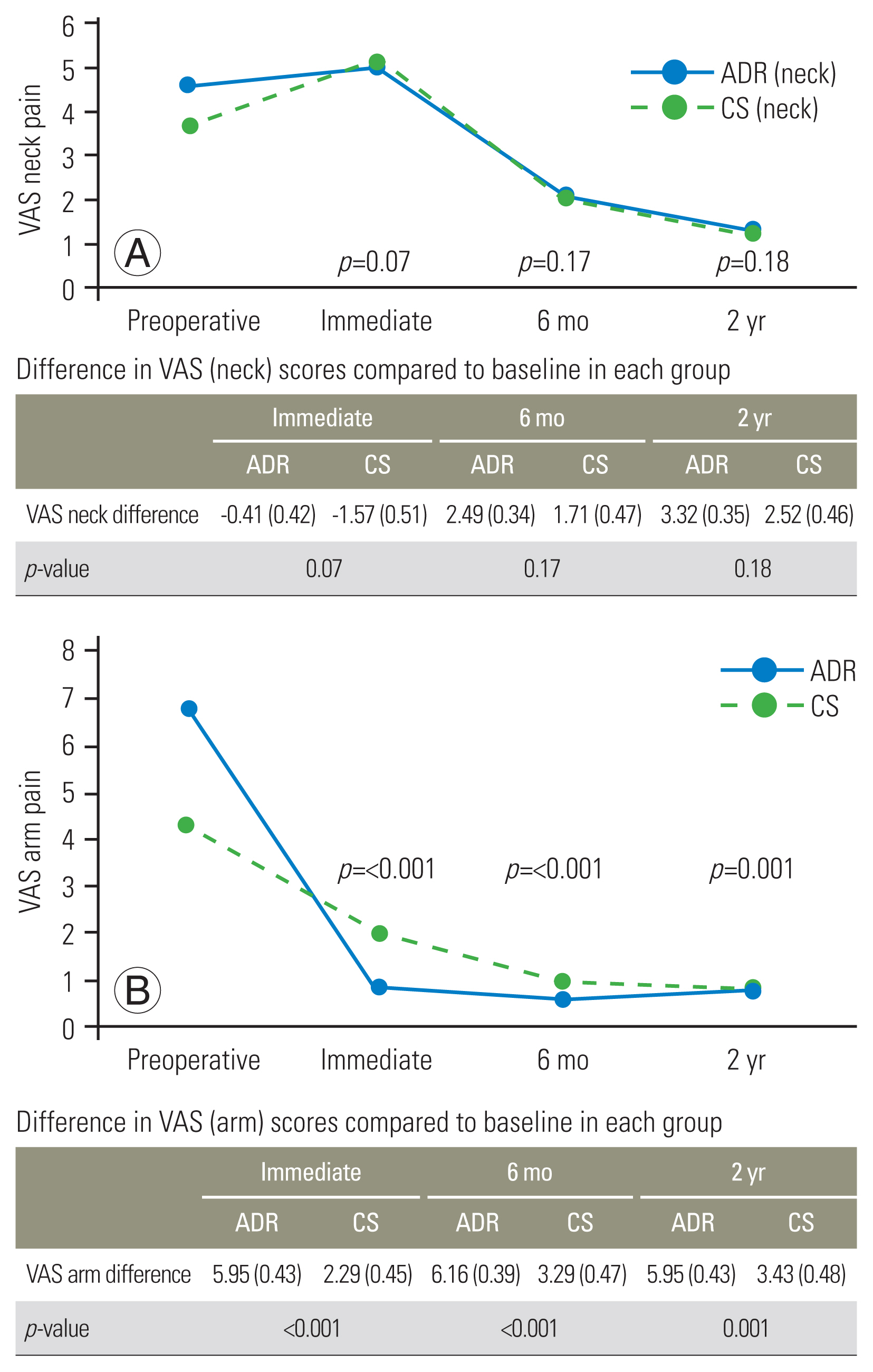
Abstract
Study Design
Retrospective single-center, single-surgeon cohort study.
Purpose
Our goal was to compare the 2-year clinical and radiological results of artificial disc replacement (ADR) and cage screw (CS) implants in patients with cervical degenerative disc disease (DDD).
Overview of Literature
Anterior cervical discectomy and fusion with CS implants are an acceptable alternative to traditional cage-plate construct due to perceived decreased complications of dysphagia. However, patients may experience adjacent segment disease because of increased motion and intradiscal pressure. ADR is an alternative to restore the physiological kinematics of the operated disc. Few studies directly compare ADR and CS construct for their efficacy.
Methods
Patients who received single-level ADR or CS between January 2008 and December 2018 were included. Data collected was preoperatively, intraoperatively, and postoperatively (6, 12, 24 months). Demographic information, surgical information, complications, follow-up surgery, and outcome ratings (Japanese Orthopaedic Association [JOA], Neck Disability Index [NDI], Visual Analog Scale [VAS] neck and arm, 36-item Short Form Health Survey [SF-36], EuroQoL-5 Dimension [EQ-5D]) were gathered. The radiological assessment included motion segment height, adjacent disc height, lordosis, cervical lordosis, T1 slope, the sagittal vertical axis C2–7, and adjacent level ossification development (ALOD).
Results
Fifty-eight patients were included (ADR: 37 and CS: 21). At 6 months, both groups’ JOA, VAS, NDI, SF-36, and EQ-5D scores significantly improved, and the positive trends persisted at 2 years. Noted no significant difference in the enhancement of clinical scores except for the VAS arm (ADR: 5.95 vs. CS: 3.43, p=0.001). Radiological parameters were comparable except for the progression of ALOD of the subjacent disc (ADR: 29.7% vs. CS: 66.9%, p=0.02). No significant difference in adverse events or severe complications seen.
Conclusions
ADR and CS obtain good clinical results for symptomatic single-level cervical DDD. ADR demonstrated a significant advantage over CS in the improvement of VAS arm and reduced progression of ALOD of the adjacent lower disc. No statistically significant difference of dysphonia or dysphagia between the two groups were seen, attributed to their comparable zero profile.
Introduction
Cervical degenerative disc disease (DDD) has a varied spectrum of presentations ranging from asymptomatic to patients having debilitating and intractable pain and/or neurological deficits. Physiotherapy, non-steroidal anti-inflammatory medications, traction, and activity modification are examples of non-operative treatments. Failing a period of conservative measures, anterior cervical discectomy and fusion with cage and plate construct (anterior cervical discectomy and fusion [ACDF]) is the traditional surgical option for cervical radiculopathy and myelopathy. The goals of ACDF are to restore anatomical disc space height, maintain segmental alignment, and achieve permanent segmental stabilization [1,2]. This procedure is typically well tolerated with excellent results [3,4]; however, 25% or more of patients may develop adjacent segment disease (ASD) within 10 years manifested as new radiculopathy or myelopathy in studies with longer follow-up [5]. Increased mobility and intradiscal pressure at nearby disc levels that have not undergone surgery are associated with the development of ASD [5,6]. However, this is now changing due to the development of newer implants such as cervical artificial disc replacement (ADR) and cage screw (CS) construct.
ADR was created as an alternative treatment to restore the physiological kinematics of the operated disc by trying to obtain normal segmental lordosis and near physiological motion [7,8]. ADR has been reported to provide outcomes that are comparable to or better than ACDF in several prospective randomized controlled trials with a 2-year follow-up [8–12]. These outcomes were corroborated with further studies with longer follow-up [13–15]. The favorable outcomes include a lower reoperation rate [16–18] and lower development of ASD compared to ACDF [9].
A frequently mentioned complication of ACDF is dysphagia, postulated to be related to postoperative soft tissue edema, hematoma, and adhesions around the implant [19]. Additionally, the profile of the plate is connected to dysphagia, with thicker plates being associated with higher rates of dysphagia [20]. CS implants were constructed to provide immediate biomechanical stability similar to that of cage and plate construct (e.g., Zero-P; DePuy Synthes, West Chester, PA, USA) but without the anterior footprint and thickness. Less often reported dysphagia and implant failure, with comparable fusion rates, were found in short-term investigations comparing these implants to cage and plate build [21].
There is little evidence in the literature comparing ADR and CS construct directly for the treatment of single-level cervical DDD. The goal of this study was to compare the clinical and radiological results of ADR and CS implants at 2-year follow-ups.
Materials and Methods
The requirement for informed consent from individual patients was omitted because of the retrospective design of this study and was approved by the National Healthcare Group Domain Specific Review Board with the reference 2016/00115-AMD0003.
1. Subject design
All consecutive patients who received single-level ADR with ProDisc-C device (DePuy Synthes) or CS with Zero-P VA Stand-Alone Implant (DePuy Synthes) by a single spine surgeon were enrolled, between January 2008 and December 2018, within a single-center. Inclusion criteria comprised of single-level cervical DDD secondary to disc herniation or focal osteophytes producing symptomatic nerve root and/or spinal cord compression, aged between 25 and 70 years old, symptoms refractory to at least 6 weeks of conservative management. Exclusion requirement comprised of radiological signs of instability defined by dynamic (flexion/extension) radiographs indicating sagittal plane translation >3.5 mm or angulation >20°, two or more cervical levels requiring surgery, previous cervical spinal surgery, ossification of posterior longitudinal ligament, rheumatoid arthritis, ankylosing spondylitis, metabolic bone disease, trauma, tumor, and infection.
2. Outcome assessment
Clinical results were evaluated with the Japanese Orthopaedic Association (JOA) Score, Neck Disability Index (NDI), 36-item Short Form Health Survey SF-36 (Physical and mental component), EuroQoL-5 Dimension (EQ-5D), and Visual Analog Scale (VAS) for neck and arm pain by the outcome evaluation team. Additionally, any serious issues that arose during the procedure and afterward were noted. Plain and dynamic standing radiographs and magnetic resonance imaging scans were digitally analyzed preoperatively. Postoperatively, only plain standing radiographs (neutral anteroposterior and lateral radiographs) were conducted immediately, postoperatively on day 2, 6 months, 1 year, and 2 years. Radiological assessments, as shown in Fig. 1, included surrogate motion segment height (of the superior endplate of the upper vertebral body to the lower endplate of the lower vertebral body adjacent to the replaced disc), implant subsidence can hereby be estimated by a change in the serially determined surrogate motion segment height, adjacent disc height and sagittal Cobb angle (upper and lower), cervical lordosis (sagittal C2–7 Cobb angle), T1 slope, the sagittal vertical axis (SVA) of C2–7, adjacent level ossification development (ALOD) using the classification of Park et al. [22]. Radiological parameters were measured by a senior orthopedic resident, and guided by a senior orthopedic consultant. The methodology for analyzing these radiological parameters was internally verified in a local audit. Interrater reliability was near perfect agreement with Cohen’s kappa calculated to be 0.84.
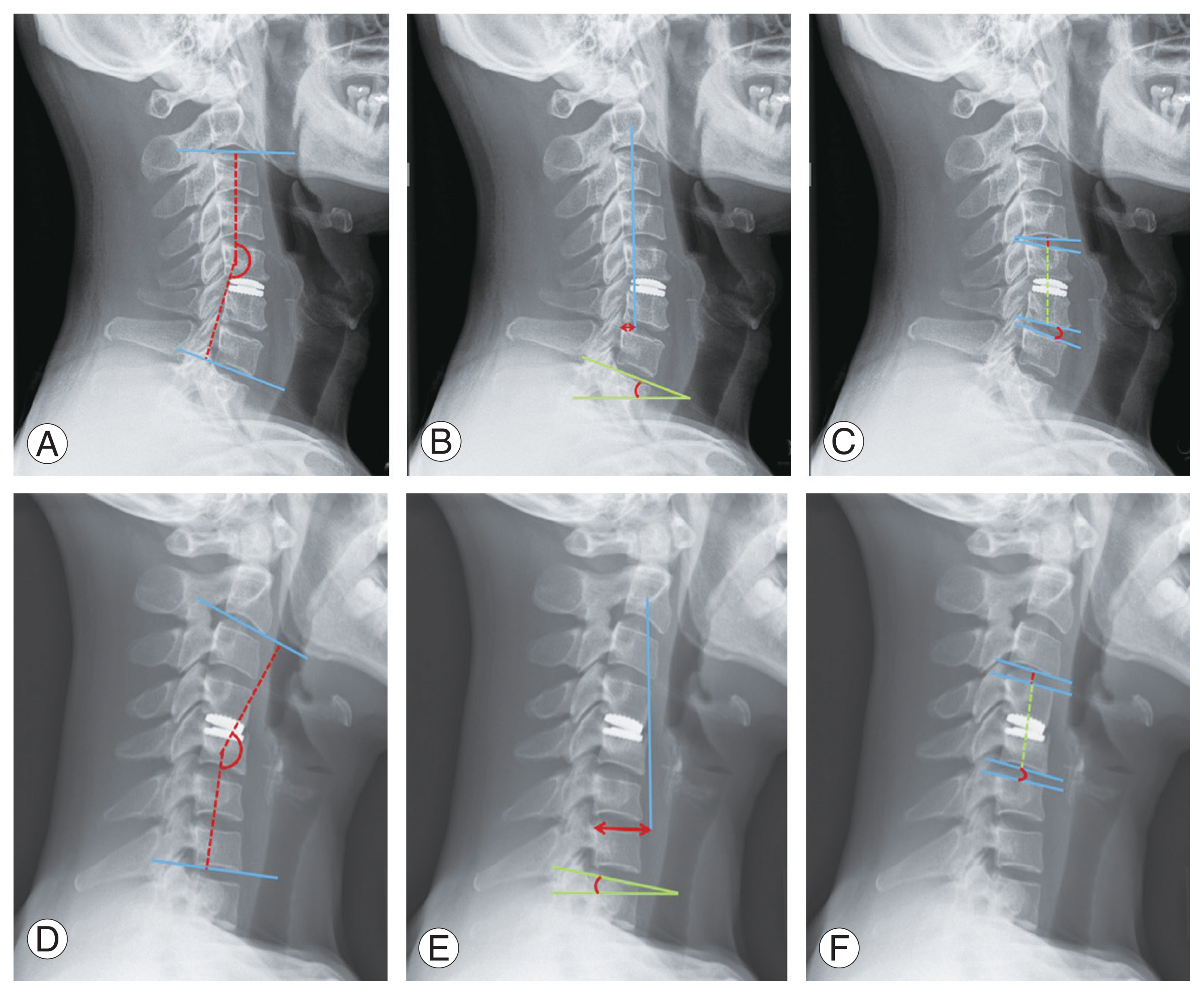
Measurement of the C2–C7 radiological parameters in a lordotic cervical spine: (A) C2–C7 sagittal Cobb angle; (B) C2 sagittal vertical axis, T1 slope; (C) adjacent disc sagittal height upper (red), surrogate motion segment height (green). Measurement of the C2–C7 radiological parameters in a neutral/ kyphotic cervical spine: (D) C2–C7 sagittal Cobb angle; (E) C2 sagittal vertical axis, T1 slope; (F) adjacent disc sagittal height upper (red), surrogate motion segment height (green).
3. Statistical methods
IBM SPSS Statistics for Windows ver. 26.0 (IBM Corp., Armonk, NY, USA) was used. The normally distributed data and not normally distributed data are presented as mean±standard deviation, and median including range respectively. The Wilcoxon signed-rank test was applied for within-group comparison of preoperative and postoperative results. The Mann-Whitney U test was used for the between-group comparison of results. Categorical data, including sex, diagnosis, and index level in the two groups were analyzed by chi-square test or Fisher’s exact test for small samples. A p-value of <0.05 was defined as significant.
Results
A total of 58 patients (37 ADR and 21 CS) completed a minimum of 2-year follow-up and were included. There were differences in the baseline demographics of patients between the ADR and CS group for age (46.5 years old versus 62.5 years old, p<0.001), and percentages of males (83.8% versus 57.1%, p=0.03). In terms of BMI, smoking status, race, pathology, intraoperative blood loss, and levels of operated discs, there were no statistical differences between the two groups. The patient demographics of the two groups are illustrated in Table 1.
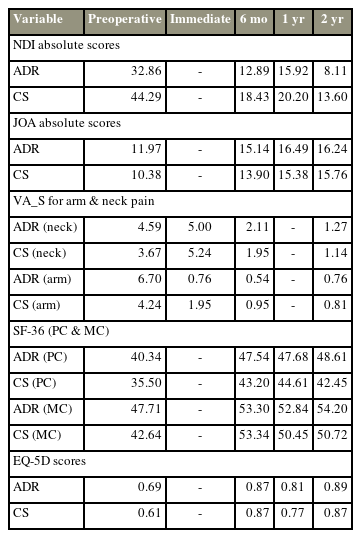
1. Neck Disability Index scores
The NDI scores significantly enhanced from preoperative scores in both groups by 6 months and these enhancements were sustained for 2 years. In the ADR group, NDI scores increased to 12.89 at 6 months (p<0.001), 15.92 at 1 year (p<0.001), and 8.11 at 2 years (p<0.001), from a mean preoperative score of 32.86. In the CS group, NDI scores improved to 18.43 at 6 months (p<0.001), 20.2 at 1 year (p<0.001), and 13.6 at 2 years (p<0.001), from a mean preoperative score of 44.29 as seen in Table 2. At 6-month, 1-year, and 2-year periods, the improvement in NDI scores was not significantly different between the two groups (p=0.34, p=0.32, and p=0.25, respectively) as depicted in Fig. 2.
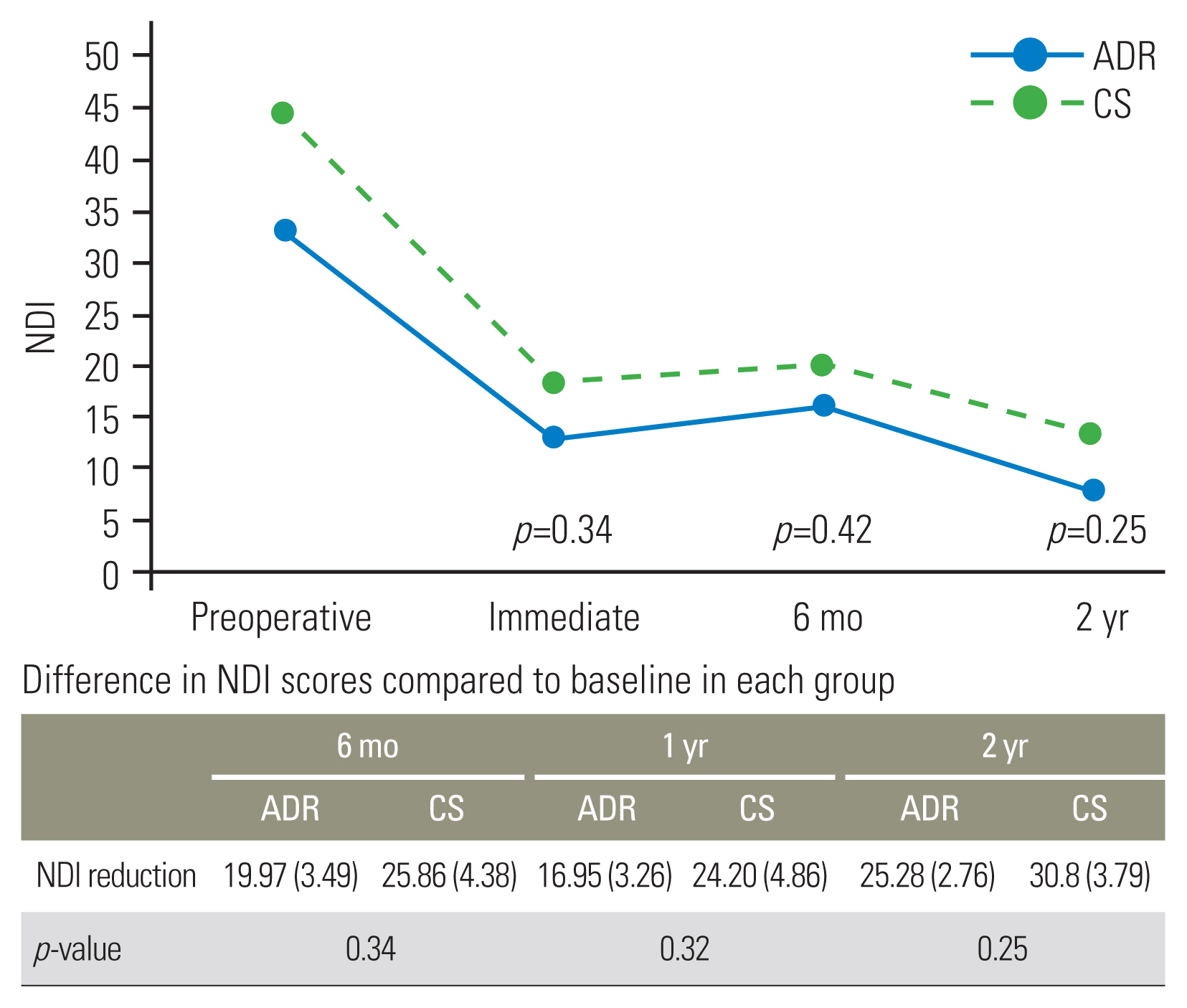
2. Japanese Orthopaedic Association scores
The JOA scores significantly improved from preoperative scores in both groups by 6 months and these improvements were sustained for 2 years. In the ADR group, JOA scores improved by 3.16 at 6 months (p<0.001), 4.51 at 1 year (p<0.001), and 4.27 at 2 years (p<0.001), from a mean preoperative score of 11.97. From a mean preoperative score of 10.38 as shown in Table 2, the JOA scores in the CS group increased by 3.52 at 6 months (p<0.001), 5.00 at 1 year (p<0.001), and 5.38 at 2 years (p<0.001). The improvement in JOA scores was not significantly different between the two groups during the 6-month, 1-year, and 2-year follow-up (p=0.37, p=0.43, and p=0.15, respectively) as shown in Fig. 3.
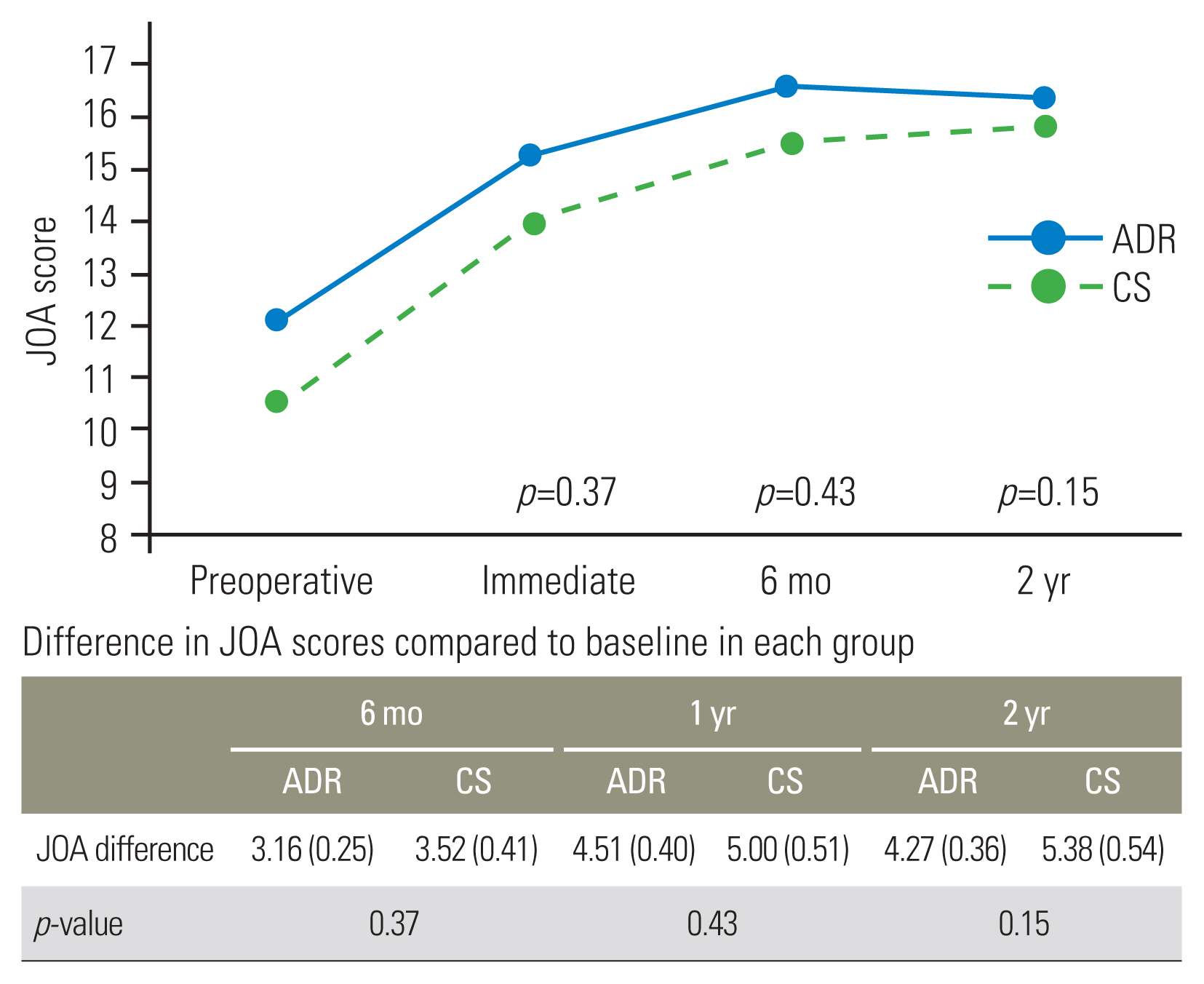
3. Visual Analog Scale-neck pain
In the ADR group, VAS neck deteriorated immediately postoperatively (increased by 0.41; p=0.40) but it was not significant. In the CS group, VAS neck worsened immediately postoperatively (increased by 1.57; p=0.01) which was significant. However, both groups afterward greatly outperformed their preoperative scores at 6 months, and these gains persisted for 2 years. In the ADR group, VAS neck increased by 2.49 at 6 months (p<0.001) and 3.32 at 2 years (p<0.001), from a mean preoperative score of 4.59. In the CS group, VAS neck scores increased by 1.71 at 6 months (p=0.003) and 2.52 at 2 years (p<0.001), from a mean preoperative score of 3.67 as depicted in Table 2. Fig. 4A shows that when comparing the two groups, the improvement in VAS neck scores did not differ statistically significantly after 6 months, a year, or 2 years (p=0.07, p=0.17, and p=0.18, respectively).
4. Visual Analog Scale-arm pain
The VAS arm scores significantly increased from preoperative scores in both groups during the immediate postoperative period and these improvements were maintained for 2 years. From a mean preoperative score of 6.70, the VAS arm in the ADR group increased by 5.95 at the immediate postoperative period (p<0.001), 6.16 at 6 months (p<0.001), and 5.95 at 2 years (p<0.001). In the CS group, VAS arm scores improved by 2.29 at the immediate postoperative period (p<0.001), 3.29 at 6 months (p<0.001), and 3.43 at 2 years (p<0.001), from a mean preoperative score of 4.24. As can be shown in Fig. 4B, the ADR group improved VAS arm scores much more than the CS group did at the 6-month, 2-year, and immediate postoperative time points (p=0.001, p=0.001, and p=0.001, respectively).
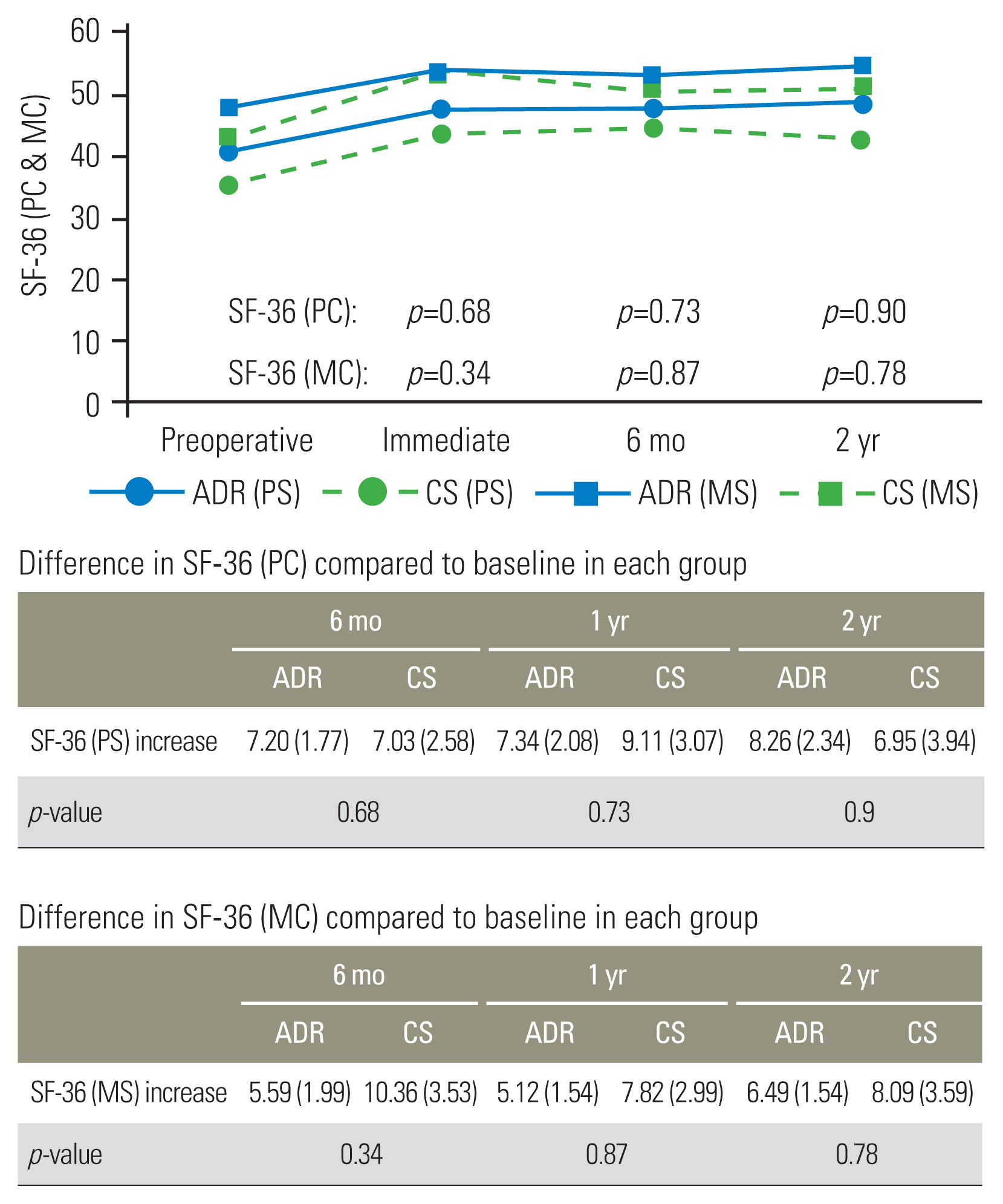
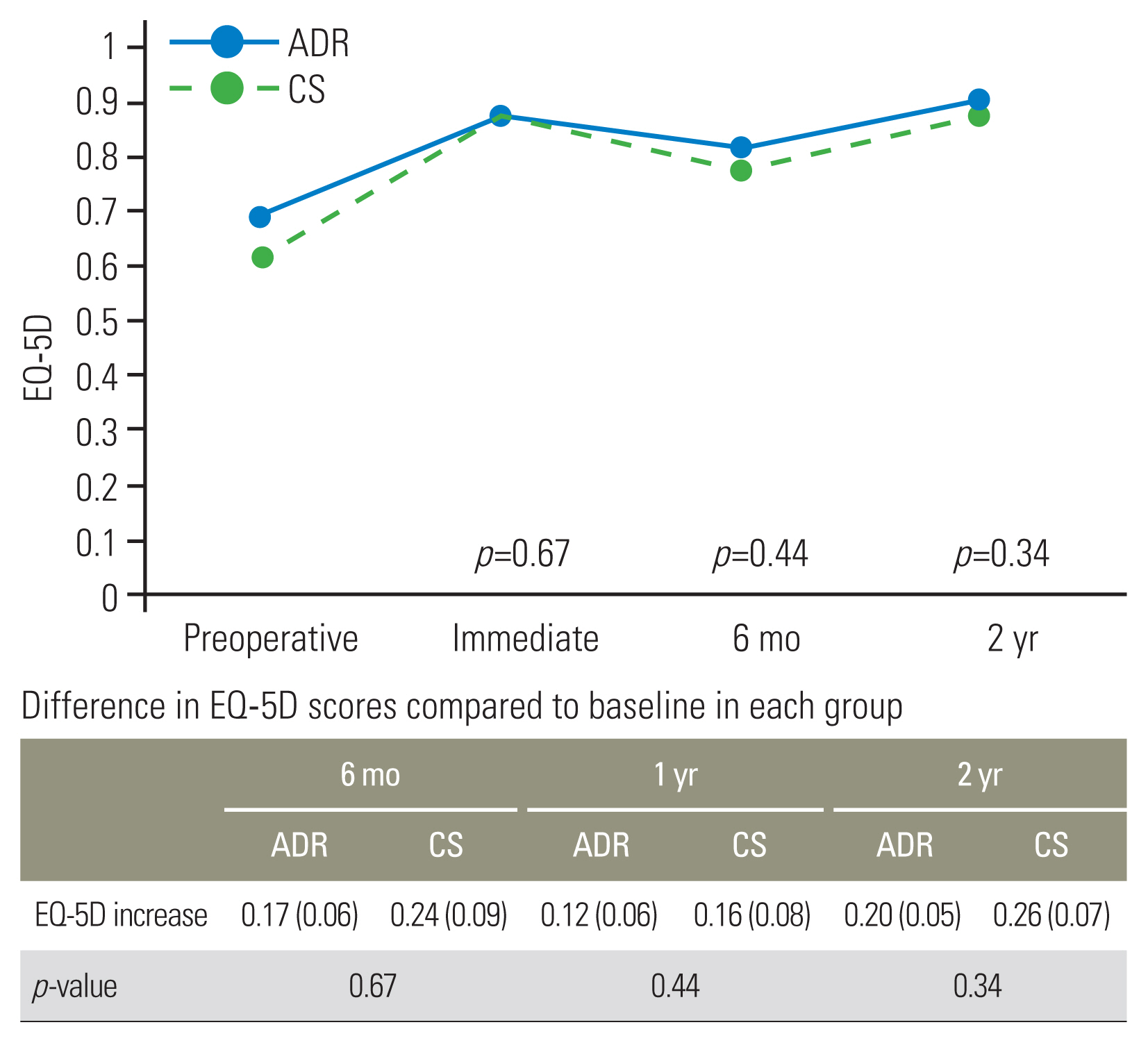
5. 36-Item Short Form Health Survey
At 2 years, the mean SF-36 physical component and mental component scores had increased for both groups compared to preoperative levels but only revealed significance in the ADR group (p=0.002). The mean preoperative SF-36 physical component scores were 40.34 and 35.50 for the ADR and CS groups, respectively, increasing to 48.61 (p=0.002) and 42.45 (p=0.09) at 2 years (Fig. 5). The mean preoperative SF-36 mental component scores were 47.71 versus 42.64 for the ADR and CS groups, respectively, improving to 54.20 (p=0.001) and 50.72 (p=0.117) as shown in Table 2. As shown in Table 2, the mean preoperative SF-36 mental component scores for the ADR and CS groups were 47.71 and 42.64, respectively, and they increased to 54.20 (p=0.001) and 50.72 (p=0.117), respectively.
6. EuroQoL-5 Dimension
The mean EQ-5D ratings for both groups had significantly increased after 2 years compared to preoperative levels. The mean preoperative EQ-5D scores were 0.69 and 0.61 for the ADR and CS groups, respectively, increasing to 0.89 (p=0.001) and 0.87 (p=0.002) at 2 years as depicted in Table 2. At 6-month, 1-year and 2-year periods, the improvement of EQ-5D was not significantly different between the two groups (p>0.05) as seen in Fig. 6.
7. Radiological outcomes
There were no cases of device migration in both groups. As depicted in Table 3, the mean motion segment height (surrogate) was 36.87 mm and 35.78 mm for the ADR and CS groups, respectively, decreasing to 36.03 mm (p=0.001) and 35.00 mm (p=0.008) at 2 years. There was no discernible difference between the two groups in the evolution of motion segment height, a measurement of implant subsidence (p=0.92) (Fig. 7).
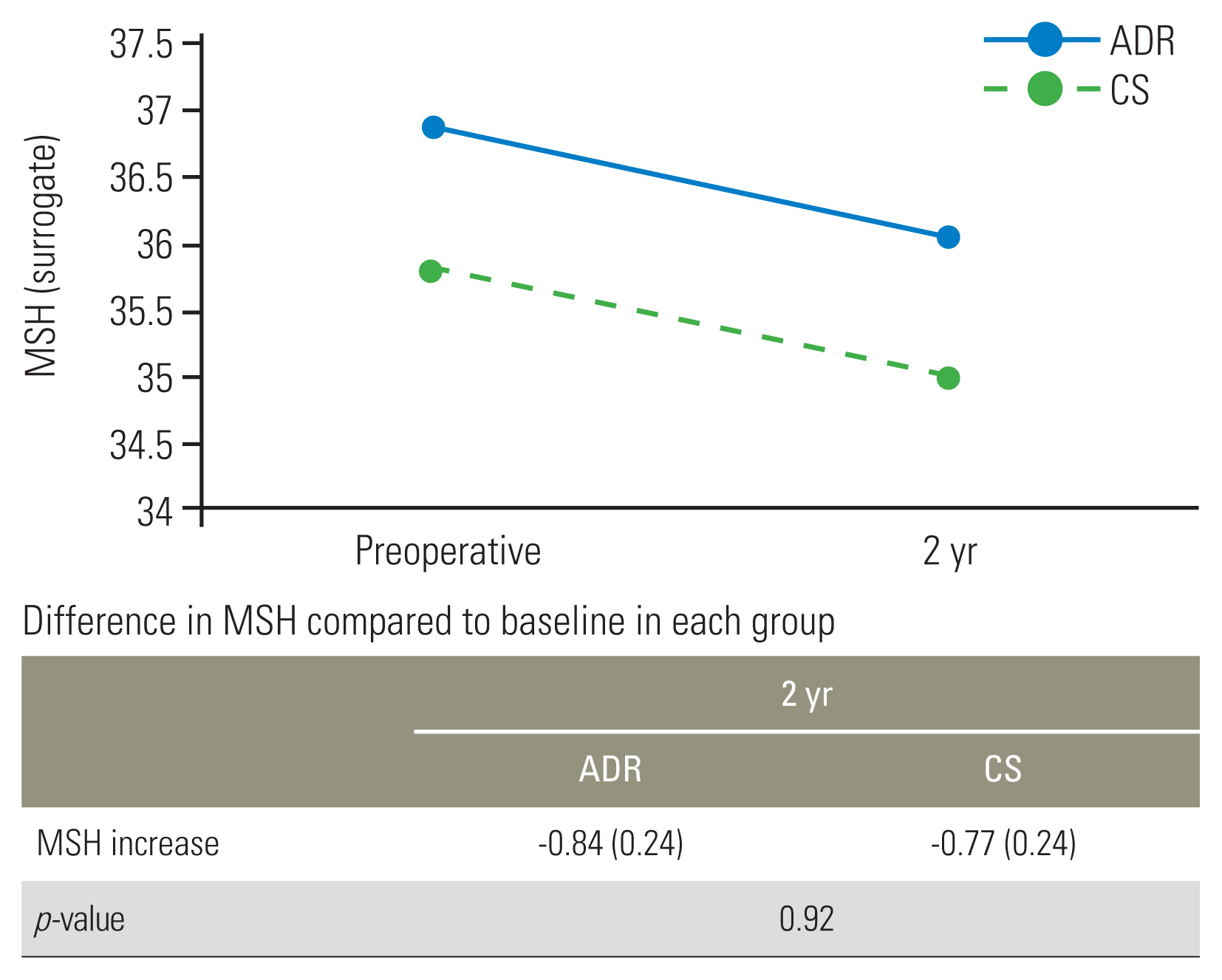
Motion segment height (MSH, surrogate) in the artificial disc replacement (ADR) group and cage screw (CS) group preoperatively and at 2-year follow-up. Values are presented as number (%).
The mean preoperative cervical lordosis was 11.16° and 7.81° for the ADR and CS groups, respectively, progressing to 12.21° and 6.04° at 2 years, but it was not statistically significant (p=0.21 and p=0.74) as seen in Table 3. There was no significant progression of T1 slope, SVA C2–7, upper and reduce adjacent disc heights, and sagittal Cobb angles as illustrated in Table 3.
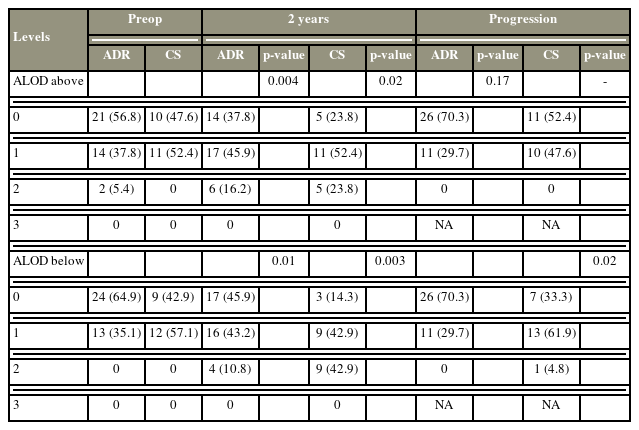
Preoperatively, there was no discernible difference between the upper disc ALOD mean scores in the ADR group and the CS group (0.48 versus 0.52, p=0.81). Upper disc ALOD progressed in 29.7% (p=0.004) of the ADR group compared to 47.6% (p=0.02) of the CS group, but there was no significant difference between the two groups (p=0.17) as shown in Table 4. Preoperatively, the lower disc ALOD mean scores were 0.35 in the ADR group compared to 0.57 in the CS group but there was no considerable difference (p=0.11). Lower disc ALOD advanced in 29.7% (p=0.01) of the ADR group compared to 66.7% (p=0.003) of the CS group. According to Table 4, there was a statistically significant difference between the groups, demonstrating ADR’s superiority over CS in the slower evolution of lower disc ALOD (p=0.02).
8. Complications
Within the ADR group, there were three patients (8.1%) who experienced dysphagia, one patient (2.7%) had a surgical site hematoma, one patient (2.7%) developed pseudoarthrosis and one patient (2.7%) suffered a minor sensory neurological deficit. Within the CS group, three patients (14.2%) suffered either dysphagia or dysphonia, and one patient (4.8%) developed pseudoarthrosis. Each case of dysphagia was minor and went away in 3 weeks. Between ADR and CS, there was no discernible difference in adverse events (p=0.72). None of the patients experienced surgical site infection, implant loosening, or breakage.
Discussion
Our results show that both ADR and CS implants obtain good clinical results for patients with symptomatic single-level cervical DDD. There was a significant improvement in VAS arm score and reduced development of ALOD of the subjacent disc with ADR compared to CS implant. ALOD has been linked to anterior cervical surgeries; it often appears a year after surgery and progresses to extensive ossification by 24 months [22]. Patients with minimal ossification at 12–24 months are unlikely to progress to advanced ALOD [23]. A minimum stripping of the anterior longitudinal ligament and avoiding Caspar pins and anterior plates are some recommended methods to reduce the incidence of ALOD [24]. While undesirable, ALOD does not appear to greatly influence clinical results at 2 years. However, ALOD might be a herald for ASD and symptomatic ASD is a common reason for subsequent surgery [16,17]. In the classic paper by Hilibrand et al. [5], the rate of symptomatic ASD was determined to be 2.9% per year.
The ADR group also showed significantly better VAS arm improvement compared to CS. We can make comparisons to other randomized controlled trials that showed that ADR was superior to ACDF for arm pain at 24–60 months after surgery [25,26]. However, we theorize that these significances could be confounded by the different patient demographics between the two groups. The mean age in the ADR group was younger than that in the CS group (46.5 years versus 62.5 years, p<0.001). Symptomatic cervical DDD in younger patients is typically more acute in onset and frequently due to a herniated nucleus pulposus, compared to an older patient with more subacute pain resulting from nerve impingement by an osteodiscoligamentous complex consisting of syndesmophytes, disc bulge, and facet joint arthritis. Technically speaking, the decompression of such an osteodiscoligamentous complex is more difficult than that of a straightforward herniated disc. Hence, although this discovery was statistically significant, its therapeutic relevance may not necessarily follow.
The age difference between the two groups in our study was significant. ADR is a suitable alternative because symptomatic disc prolapse is the pathophysiology in younger patients. Older patients above 65 years of age usually have lower activity demands and the prevailing literature favors fusion for older patients. Hence, the tendency for offering these patients CS over ADR. Additionally, with similar treatment ideas of fusion, CS is a more viable alternative to the conventional ACDF. This comparison is necessary and appropriate given the size of the implant and the zero profile of both ADR and CS.
There was no discernible difference in adverse events between the ADR and CS groups. Notably, the incidence of dysphagia and dysphonia in both groups were similar. In the landmark US Food and Drug Administration-approved investigational device exemption clinical trials, there was a statistically significant decrease in dysphagia and dysphonia seen in the ADR group compared to the conventional ACDF group [10–12]. In our study, the zero profile CS system was utilized instead of the traditional cage-plate system which carries a higher profile with the use of a plate. We hypothesize that the zero profile CS system’s innovative design has made it possible for postoperative dysphagia and dysphonia rates to be equivalent to ADR.
There are several limitations in this study. Firstly, given the retrospective nature of this study, there is a possibility of inherent patient selection bias. The choice of implants was left up to the surgeon’s judgment based on his evaluation of the patient’s appropriateness. In general, patients above 65 years old were offered CS while younger patients were measured radiologically for suitability and offered either ADR or CS following a thorough discussion of the pros and cons. As a result, ADR for younger patients and CS for older patients may both have selection bias.
Second, the sample size of 58 is relatively small. Furthermore, only a few patients had complications. While the inter-group comparisons did not reveal the statistical difference, our findings should be considered in light of this. Future studies of greater scope and longer duration would provide a more precise comparison of the incidence of problems in the two implant groups, which would in turn reflect the durability of the two implants.
Conclusions
In our retrospective cohort study on the outcomes of single-level cervical ADR compared to CS, 2-year results revealed that both groups obtain a good clinical result for patients with symptomatic single-level cervical DDD. ADR demonstrated a significant advantage over CS in the improvement of VAS arm and reduced progression of ALOD of the adjacent lower disc. However, there was no significant difference in the incidence of dysphagia or dysphonia in the ADR group compared to CS, which may be due to the similar zero profile of both implants examined. Nevertheless, as both implants already obtained comparable and highly promising outcomes in the early postoperative period, further studies with answers on the longevity of the implants would ultimately guide a spine surgeon in his implant of choice.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conceptualization: NK; data curation: TYZE, DS; formal analysis: SL, NK, TYZE; methodology: NK; project administration: NK; visualization: TYZE, NK; writing–original draft: TYZE, NK; writing–review & editing: all authors; and final approval of the manuscript: all authors.