Axial Neck Pain after Cervical Laminoplasty with Preserving C7 Spinous Process Using C7 Arcocristectomy: A Prospective Study
Article information
Abstract
Study Design
Single-blinded, randomized, single-center, prospective study.
Purpose
This study aims to compare the radiographical and clinical outcomes between C7 laminoplasty and C7 arcocristectomy, which preserves the C7 spinous process.
Overview of Literature
Laminoplasty is a widely used surgical method that decompresses the cervical spinal cord. However, axial neck pain is one of the major factors of dissatisfaction, and still, it is not clearly solved the reduction method of postoperative axial neck pain.
Methods
Thirty-one patients with multilevel cervical spondylotic myelopathy who required C6–C7 level decompression surgery were operated and followed up for 24 months. One group (15 patients) received C7 arcocristectomy without laminoplasty, and the other group (16 patients) received C7 laminoplasty. Flexion, neutral, and extension angles were measured using the Cobb method at C2–C7 to evaluate preoperative and postoperative radiographic parameters. Range of motion (ROM), ROM preservation rate of the cervical spine, C2–C7 sagittal vertical axis (SVA), and T1 slope were measured using C-spine lateral X-ray. The Visual Analog Scale (VAS) and modified Japanese Orthopedic Association (JOA) score were used to compare preoperative and postoperative clinical symptoms.
Results
Flexion, neutral, extension angles of the cervical spine, C2–C7 SVA, T1 slope, ROM, ROM preservation rate, and modified JOA score were not significantly different between the two groups (p>0.05). In the C7 arcocristectomy group, the average postoperative VAS for axial neck pain was increased in 13.3% (2/15) of the patients, whereas in the C7 laminoplasty group, the average postoperative VAS was increased in 43.8% (7/16) of the patients (p=0.018).
Conclusions
C7 arcocristectomy, which preserves the C7 spinous process and posterior structures, is a useful technique for relieving axial neck pain.
Introduction
Laminoplasty is a non-fusion surgical method widely used to preserve cervical motion while decompressing the cervical spinal cord [1]. In addition, laminoplasty has strong advantages over laminectomy in preventing postoperative kyphosis, segmental instability, and other post-laminectomy complications. However, cervical laminoplasty has complications, including axial neck pain and reduction in cervical motion [2–7]. Even in patients who have recovered neurologic symptoms after surgery, axial neck pain is a prominent source of dissatisfaction [8,9].
The exact etiology of persistent axial neck pain following laminoplasty is still unclear. Several studies have suggested that axial neck pain may be prevented by preserving the C7 spinous process and its muscle and ligament attachments [10–14]. To minimize surgical invasion of the nuchal muscles, a new procedure changing the area of decompression from “C3–C7” to “C3–C6” to preserve the C7 spinous process has been reported [10].
The preservation of the C7 spinous process in cervical laminoplasty is still controversial. Several studies showed no difference between preserving and sacrificing the C7 spinous process in cervical laminoplasty [15]. Other studies found significant differences in axial neck symptoms and the Japanese Orthopedic Association (JOA) score when the C7 spinous was preserved or sacrificed [11–16]. In addition, previous studies compared axial pain after laminoplasty with and without C6–C7 level decompression. There still needs to be research focused on the range of motion (ROM), cervical alignments, and neck pain after laminoplasty with C7 arcocristectomy. In this study, C7 arcocristectomy was applied to the multilevel open-door laminoplasty to preserve the C7 supraspinous ligament and posterior structures. To confirm the effectiveness of preserving the C7 supraspinous ligament after cervical laminoplasty, radiographic (ROM and alignment) and clinical (preoperative and postoperative axial pain) outcomes were analyzed and compared.
Materials and Methods
This study was conducted in accordance with the principles of the Helsinki Declaration, and the protocol was reviewed and approved by the Institutional Review Board of Busan Medical Center (IRB no., 2022-10-001). All patients provided informed consent before participating after an explanation of the research procedure.
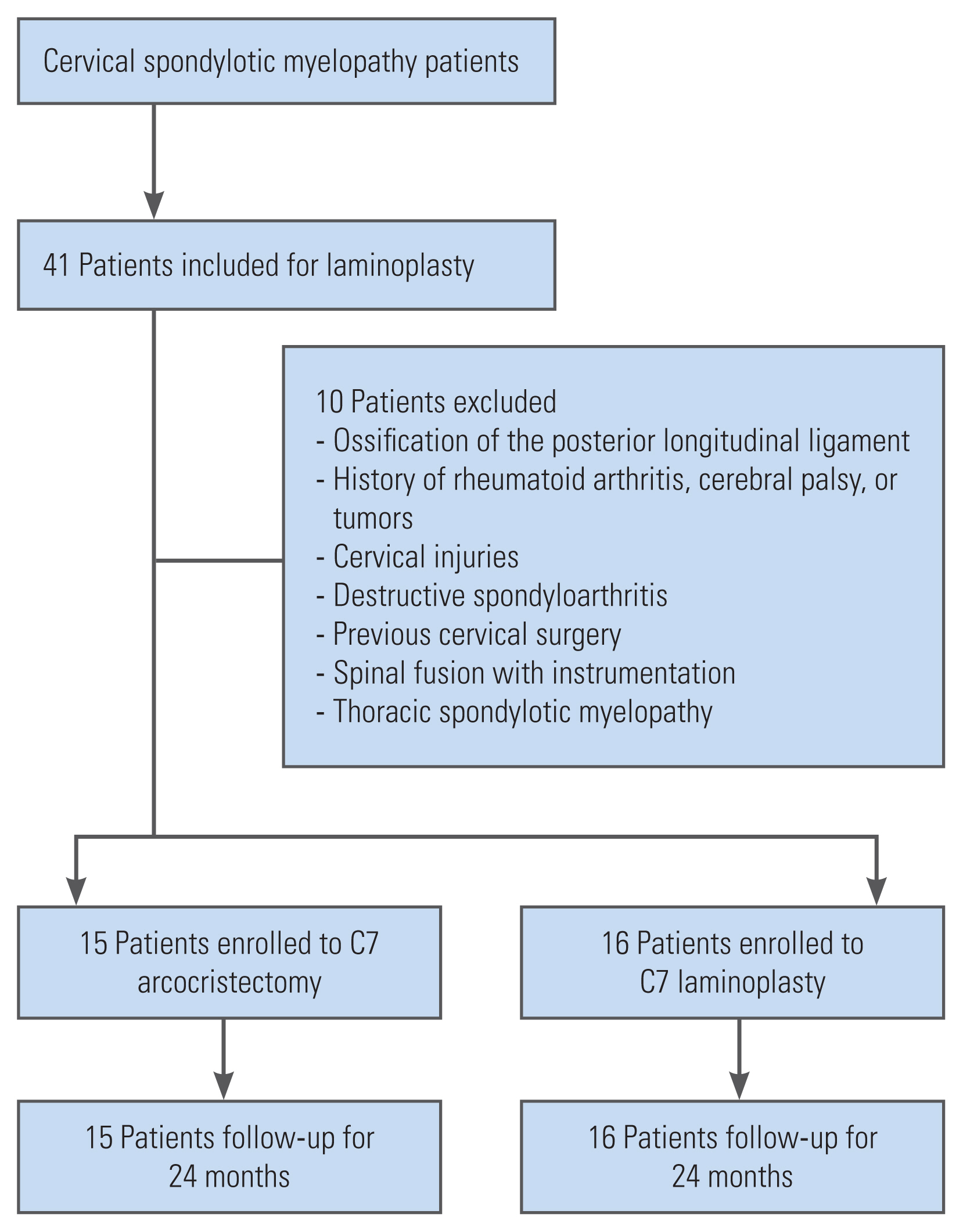
This is a prospective, single-center, single-blinded, randomized, and comparative study. This study included patients with multilevel (more than three levels) cervical spondylotic myelopathy, including C6–C7 level, who had multilevel cervical laminoplasty between March 2016 and August 2020. Among them, 10 patients were excluded based on the exclusion criteria indicated in Fig. 1. This study included 31 patients who were divided into two groups at random. Fifteen patients were assigned to group A to preserve the C7 spinous process with C7 arcocristectomy, and 16 patients were assigned to group B to sacrifice the C7 posterior structure with laminoplasty at the C7 level. When the patient enrolled in the study, the randomization program of the website (www.Randomizer.org) was used to randomize the surgical treatment. Patients were randomly assigned, and the number of patients was evenly distributed for both groups. After the confirmation of inclusion, the assignment of each patient to the surgical technique was shown to the surgeon.
APIS dolphin plate (TDM, Gwangju, Korea) and its application was operated by one experienced orthopedic surgeon. Arcocristectomy, like dome-like laminoplasty, can decompress the spinal cord while preserving the muscular attachments at the upper part of C7 with minimum surgical exposure. Approximately 50% of the upper part of the laminae and ligamentum flavum can be removed using arcocristectomy (Fig. 2). In this study, C7 arcocristectomy was used only at the C6–C7 level to preserve the C7 spinous process, and modified open-door laminoplasty was used at the other cervical spine level. Fig. 3 is an example of a patient who had laminoplasty at C5–C6 and arcocristectomy at C7 and was diagnosed with cervical spondylotic myelopathy at the C5–C7 levels. The anteroposterior and lateral views of the cervical spine model are shown. During each operation, the facet joint and the origin of the muscles attached to C2 and C7 were preserved as much as possible.

A Cervical spine mock-up model of a patient with laminoplasty at C5, C6 and arcocristectomy at C7. (A) Anteroposterio view. (B) Lateral view.
ROM exercise was started 4 weeks after surgery, and patients were followed up for at least 24 months. Radiological measurements and clinical symptoms were compared to evaluate the patients’ surgical outcomes. The sagittal vertical axis (SVA) and Cobb angles at the C2–C7 level with flexion, neutral, and extension in the lateral view of cervical X-ray, ROM, and ROM preservation rate were measured in the radiographic measurements. The cervical spine Cobb angle is measured by drawing parallel lines from the lower endplate of the C2 vertebral level to the lower endplate of the C7 vertebral level. Perpendicular lines are drawn from the previous two lines, and the angle at which they intersect is known as the cervical Cobb angle. The horizontal distance between the posterosuperior corner of the C7 vertebral body and a plumb line drawn from the center of C2 is used to measure C2–C7 SVA. Preoperative and postoperative clinical symptoms were measured using the neck Visual Analog Scale (VAS) and the modified JOA score. The average postoperative VAS is the outcome 2 years after the operation. This study compared and analyzed the radiologic and clinical data preoperatively and 2 years after the surgery.
For the statistical analysis, demographic data were analyzed using the paired t-test. Categorical variables were analyzed using the Mann-Whitney U test and the Wilcoxon sign-ranked test, and continuous variables were analyzed using repeated analysis of variance. A p-value <0.05 was considered a statistically significant variable. For all statistical analyses, IBM SPSS ver. 24.0 (IBM Corp., Armonk, NY, USA) was used. The intraclass correlation coefficient between the two assessments was 0.857 (0.713–0.921) for the reliability of the intra-observer analysis of the one spinal surgeon.
Results
The study included 31 patients (15 men and 16 women) with a mean age of 62.4 years (range, 48–79 years). The average number of segments operated was 3.65. The gender composition of groups A and B differed; however, there was no significant difference between the two groups when a p-value of 0.332 was used. The p-values for average age and the number of segments operated were 0.742 and 0.415, respectively, with no significant differences between the two groups (Table 1).
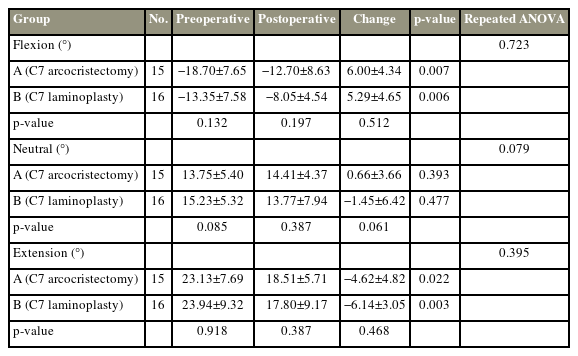
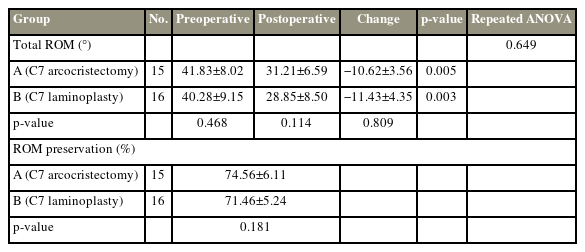
For the comparison between the preoperative and postoperative radiographic parameters, the Cobb flexion, neutral, and extension angles were measured in Table 2 to compare the preoperative and postoperative radiographic parameters. The Cobb angles of each position and the changes in the Cobb angles after the operation showed no significant differences between C2–7 groups A and B.
C2–C7 SVA was measured in both groups before and after the operation (Table 3). The preoperative and postoperative C2–C7 SVAs in group B were larger than in group A with approximately 2.54 mm and 1.56 mm, respectively; however, there were no significant differences between the two groups when p-values were >0.05. T1 slope was measured before the operation, and group B showed a larger T1 slope angle than group A with approximately 0.78°, although this was not statistically significant (p=0.243).
When total ROM and ROM preservation rate were compared, the postoperative total ROMs in group A were decreased by 10.62° and 11.43° in group B (Table 4). These changes have no statistically significant differences (p=0.809). Group A had a ROM preservation rate of 74.56%, whereas group B had a ROM preservation rate of 71.46%. The difference in ROM preservation rates between groups A and B was 3.10%, although not statistically significant when p=0.181 was considered.
In the clinical evaluation, the average changes of postoperative neck VAS in groups A and B were −1.10 and +0.36, respectively (Table 5). These results showed a statistically significant difference between the two groups (p=0.018). In Table 6, the change in neck VAS is categorized into three groups (increased, no change, and decreased). The percentage of patients with increased neck VAS in group A is 13.3% (2/15) and 43.8% (7/16) in group B. After surgery, 60.0% (9/15) of patients in group A and 25.0% (4/16) in group B showed decreased neck VAS. The average changes in the modified JOA score showed no significant difference between the two groups (p=0.223).
Discussion
Laminoplasty is a well-known surgical method for cervical spondylotic myelopathy. Laminoplasty has become more popular for spinal cord decompression because it was initially reported in 1973 [17]. Despite the advantages of laminoplasty, there has always been a concern that axial neck pain worsens the quality of life after laminoplasty.
Axial neck pain after laminoplasty remains an unresolved complication. Kimura et al. [9] investigated the time-dependent axial neck pain after double-door laminoplasty. They concluded that the axial neck pain persisted for 2 years after the operation. Most studies did not mention the exact incidence of axial neck pain [2]. According to Hosono et al. [16], axial neck pain was found in approximately 60% of cervical spondylotic myelopathy patients, and the pain remained in 42% of patients after laminoplasty. In the study by Kawaguchi et al. [17], axial pain was observed in 80% of patients. Ohnari et al. [18] reported that axial symptoms significantly increased after cervical laminoplasty from 60.8% to 78.3%.
The etiology of axial pain after laminoplasty can be found in the anatomy of the cervical spine. Several muscles could be included when considering the muscles related to axial neck pain after cervical laminoplasty. Among the cervical vertebral bodies, the rhomboid minor, upper part of the trapezius, superior part of the serratus posterior, and splenius capitis are attached to only C7. The C7 spinous process also provides a long lever arm to the extensor muscle complex, including the semispinalis, rhomboid, and trapezius [9]. The fibers of ligamentum nuchae are firmly attached to the C7 spinous processes. Because of the direct attachments of the ligamentum nuchae to the C7, the lower part of the cervical spine can endure excessive loading [19]. According to the research of Ito et al. [20], the trapezius muscle is related to neck pain [21]. Furthermore, the maximum force generated by the trapezius at C7 was greater than at the upper or middle cervical vertebrae [18]. For these reasons, preserving the C7 spinous process can prevent disrupting the cervical and shoulder muscles and reduce axial neck pain after laminoplasty.
Several new surgical procedures were developed to minimize postoperative axial neck pain. The area of decompression was changed from “C3–C7” to “C3–C6” to preserve the C7 spinous process [10,22,23]. Moreover, skip laminectomy or C7 dome laminoplasty was used to reduce axial neck pain in patients with multilevel cervical spondylotic myelopathy [24].
As previously stated, preserving the C7 spinous process in cervical laminoplasty is still controversial. Several studies focused on the similar results between preserving and sacrificing the C7 spinous process in cervical laminoplasty [9–11]. They compared the cervical mobility or curvature morphology, axial symptoms, and JOA score and found that both groups showed comparable neurologic improvement and axial symptoms. However, many studies insist that there are significant differences in axial symptoms, such as axial neck pain and neck stiffness, between preserving and sacrificing the C7 spinous process. They also found that the postoperative JOA score in the C7 preserving group is higher [11,12,25,26].
In this study, the authors attempted to exclude various factors that can cause postoperative axial pain. Postoperative axial neck pain increased in 13.3% (2/15) of patients in group A and 43.8% (7/16) of patients in group B. Interestingly, the two groups differed significantly in postoperative axial neck pain. In group A, during the C7 arcocristectomy, we preserved most of the C7 spinous process and resected as much of the upper half of the C7 lamina as possible for cervical spinal cord decompression. Because of the modified approach for preserving the C7 spinous process, damage to the facet joint is minimized, and the muscles attached to the C7 spinous processes, such as the semispinalis, splenius capitis, rhomboid minor, and trapezius, which are the source of the axial neck pain, are preserved. For these reasons, sufficient posterior decompression could relieve neurologic symptoms (increased postoperative modified JOA score) and improve axial neck pain (decreased neck VAS) after C7 arcocristectomy.
In the present study, the change of VAS was measured with the differences between postoperative and preoperative neck pain. After the operation, the VAS of patients who had C7 arcocristectomy (group A) was decreased by 1.1 points, whereas the VAS of patients who had C7 laminoplasty (group B) was increased by 0.36 point. After surgery, 43.8% (7/16) of patients in group B showed increased axial neck pain. However, 13.3% (2/15) of patients in group A showed increased axial neck pain after surgery. These results are the most significant difference between the two groups and are consistent with previous studies indicating that axial neck pain persists or increases after the surgery, which is the main complication of cervical laminoplasty.
In the technique of arcocristectomy, only the upper half of the cervical laminae and ligamentum flavum are removed to widen the spinal canal diameter [27,28]. It is comparable with dome laminoplasty in terms of accessing the upper part of the cervical laminae and decompressing posteriorly. In the case of dome laminoplasty, only the cephalad surface of the posterior arch and approximately 20%–30% of the upper laminae could be assessed. However, because of the approach of an anteriorly downward cutting angle to the upper part of the C7 spinous process, the arcocristectomy can provide sufficient decompression by removing most of the upper part of the posterior C7 lamina and the undersurface of the lateral surface of the C7 lamina. Moreover, arcocristectomy saves most spinous processes than dome laminoplasty. Fig. 4 shows the difference in surgical decompression area between arcocristectomy and dome laminoplasty using the C7 mock-up model. In terms of stability, the C7 spinous process is lengthy and posteriorly downward shaped, unlike other cervical spinous processes. Anatomically, stability is maintained even if the upper half of the laminae is removed by C7 arcocristectomy. For these reasons, we have used C7 arcocristectomy on patients who require decompression at the C6–C7 level. The supraspinous and interspinous ligaments and muscle attachment to the C7 spinous process were always preserved.

Comparison of C7 spinal cord decompression area between arcocristectomy and dome laminoplasty. (A) Arcocristectomy. (B) Dome laminoplasty.
The operative procedure causes damage to the posterior cervical muscles, facet joint, and capsule, resulting in a reduction in postoperative cervical ROM. In the present study, either detachment of the muscles attached to the C7 spinous process or the C7 spinous process splitting laminoplasty did not affect cervical mobility more than 2 years after the operation. Among the muscles attached to the C7 spinous process, only the splenius capitis muscle works for extension, flexion, and rotation. Therefore, muscle action may be preserved, and neck mobility may be unaffected by detaching muscles attached to the C7 spinous process [29].
This study has several limitations. Because this was a prospective, single-center study, 31 cases were reviewed and the pathology at the C6–C7 level is an essential factor for the comparison in this study, obtaining a sufficient sample size was challenging. More patients should be included in both groups to make the study more reliable, and the patient data should be compared. In terms of follow-up periods, we routinely recommended visits every 3 months after surgery to all enrolled patients, and many followed up irregularly. Unfortunately, all of the postoperative parameters presented in this study are the results of the surgery 2 years ago. Lamina auto-fusion is one of the complications that can occur after laminoplasty. In the present study, additional evaluation of lamina auto-fusion was required to measure cervical ROM. Furthermore, it is desirable to clearly categorize axial neck pain to understand the origin or cause of neck pain before and after laminoplasty.
Conclusions
In conclusion, the modified open-door laminoplasty with C7 spinous process and posterior structures preserved using C7 arcocristectomy helps reduce axial neck pain.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conception and design: MWK; data acquisition: HES, MWK, JWB; analysis of data: HES, MWK, JWB; drafting of the manuscript: HES, MWK, JWB; administrative support: MWK; and final approval of manuscript: all authors.