Significance of Facet Fluid Index in Anterior Cervical Degenerative Spondylolisthesis
Article information
Abstract
Study Design
Retrospective cohort study.
Purpose
To correlate cervical facet fluid characteristics to radiographic spondylolisthesis, determine if facet fluid is associated with instability in cervical degenerative spondylolisthesis, and examine whether vertebral levels with certain facet fluid characteristics and spondylolisthesis are more likely to be operated on.
Overview of Literature
The relationship between facet fluid and lumbar spondylolisthesis is well-documented; however, there is a paucity of literature investigating facet fluid in degenerative cervical spondylolisthesis.
Methods
Patients diagnosed with cervical degenerative spondylolisthesis were identified from a hospital’s medical records. Demographic and surgical characteristics were collected through a structured query language search and manual chart review. Radiographic measurements were made on preoperative MRIs for all vertebral levels diagnosed with spondylolisthesis and adjacent undiagnosed levels between C3 and C6. The facet fluid index was calculated by dividing the facet fluid measurement by the width of the facet. Bivariate analysis was conducted to compare facet characteristics based on radiographic spondylolisthesis and spondylolisthesis stability.
Results
We included 154 patients, for whom 149 levels were classified as having spondylolisthesis and 206 levels did not. The average facet fluid index was significantly higher in patients with spondylolisthesis (0.26±0.07 vs. 0.23±0.08, p<0.001). In addition, both fluid width and facet width were significantly larger in patients with spondylolisthesis (p<0.001 each). Cervical levels in the fusion construct demonstrated a greater facet fluid index and were more likely to have unstable spondylolisthesis than stable spondylolisthesis (p<0.001 each).
Conclusions
Facet fluid index is associated with cervical spondylolisthesis and an increased facet size and fluid width are associated with unstable spondylolisthesis. While cervical spondylolisthesis continues to be an inconclusive finding, vertebral levels with spondylolisthesis, especially the unstable ones, were more likely to be included in the fusion procedure than those without spondylolisthesis.
Introduction
Degenerative cervical spondylolisthesis is often indolent but can occasionally present with neck or occipital pain and myeloradiculopathy [1]. Although there is no consensus on treatment, some authors suggest that spondylolisthesis with evidence of instability or progressive neurologic involvement is an indication of operative management [1,2]. Magnetic resonance imaging (MRI) is essential in understanding the magnitude of cervical spondylosis in patients with complaints of radiculopathy or myelopathy and providing insight into the type of surgical procedure required to address the underlying disease. However, additional findings on MRI, such as cervical spondylolisthesis, may alter the treatment plan (i.e., the number of levels to be fused) since surgeons may be hesitant to end a fusion construct adjacent to a level with cervical spondylolisthesis.
Several studies have identified specific MRI features, such as intraspinal synovial cyst, facet fluid, and facet orientation, which may be suggestive of spondylolisthesis [3–5]. Extensive literature is available for the lumbar spine which states that the presence of facet fluid is correlated with the likelihood of lumbar spondylolisthesis [5–11]. The presence of excessive facet fluid is measured by the facet fluid index, which is calculated by dividing the combined diameter of facet fluid measurements by the combined facet widths. The facet fluid index is reportedly associated with a higher magnitude of lumbar vertebral slip [5,7]. In the cervical spine, facet characteristics, including facet fluid, tropism, axial inclination, coronal inclination, and sagittal inclination, have been suggested to be associated with cervical spine instability [12,13]; however, these authors acknowledged small sample size as a limitation of their study and recommended the need for a larger cohort analysis [12].
Therefore, the objectives of our study were to (1) correlate cervical facet fluid characteristics to radiographic spondylolisthesis, (2) determine if facet fluid was associated with instability in spondylolisthesis, and (3) examine whether vertebral levels with certain facet fluid characteristics and spondylolisthesis were more likely to require operative management.
Materials and Methods
After obtaining approval from the Institutional Review Board of Thomas Jefferson University (IRB approval no., 19D.493), all patients ≥18 years undergoing anterior cervical discectomy and fusion (ACDF) for primary degenerative cervical spondylolisthesis below C3 at a single academic institution during 2015–2021 were retrospectively identified. The requirement for informed consent from individual patients was omitted due to the retrospective design of this study. The Current Procedural Terminology code ‘22551’ was used to include all patients undergoing ACDF during the selected study period. Exclusion criteria comprised a lack of imaging data, including flexion-extension radiographs and MRI scans taken >1 year apart or >1 year preoperatively, a history of previous cervical spine surgery, congenital deformity of the cervical spine, inflammatory arthritis, and cervical spine fracture or traumatic instability, malignancy, and infection. Based on the patient’s clinical presentation and imaging findings, a diagnosis of myelopathy or radiculopathy was made. The appropriate surgical intervention was planned through shared decision-making between the physician and the patient.
1. Data extraction
Patient demographics and surgical characteristics were collected through a structured query language search and manual chart review of the hospital’s electronic medical records. Demographic information regarding the age, sex, race, ethnicity, body mass index (BMI), smoking status (nonsmoker, current smoker, or former smoker), Elixhauser comorbidity index (ECI), and diabetes status was collected for all patients. Surgical characteristics included levels operated and preoperative diagnosis; the vertebral segment C6–C7 was omitted from the analysis because of inconsistent visualization.
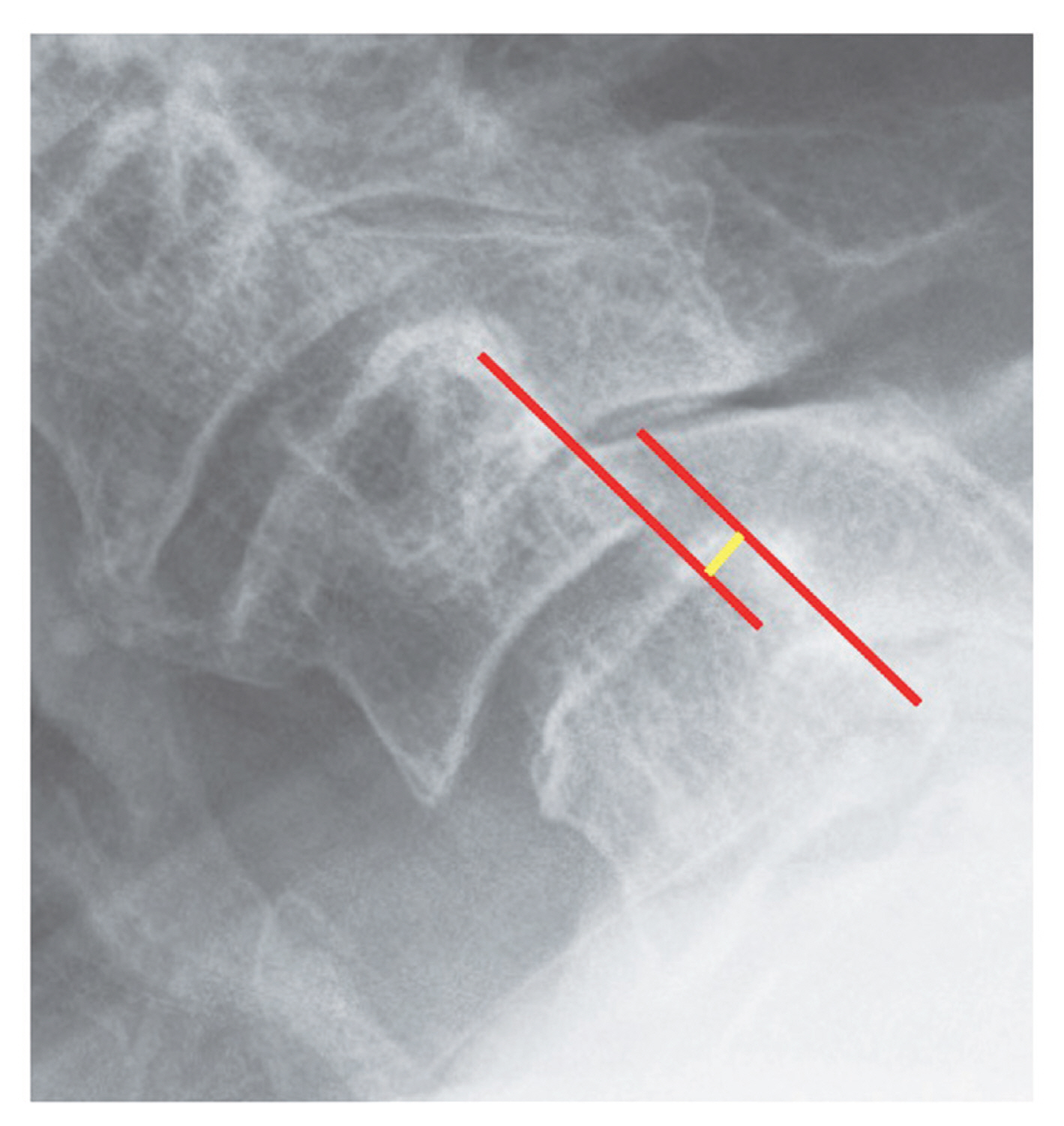
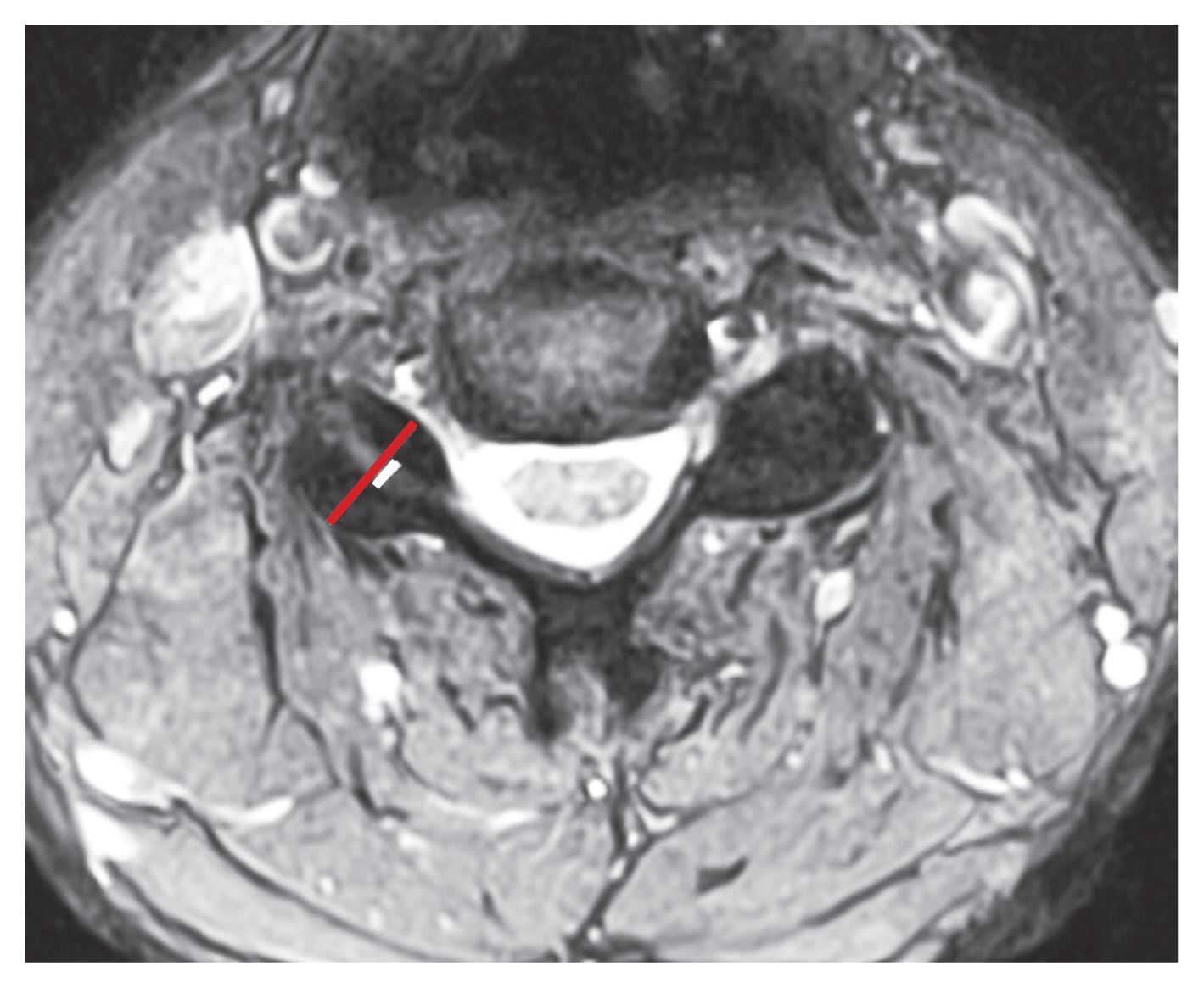
Radiographic data were collected via our institution’s picture archiving and communication system (Sectra AB, Linköping, Sweden). All measurements were made on preoperative radiographs and MRIs for the vertebral levels diagnosed with spondylolisthesis and adjacent undiagnosed levels. The posterior vertebral cortices were referenced on the preoperative flexion-extension radiographs to measure the magnitude of spondylolisthesis by determining the extent (in mm) of anterior translation of the superior vertebra relative to the inferior vertebra (Fig. 1) [5]. Radiographic spondylolisthesis was defined as >3.0 mm anterior translation of a vertebral body relative to its inferior counterpart on a flexion radiograph [14,15]. Instability was defined as a difference of >3.5 mm in vertebral translation between flexion and extension radiographs [2,13,14,16]. Since the axial MRI most clearly demonstrated the facet joints, it was used to determine the average facet fluid index computed by dividing the combined diameter of both facet fluid measurements by the combined diameter of the facet widths on axial MRI (Fig. 2) [5]. Fluid width was measured perpendicular to the apparent joint line [11]; the combined facet widths and combined fluid widths were recorded.
2. Statistical analysis
Descriptive statistics, including means and standard deviation or percentage and frequency, were computed for all patient demographics, surgical characteristics, and radiographic parameters. The Shapiro-Wilk test was used to analyze the normality of each continuous variable; accordingly, parametric data were compared using independent samples t-tests, and non-parametric data using the Mann-Whitney U test. Dichotomous variables were compared using Pearson’s chi-square test. Additionally, a bivariate analysis was used to compare facet characteristics based on radiographic spondylolisthesis and the stability of the affected level. Statistical significance was set at a p-value of <0.05.
Results
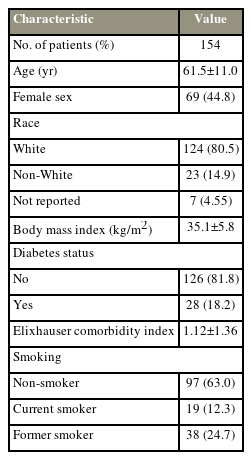
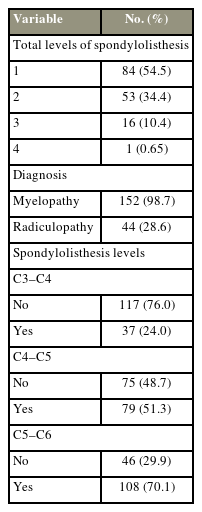
We identified 154 patients with a diagnosis of degenerative cervical spondylolisthesis during the selected study period (mean age, 61.5±11.0 years; mean BMI, 35.1±5.82 kg/m2; mean ECI, 1.12±1.36); 44.8% of these patients were female and 80.5% were White. Approximately 18.2% of the patients were diabetic, and 63.0% were nonsmokers (Table 1). Most patients (54.5%) only had one level of spondylolisthesis involving the C5–C6 level (70.1%); 152 patients (98.7%) had a diagnosis of myelopathy and 44 (28.6%) had a diagnosis of radiculopathy (Table 2).
When assessing all vertebral levels, 149 levels met the criteria for spondylolisthesis, while 206 levels did not. The average facet fluid index was significantly higher in patients with spondylolisthesis (0.25±0.08 versus 0.27±0.08, p<0.031). In addition, both fluid width (4.61±2.58 mm versus 6.19±2.55 mm, p<0.001) and facet width (17.9±7.12 mm versus 23.0±6.66 mm, p<0.001) were significantly larger in patients with spondylolisthesis. However, there was no difference in the presence of facet fluid between levels with and without spondylolisthesis (p=0.611) (Table 3).
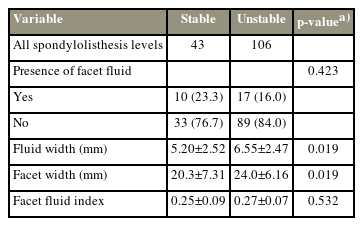
Out of the 149 affected vertebral levels, 106 levels had an unstable spondylolisthesis (>3.5 mm difference between flexion and extension radiographs), while 43 levels did not. Facet width (20.3±7.31 mm versus 24.0±6.16 mm, p<0.019) and fluid width (5.20±2.52 mm versus 6.55±2.47 mm, p<0.019) were significantly larger in patients with instability. However, there was no association between vertebral instability and facet fluid index (p=0.532) or facet fluid presence (p=0.423) (Table 4).
Cervical levels that were included in the fusion construct demonstrated greater fluid width (6.71±2.05 versus 2.42±0.94, p<0.001), facet width (24.2±5.36 versus 11.9±2.00, p<0.001), and facet fluid index (0.21±0.08 versus 0.28±0.06, p<0.001). These levels were also more likely to be levels with spondylolisthesis (p<0.001). Lastly, vertebral levels included in the fusion construct were more likely to have unstable spondylolisthesis than stable spondylolisthesis (76.7% versus 23.3%, p<0.001) (Table 5).
Discussion
As conventional MRI is a static image, it is difficult to use only standard MRI views for diagnosing spondylolisthesis, which has a dynamic component. Therefore, determining surrogates for spondylolisthesis on an MRI may be beneficial when evaluating spinal diseases. Several studies have recommended certain MRI findings that indicate instability; the amount of facet fluid is one such indicator [5–11]. However, most of the literature assessing the role of facet fluid in predicting spinal instability belongs to the lumbar spine, while those studying the cervical spine are limited by sample size.
The presence and magnitude of facet fluid in the lumbar spine correlate with the likelihood of having spondylolisthesis. A retrospective radiographic review by Chaput et al. [11] demonstrated that large facet effusions (>1.5 mm) are highly predictive of degenerative spondylolisthesis at the L4–L5 spinal level, and a clinically measurable amount of facet fluid (>1 mm) should be the cutoff for evaluating spondylolisthesis in the lumbar spine by flexion and extension radiographs. Likewise, Rihn et al. [5] retrospectively analyzed 51 patients and demonstrated that the magnitude of facet fluid, as measured by facet fluid index, is also correlated with the extent of vertebral slip (r=0.90 between facet fluid index and slip percent). In addition, they reported a positive predictive value of 82% for facet fluid and radiographic evidence of anterior translation on flexion radiographs.
Furthermore, the presence of facet fluid in lumbar spine may also contribute to the diagnosis of instability in spondylolisthesis. Cho et al. [17] showed that among patients with diagnosed degenerative spondylolisthesis, 87.3% of patients with a slip of >5 mm or >10° angulation between flexion and extension radiographs had facet fluid compared to only 12.9% of patients with smaller parameter changes. Although other studies have reported lesser association between the various measures of instability, including lumbar spine anterolisthesis (67.5%) and a difference of >5 mm slip or >10° of angulation between flexion and extension radiographs (53.7%) [8,18], these studies do agree that facets with fluid are significantly more unstable than those without. Aggarwal and Garg [10] conducted a meta-analysis including 1,065 patients and concluded that 71% of patients with unstable spondylolisthesis (a difference of >5 mm translation or >10° angulation between flexion and extension radiographs) had facet fluid compared to 22% who did not. The authors also demonstrated that the pooled odds ratio for the predictive value of unstable spondylolisthesis was 7.55 (p<0.001). As a result, many authors recommend flexion-extension radiographs to assess radiographic lumbar spine instability in patients with facet fluid of >1 mm [5,8,10,17].
Unfortunately, no such recommendations can be made for the cervical spine due to the lack of supporting literature. Given the level of evidence available for the lumbar spine, a similar relationship can be presumed for degenerative spondylolisthesis of the cervical spine; nevertheless, because of inherent differences in the cervical and lumbar spines, an independent analysis is essential to assess the relationship between cervical instability and facet fluid. Kulkarni and Sagane [12] retrospectively reviewed 17 patients with degenerative cervical spondylolisthesis and showed that 59% of patients had facet effusion on MRI. In continuation with these results, the present study analyzed a larger cohort to demonstrate that greater fluid width, larger facets, and a higher facet fluid index are associated with cervical spondylolisthesis. We also found that unstable spondylolisthesis (>3.5 mm difference in translation between flexion and extension radiographs) may be associated with larger facet and fluid diameter. These results can be rationalized by understanding the anatomic orientation of cervical facets in the sagittal plane, which is anterosuperior to posteroinferior. Therefore, a reduced sagittal facet angle with respect to the horizontal could hinder the anteroinferior facet’s ability to buttress the posterosuperior vertebrae from an anterior slip [13]. A more horizontal facet would then present on an axial cut of an MRI with a larger facet diameter. Moreover, a horizontally oriented facet would also appear wider in the axial plane, leading to an increased measurement of facet fluid width. Additional research to prospectively assess the relationship between facet characteristics, such as facet diameter and fluid, is warranted to investigate this relationship.
There are no well-established guidelines for the management of cervical degenerative spondylolisthesis [1]. Initial treatment is often conservative and includes pharmacotherapy for pain relief, paraspinal muscle strengthening, and corticosteroid injections [2]. Surgical intervention is often recommended after symptoms of radiculopathy or neurologic deficits fail to respond to conservative treatment or imaging demonstrates spondylolisthesis with instability or spinal cord compression [1]. The decision to surgically intervene is complicated and based on the patient’s clinical symptoms, degree of spondylolisthesis, and magnitude of spinal cord compression. Our study demonstrates that the vertebral levels included in the fusion construct were more likely to have a higher facet fluid index, fluid width, and facet width and those with spondylolisthesis were significantly more likely to be included in the fusion construct. Among vertebrae with spondylolisthesis, the levels demonstrating instability were significantly more likely to be included in the fusion construct than those without instability, indicating greater symptomology.
This study has certain limitations, including those inherent to its retrospective design. Due to varying definitions of instability, our results may not be comparable to studies that defined instability differently. In the present study, instability was measured in the sagittal plane and based on the difference between the translation of the superior vertebrae past the inferior vertebrae on flexion and extension radiographs. This definition does not account for rotational or translational instability that may be present additionally; it is possible that analysis of instability in these directions may demonstrate a different relationship between the magnitude of facet fluid and vertebral instability [19]. Our study may also be underpowered to detect all true relationships between facet characteristics and unstable spondylolisthesis; therefore, additional studies with large cohorts are recommended for further evaluation.
Conclusions
Our study demonstrates that facet fluid index is associated with degenerative cervical spondylolisthesis, while an increased facet size and fluid width are associated with unstable spondylolisthesis. We found that vertebral levels with spondylolisthesis, especially those with instability, were more likely to be included in the fusion construct than those without spondylolisthesis. High-quality retrospective studies and prospective trials are needed to further investigate the relationship between facet characteristics and spondylolisthesis in the cervical spine.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Funding
This study was supported by internal funding from the Rothman Orthopaedic Institute.
Author Contributions
Project conception: YL, MJL; data collection: JCH, NK, BW, PG; statistical analysis: YL, JCH, MJL, NK, BW, PG; first draft writing: JCH; manuscript writing: YL, JJM, JAC, MK, IDK, ASH, ARV, CKK, GDS, JR; manuscript editing: all authors; and final approval of the manuscript: all authors.