A Comparison between Structural Allografts and Polyetheretherketone Interbody Spacers Used in Anterior Cervical Discectomy and Fusion: A Systematic Review and Meta-analysis
Article information
Abstract
Among interbody implants used during anterior cervical discectomy and fusion (ACDF), structural allografts and polyetheretherketone (PEEK) are the most used spacers. Currently, no consensus has been established regarding the superiority of either implant, with US surgeons preferring structural allografts, whereas UK surgeons preferring PEEK. The purpose of this systematic review (level of evidence, 4) was to compare postoperative and patient-reported outcomes between the use of structural allografts PEEK interbody spacers during ACDF. Five electronic databases (PubMed, Embase, Scopus, Web of Science, and Cochrane) were searched for articles comparing the usage of structural allograft and PEEK interbody spacers during ACDF procedures from inception to April 10, 2023. The searches were conducted using the keywords “Spine,” “Allograft,” and “PEEK” and were performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis guidelines. Subsequent quality and sensitivity analyses were performed on the included studies. Nine studies involving 1,074 patients were included. Compared with the PEEK group, the structural allograft group had comparable rates of postoperative pseudoarthrosis (p=0.58). However, when stratified according to the number of levels treated, the 3-level ACDF PEEK group was 3.45 times more likely to have postoperative pseudoarthrosis than the structural allograft group (p=0.01). Subsequent postoperative outcomes (rate of subsidence and change in the preoperative and postoperative segmental disc heights) were comparable between the PEEK and structural allograft groups. Patient-reported outcomes (Visual Analog Scale [VAS] of neck pain and Neck Disability Index [NDI]) were comparable. This study showed that for 3-level ACDFs, the use of structural allografts may confer higher fusion rates. However, VAS neck pain, NDI, and subsidence rates were comparable between structural allografts and PEEK cages. In addition, no significant difference in pseudoarthrosis rates was found between PEEK cages and structural allografts in patients undergoing 1- and 2-level ACDFs.
Introduction
Anterior cervical discectomy and fusion (ACDF) is a well-established treatment for cervical myelopathy and radiculopathy [1–4]. It was first described by Smith and Robinson [4] in 1958, who advocated the use of a structural iliac crest autograft to promote interbody fusion. However, the use of harvested iliac crest grafts has complications and is associated with donor-site morbidities such as pain and surgical site infection [5]. As a result, various alternatives such as interbody cages and structural allografts were developed to mitigate these complications [6].
Among interbody implants, structural allografts and polyetheretherketone (PEEK) are the most commonly used spacers. In a survey comprising 599 AO spine members, 92% utilized structural allograft or PEEK interbody cages during ACDF [7]. However, no consensus has been established regarding the superiority of either implant, with US surgeons preferring structural allografts, where UK surgeons preferring PEEK cages [8].
Previous systematic reviews [9] and meta-analysis [10] have attempted to compare PEEK cages with structural allografts as interbody spacers, and both cervical and lumbar data were combined because of insufficient data. Thus, this review aimed to compare the postoperative clinical and radiological outcomes of PEEK interbody cages with structural allograft interbody implants in ACDF. To the author’s knowledge, this is the first meta-analysis that seeks to compare PEEK cages against structural allografts in ACDF procedures.
Methods
1. Search strategy
The study was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-analysis statement [11]. An electronic database search of PubMed, Embase, Scopus, Web of Science, and Cochrane Central Register of Controlled Trials was performed from inception to April 10, 2023 using keywords relating to spine (spinal OR spine* OR vertebra* OR vertebrae* OR cervical OR “cervical spine*”), ACDF (surgery OR surgeries OR operation* OR surgical OR procedure* OR “cervical fusion” OR “interbody fusion” OR interbody* OR ACDF OR “Anterior Cervical Discectomy and Fusion” OR discectomy* OR diskectomy*), allograft (allograft* OR homograft* OR allotransplant* OR “structural allograft” OR allogenic OR allogeneic OR homologous OR homogenous OR bone transplant* OR bone graft*), and PEEK (PEEK OR polyetheretherketone OR Cage* OR polyetherketone).
2. Data assessment and inclusion and exclusion criteria
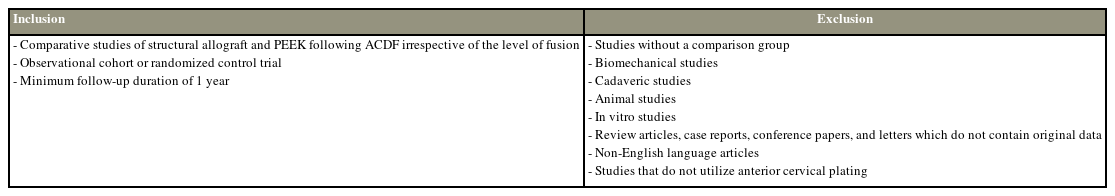
Abstracts were screened to remove duplicates and selected based on the predetermined inclusion criteria (Table 1). The full texts of the remaining studies were further analyzed. The reference lists of the included articles were manually searched to identify further studies for analysis. Any discrepancies were resolved by achieving a consensus with a third author (T.J.H.).
Studies comparing the use of structural allografts with PEEK interbody cages for ACDF were selected. The Newcastle–Ottawa Quality Assessment Scale was used to assess the quality of non-randomized studies in meta-analyses [12]. All nine included studies were of good quality according to the Newcastle–Ottawa Scale, with a range of 7–9 points (Supplement 1).
3. Data collection
Data from the included studies were extracted independently by F.F.J.Y. and L.C.Y. using a standardized protocol and reporting form. Study characteristics (year of study, study design, follow-up duration, and patient demographics) and operative outcomes (pseudoarthrosis, subsidence rates, and segmental disc height) were extracted. The following patient-reported outcomes at baseline and last follow-up were also extracted: Visual Analog Scale (VAS) for neck pain and Neck Disability Index (NDI). When means and standard deviations were unavailable, data were converted using previously established models by Wan et al. [13]. The corresponding authors were not contacted because no data were missing during extraction. The following definitions for operative and patient-reported outcomes were used:
(1) Pseudoarthrosis was defined as (a) no bridging bone seen across the intervertebral space, (b) radiolucent line at the graft vertebral body interface, and (c) motion >1 mm between adjacent spinous processes as seen on flexion–extension cervical spine radiographs in all of the studies [14–18]. Wang et al. [14] further included patients who had a halo appearing around the screws and/or implant failure that could be visualized on radiographs into their definition of pseudoarthrosis.
(2) Subsidence was defined as a radiologic decrease in the intervertebral height of ≥2 mm between the immediate postoperative and final postoperative radiographs [7,17,19,20]. All studies that reported subsidence adopted this definition.
(3) The segmental disc height was defined as either the average of the anterior and posterior intervertebral height [21] or the midpoint of the upper endplate of the vertebral body to the midpoint of the lower endplate of the vertebral body [14,17].
(4) VAS neck pain was reported on a scale of 0–10, where 0 was defined as “no pain,” whereas 10 as “worst pain ever” [22].
(5) Patient disability was measured using NDI, with scores ranging from 0 to 50 points [23].
4. Statistical analysis
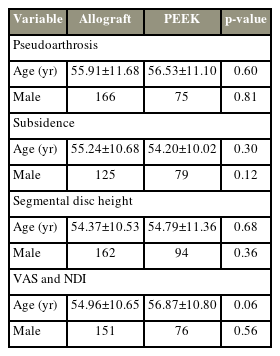
For each measured outcome, baseline variables such as age and sex were statistically compared the structural allograft group and the PEEK group. For these outcome variables, age and sex were not statistically significant between the two groups, indicating that these two variables were comparable at baseline (Table 2). The odds ratio for binary outcomes and the mean difference for continuous outcomes were extracted from the selected studies. Heterogeneity among studies was assessed using the I2 statistic, interpreted according to definitions provided by the Cochrane Handbook, where an I2 value of 0%–50% represents heterogeneity that might not be important and 50%–100% may represent heterogeneity [24]. Statistical significance was considered at p≤0.05. All statistical analyses were made assuming a two-sided test at 5% level of significance using the Review Manager ver. 5.3 (Revman; Cochrane, London, UK). Random-effects models were utilized in all meta-analyses.
Results
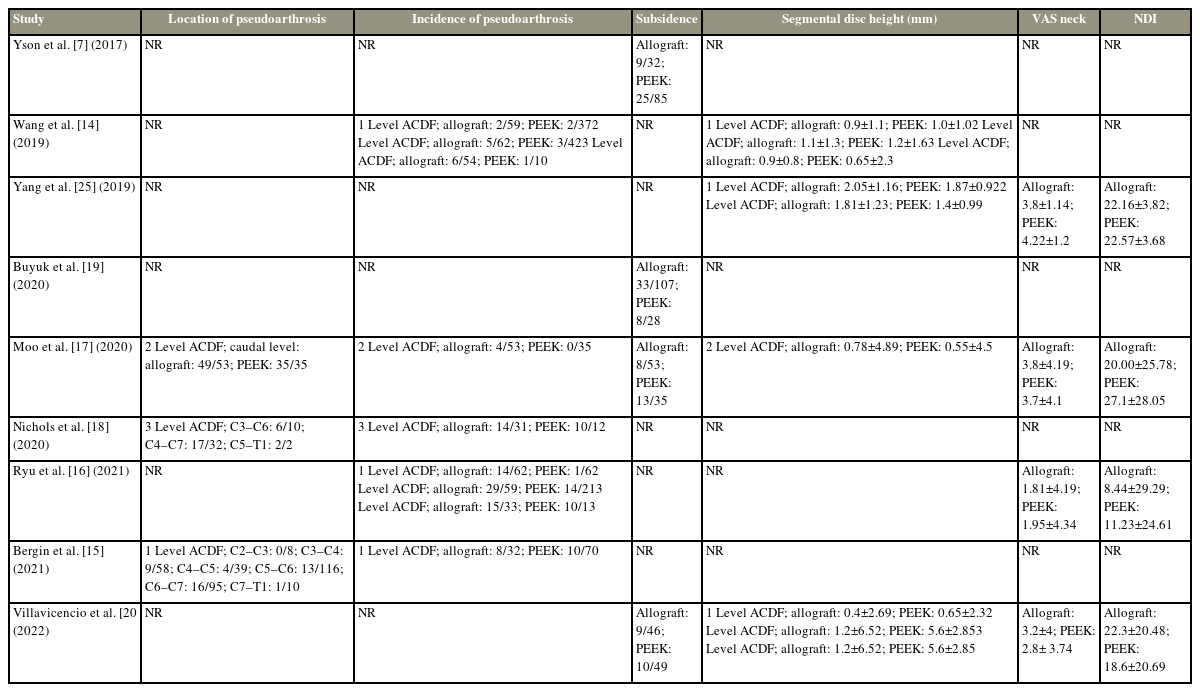
A systematic literature search using our search strategy yielded a total of 5,393 articles, with 2,110 remaining after duplicate removal. Moreover, 2,070 articles were excluded based on the title and abstract review. The remaining 40 articles underwent full-text review, of which nine articles were subsequently included in the meta-analysis (Fig. 1). Five articles were retrospective studies, three were prospective studies, and one was a randomized controlled trial. The study characteristics and clinical outcomes are summarized in Tables 3 and 4, respectively.
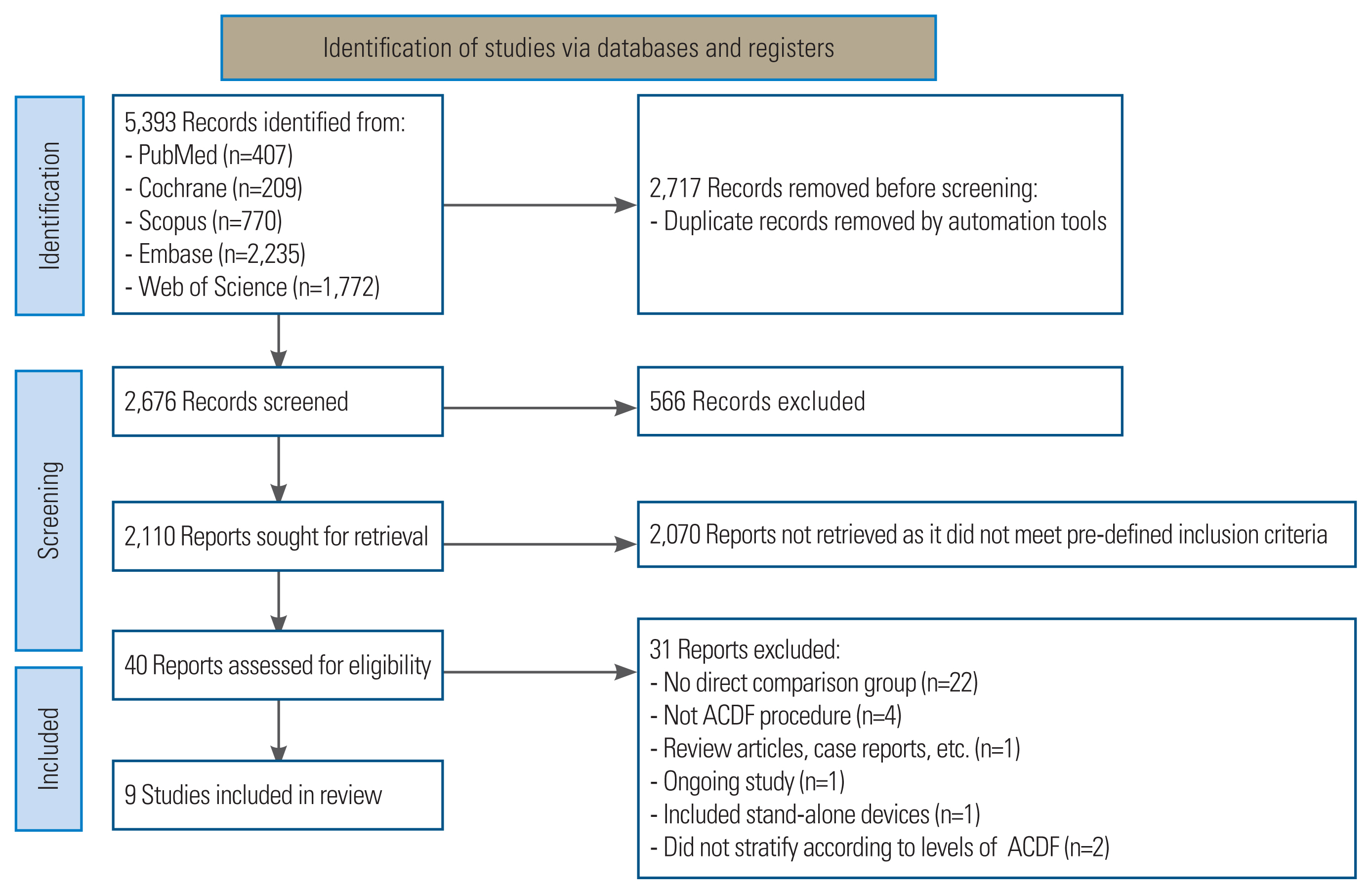
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram. ACDF, anterior cervical discectomy and fusion.
The study included a total of 1,074 patients who underwent ACDF instrumentation for spinal surgery. Of these patients, 667 underwent structural allograft fixation for ACDF, whereas 407 underwent PEEK cage fixation for ACDF. All nine studies included patients who had anterior cervical plating [7,14–20,25]. In general, seven papers did not specify whether bone morphogenic protein (BMP) was utilized [7,15,17–20,25], whereas the remaining two papers stated that none of their patients used BMP [14,16].
Study Characteristics
1. Incidence of pseudoarthrosis
The pooled numbers of patients who had postoperative pseudoarthrosis following instrumentation with structural allografts from five studies involving 445 patients and following instrumentation with PEEK cages from five studies involving 246 patients were 97 and 51, respectively.
In five studies involving 691 patients, the estimated pooled odds ratio of patients who had postoperative pseudoarthrosis between structural allografts and PEEK cages, was 1.33 (95% confidence interval [CI], 0.68–2.59; p=0.40; I2=35%) (Fig. 2). These findings suggest the lack of significant difference in the postoperative pseudoarthrosis rates between the structural allograft group and PEEK groups.
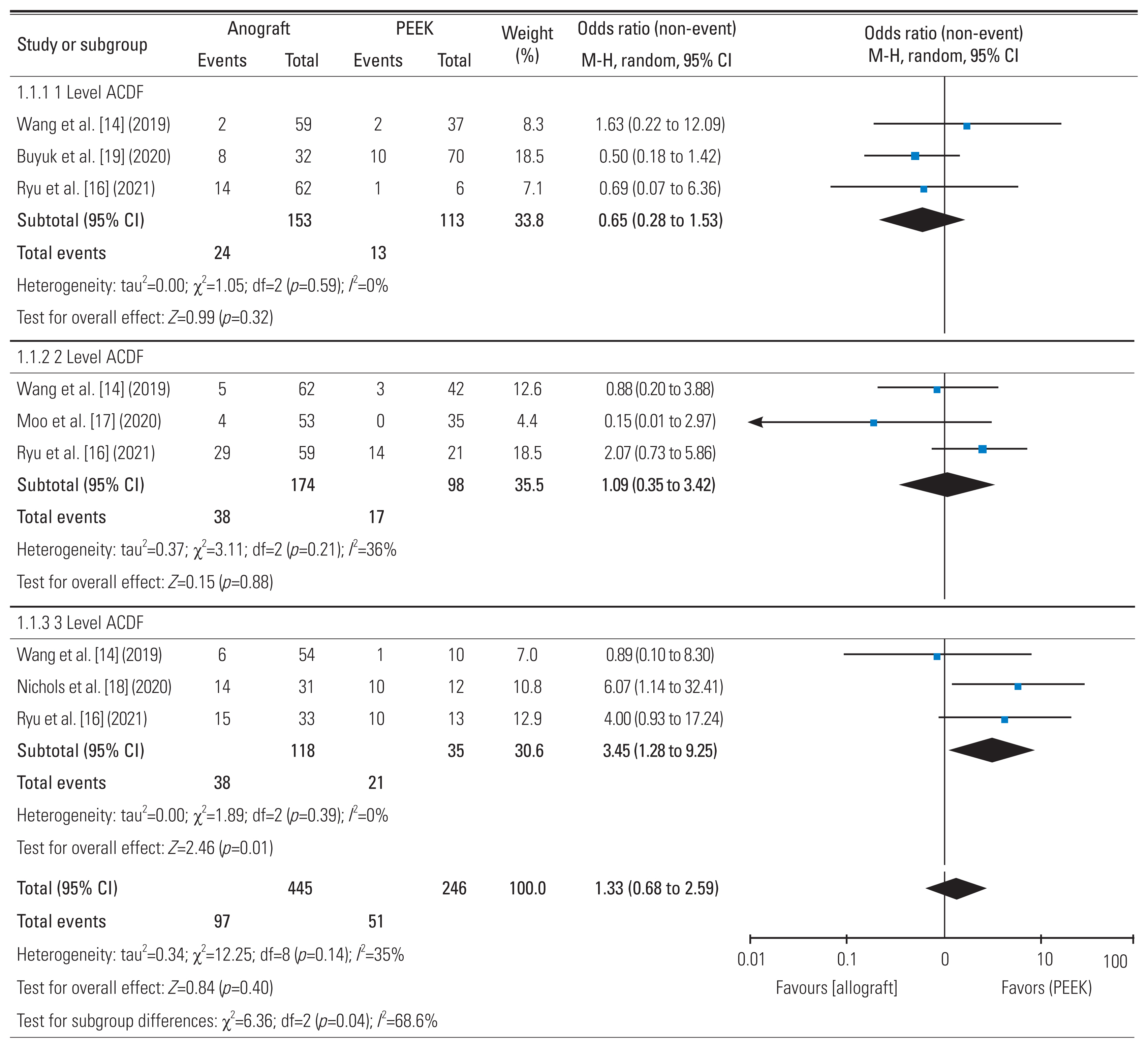
Comparison of pseudoarthrosis rates. PEEK, polyetheretherketone; M-H, Mantel-Haenszel; CI, confidence interval; ACDF, anterior cervical discectomy and fusion; df, degrees of freedom.
In a subgroup analysis of three studies comparing 266 patients who underwent 1-level ACDF, the pooled odds ratio of patients between the structural allograft and PEEK groups that had postoperative pseudoarthrosis was 0.65 (95% CI, 0.28–1.53; p=0.32; I2=0%) (Fig. 2). In a subgroup analysis of three studies involving 272 patients who underwent 2-level ACDF, the pooled odds ratio of patients between the structural allograft and PEEK groups that had postoperative pseudoarthrosis was 1.09 (95% CI, 0.35–3.42; p=0.88; I2=36%) (Fig. 2). In a subgroup analysis of three studies involving 153 patients who underwent 3-level ACDF, the pooled odds ratio of patients between the structural allograft and PEEK groups that had postoperative pseudoarthrosis was 3.45 (95% CI, 1.28–9.25; p=0.01; I2=0%) (Fig. 2).
These findings suggest that pseudoarthrosis rates were comparable between the structural allograft and PEEK groups at 1- and 2-level ACDFs. However, in 3-level ACDF, PEEK cages were 3.45 times significantly more likely to result in pseudoarthrosis than structural allografts.
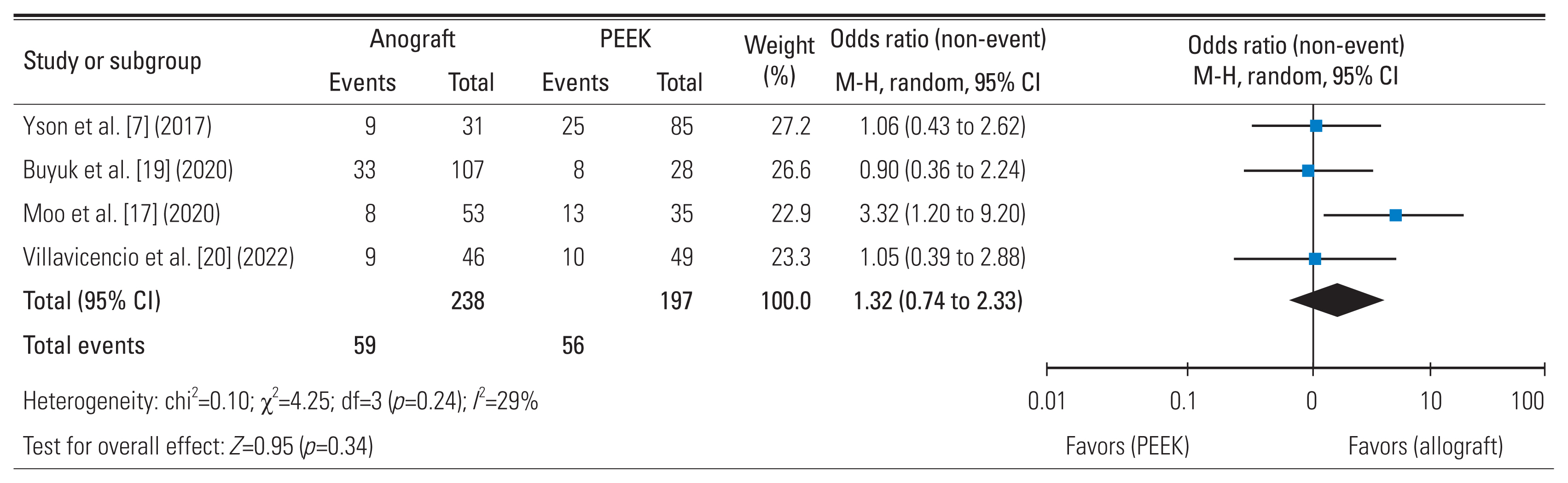
2. Incidence of subsidence
In four studies involving 238 patients, the pooled number of patients who had postoperative subsidence following instrumentation with structural allografts was 59. In four studies involving 197 patients, the pooled number of patients who had postoperative subsidence following instrumentation with PEEK cages was 56.
From the four studies involving 435 patients, the estimated pooled odds ratio of patients in the structural allograft and PEEK group who had postoperative subsidence was 1.32 (95% CI, 0.74–2.33; p=0.34; I2=29%) (Fig. 3). These findings suggest that the subsidence rates were comparable between the structural allograft and PEEK groups.
3. Segmental disc height
In four studies involving 332 patients, the pooled change between the preoperative and postoperative segmental disc heights in the structural allograft group was 1.10±2.59 mm. In four studies involving 222 patients, the pooled change between the preoperative and postoperative segmental disc heights in the PEEK group was 1.71±2.86 mm. In four studies involving 554 patients, the standard difference in the means of the segmental disc height between the structural allograft and PEEK groups was analyzed, giving a pooled estimate of −0.03 (95% CI, −0.42 to 0.36; p=0.89; I2=38%) (Fig. 4).
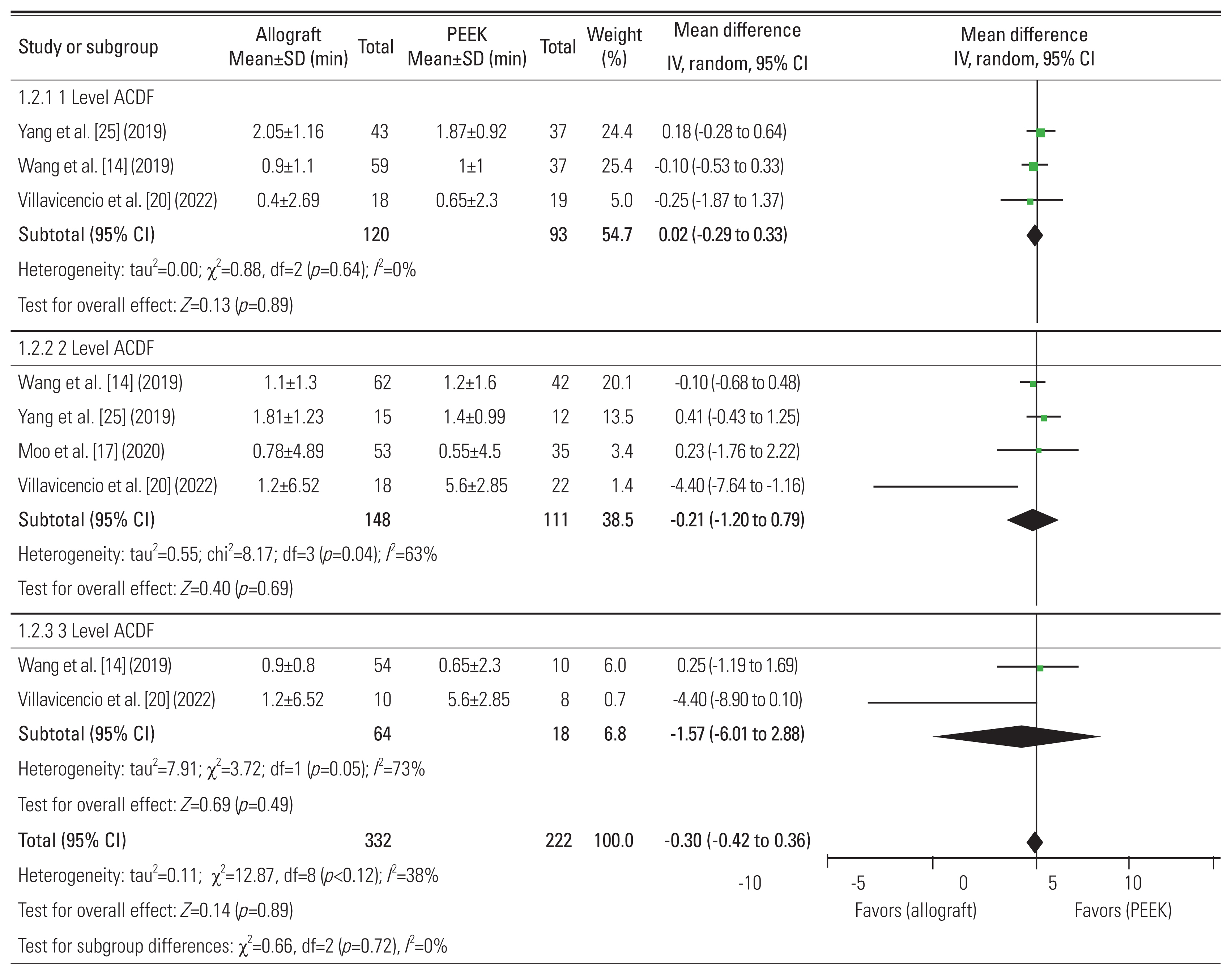
Comparison of postoperative changes in segmental disc height. SD, standard deviation; PEEK, polyetheretherketone; IV, inverse variance; CI, confidence interval; ACDF, anterior cervical discectomy and fusion; df, degrees of freedom.
In a subgroup analysis of three studies comparing 213 patients who underwent 1-level ACDF, the pooled change between the preoperative and postoperative segmental disc heights between the structural allograft and PEEK groups was 0.02 (95% CI, −0.29 to 0.33; p=0.89; I2=0%) (Fig. 4). In a subgroup analysis of four studies involving 259 patients who underwent 2-level ACDF, the pooled change between the preoperative and postoperative segmental disc heights between the structural allograft and PEEK groups was −0.21 (95% CI, −1.20 to 0.79; p=0.69; I2=63%) (Fig. 4). In a subgroup analysis of three studies involving 82 patients who underwent 3-level ACDF, the pooled change between the preoperative and postoperative segmental disc heights in the structural allograft and PEEK groups was −1.57 (95% CI, −6.01 to 2.88; p=0.49; I2=73%) (Fig. 4). These findings suggest that the difference in the preoperative and postoperative segmental disc heights was comparable between the structural allograft and PEEK groups.
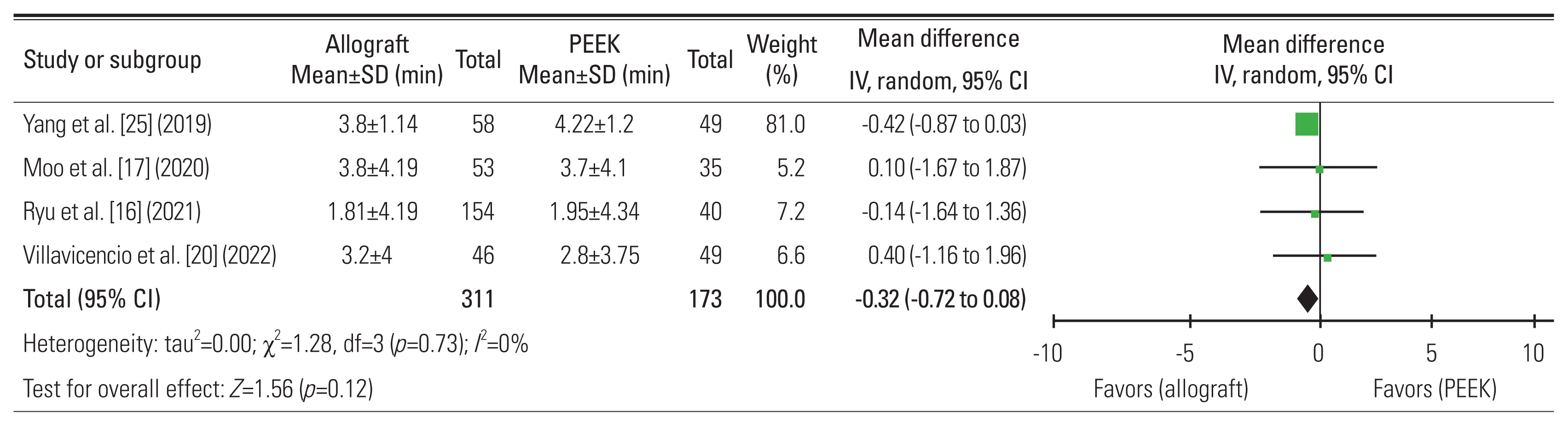
4. VAS neck pain
In four studies involving 311 patients, the pooled change between preoperative and postoperative VAS neck pain scores for the structural allograft group was 2.73±3.88 mm. In four studies involving 173 patients, the pooled change between preoperative and postoperative VAS neck pain scores in the PEEK cage group was 3.19±3.56 mm. In four studies involving 484 patients, the standard difference in the mean VAS neck pain score between the structural allograft and PEEK groups, was analyzed, giving a pooled estimate of −0.32 (95% CI, −0.72 to 0.08; p=0.12; I2=0%) (Fig. 5). These findings suggest that the change in preoperative and postoperative VAS neck pain scores was comparable between the structural allograft and PEEK groups.
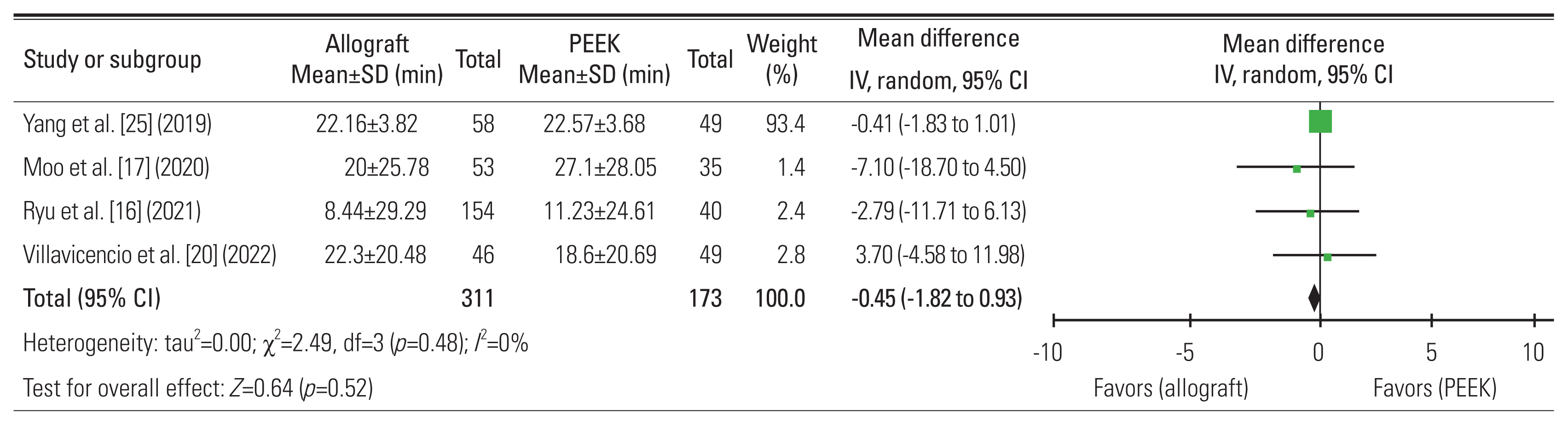
5. NDI
In four studies involving 311 patients, the pooled change between the preoperative and postoperative NDI scores in the structural allograft group was 15.02±25.33 mm. In four studies involving 173 patients, the pooled change between the preoperative and postoperative NDI scores in the PEEK group was 20.30±21.31 mm. In four studies involving 484 patients, the standard difference in the mean NDI score between the structural allograft and PEEK groups was analyzed, giving a pooled estimate of −0.45 (95% CI, −1.82 to 0.93; p=0.52; I2=0%) (Fig. 6). These findings suggest that the change in the preoperative and postoperative NDI scores was comparable between the structural allograft and PEEK groups.
Discussion
PEEK cages are notable for their biocompatibility and corrosion-resistant and radiolucent properties, which enable clear visualization of fusion on radiography [26,27]. However, given its biologically inert property, PEEK cages do not provide osteoinduction, which may increase the risk of pseudoarthrosis and graft subsidence [27–29]. On the contrary, structural allografts have the advantages of better osteoinduction but are associated with possible disease transmission [30] and are more radio-opaque than PEEK, which can make assessment of postoperative fusion challenging.
Pseudarthrosis is not an uncommon complication in ACDF and can be detrimental when it leads to inappropriate segmental motion. Patients may experience postoperative pain, neurological compromise (such as radiculopathy and myelopathy), and hardware failure and may require revision surgery [31]. Thus, this study found that in 1- and 2-level ACDFs, structural allografts and PEEK cages have comparable pseudarthrosis rates. However, in 3-level ACDF, the PEEK group was 3.45 times more likely to have pseudoarthrosis than the structural allograft group. A possible explanation could be PEEK cages’ inherent bioinert property that hinders their ability to achieve adequate osteointegration, subsequently reducing fusion rates [27]. In vitro studies observed that when mesenchymal cells are cultured on PEEK materials, they had significantly high levels of interleukin-1β, which is associated with the formation of fibrous tissues. Furthermore, these mesenchymal cells did not express known markers of bone formation [32]. An in vivo sheep model corroborated these findings, observing that PEEK cages were surrounded by fibrous tissue preventing osteointegration, increasing the risk of pseudoarthrosis [26]. In previous studies, multilevel ACDF was associated with increased rates of pseudoarthrosis compared with 1-level ACDF because of increased bone interfaces required for fusion and altered biomechanics [33–35]. In 1- and 2-level ACDFs, more remaining mobile segments allow for residual cervical spine movement. The strain at the target fusion levels is correspondingly lower, which provides a more conducive environment for fusion. However, in 3-level ACDFs, where six vertebral endplates are prepared for fusion, fewer mobile segments remained. During the arc of motion, the strain experienced in the three immobilized segments is higher, leading to a propensity for pseudarthrosis. Furthermore, with high levels of interleukin-1β induced by the PEEK material, the mesenchymal cells across the six endplates can be biologically “overtaxed,” which results in pseudarthrosis. Thus, these could explain the difference in pseudoarthrosis rates only being observed in 3-level ACDFs. For 3-level ACDFs, one should consider the use of structural allografts instead of PEEK cages to reduce the postoperative risk of pseudarthrosis.
Implant subsidence is not uncommon and occurs in up to 96% postoperatively [36–41]. It is hypothesized to occur in an implant that has a higher Young’s modulus than the native vertebral body [42]. Uncontrolled subsidence may lead to decreased intervertebral disc height and subsequent foraminal narrowing with symptom recurrence. This study found that the incidence and radiological degree of subsidence were comparable between the structural allograft and PEEK groups. When compared with other materials, PEEK cages have significantly lower elastic modulus, resulting in reduced stress shielding, increased bone growth, and hence lower subsidence rates [43]. For instance, titanium cages have significantly higher subsidence rates (20.5%) than PEEK cages (14.3%) [44–46]. Furthermore, carbon fiber-based cages had a higher subsidence rate (25.2%) than PEEK cages (22.8%) [47]. We hypothesize that the comparable subsidence rates between structural allograft and PEEK cages are due to the minimal difference in Young’s modulus between the two materials [48–51]. The elastic modulus of PEEK is approximately 8.3 GPa, which is similar to human cortical bone (17.7 GPa), and lower than that of titanium (116 GPa) [52]. Thus, this minute difference may not result in any clinical difference of subsidence.
In this study, no significant difference in NDI and VAS neck was found between structural allografts and PEEK cages. Patient-reported outcome scores are significantly poorer in patients with pseudoarthrosis requiring revision surgery [53]. In this study, no overall significant difference in fusion rates was found between PEEK cages and structural allografts when comparing all ACDF levels. Given that pseudoarthrosis rates were significantly higher in patients who underwent 3-level ACDF with PEEK cages, patient-related outcome scores may have been lower in patients who underwent PEEK cage insertion in the 3-level ACDF.
This study has several limitations. First, seven of the included articles were retrospective. To minimize the inherent bias of retrospective studies, the NOS scale was utilized to appraise the methodology of each included article. Articles that scored <7 were excluded. The final articles included had a mean score of 8.6 (range, 7–9). Second, some of the included studies have a minimum follow-up period of 1 year. Future studies with longer follow-ups are needed to corroborate our findings. Lastly, data on smoking status we insufficient for analysis, which has significantly increased the risk of pseudoarthrosis in spinal fusions [54].
Conclusions
This study showed that for 3-level ACDF, the use of structural allografts may confer higher fusion rates. However, neck pain VAS, NDI, and subsidence rates were comparable between structural allografts and PEEK cages. In addition, no significant difference in pseudoarthrosis rates was found between PEEK cages and structural allografts in patients undergoing 1- and 2-level ACDFs. Additional evidence of good-quality observational studies with a longer follow-up is needed to support our view of choosing structural allografts over PEEK cages.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Francis Fong Jia Yi and Lim Chee Yit contributed equally and are joint first authors. Francis Fong Jia Yi, Lim Chee Yit, and Tan Jun Hao contributed equally in the conceptualization of the study design and topic, data collection, data extraction, data analysis, and manuscript writing. Dennis Hey contributed in the manuscript writing.
Supplementary Materials
Supplementary materials can be available from https://doi.org/10.31616/2023.0128.
Supplement 1. Assessment of quality of studies included using the Newcastle Ottawa Scale.
asj-2023-0128-Supplementary-1.pdf