Analysis of Rod Fracture at the Lumbosacral Junction Following Surgery for Adult Spinal Deformity
Article information
Abstract
Study Design
Retrospective study.
Purpose
This study aimed to investigate the differences in the characteristics of patients with rod fracture (RF) at the lumbosacral junction from those without RF following adult spinal deformity (ASD) surgery.
Overview of Literature
RF is a major complication following ASD surgery and may require reoperation because of pain and correction loss. The lumbosacral junction is a common RF site. However, risk factors for RFs at the lumbosacral junction remain unknown.
Methods
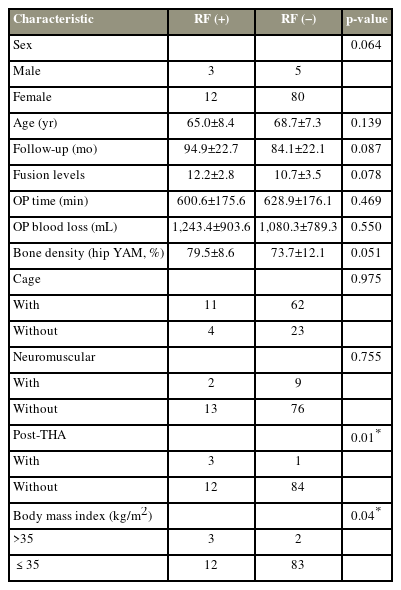
The study included data from 100 patients who underwent ASD surgery between 2012 and 2020. Fifteen of these patients presented with RFs. Patient demographics, clinical outcomes, and radiographic parameters were evaluated in each group.
Results
RFs were significantly more frequent in patients with a medical history of total hip arthroplasty (THA; p=0.01) or severe obesity (p=0.04). However, no significant differences in clinical outcomes, preoperative or postoperative measurements, or changes were found between pre- and postoperative radiographic parameters within the groups. Both pre- (p=0.01) and postoperative (p=0.02) anterior disc heights were significantly greater in the RF group than in the non-RF group. In the RF group, the postoperative lordotic angles of the lumbosacral junction significantly decreased compared with preoperative angles (p=0.02). Multiple logistic regression analysis demonstrated that a THA history (odds ratio, 34.2), severe obesity (odds ratio, 14.0), and preoperative anterior disc height (odds ratio, 1.2) were significant risk factors for RFs.
Conclusions
In this study, the greatest risk factors for postoperative lumbosacral RF after ASD surgery were THA history, severe obesity, and postoperative anterior disc height of ≥10. For patients at higher risk, the use of multirods is considered necessary.
Introduction
Thoracic and lumbar kyphosis and/or scoliosis are adult spinal deformities (ASDs) that present with trunk anterior and/or lateral tilt movements and intermittent claudication for low back and sciatic pain worsening the quality of life (QOL) [1]. For these patients, surgical treatment is an option to improve QOL.
However, surgery for patients with ASD is associated with various mechanical and nonmechanical complications [2]. Mechanical complications can be divided into implant-related and radiographical complications [3]. A typical implant-related complication is a rod fracture (RF); in one study, it accounted for 47% of all implant-related complications [3].
RFs occur in 10%–30% of cases following surgery for ASD, mainly at the lumbosacral junction and three-column osteotomy sites [4–8]. RFs may require reoperation because its development may cause symptoms such as low back pain, buttock pain, and neurological deficits. Despite several studies focusing on pseudarthrosis at the lumbosacral junction, risk factors for RFs at the lumbosacral junction remain unclear [9–13]. Thus, this retrospective study aimed to analyze the differences between patients with and without postoperative RF at the lumbosacral junction.
Materials and Methods
This study was approved by the institutional ethics board of Seirei Sakura Citizen Hospital (approval no., 2020007) and adhered to the declaration of Helsinki. The requirement for informed consent from individual patients was omitted because of the retrospective design of this study.
The database of a single institution was respectively reviewed from April 2012 to September 2020 [14,15]. Patients with ASD were enrolled based on the following inclusion criteria: (1) aged >50 years at the time of surgery, (2) pelvic incidence minus lumbar lordosis (PI–LL) >10°, (3) sagittal vertical axis (SVA) >4 cm, (4) pelvic tilt (PT) >20°, (5) upper instrumented vertebra above T10, (6) S2 alar iliac screws placed distal to the sacropelvic fixation, (7) instrumented with 6.0-mm diameter cobalt chrome dual-rod constructs, and (8) follow-up for at least 2 years. The exclusion criteria were as follows: infections, tumors, and cases that did not require spinal deformity correction, and multirod constructs. Patients who had undergone reconstruction surgery (n=141) were screened, of which 100 (70.9%) were finally enrolled. Through the last follow-up, 15 patients had RF, and 85 had none.
Patient demographics were collected, including age, sex, presence or absence of past medical history considered to be risks for RFs, young adult mean of the femoral neck, operative time, operative blood loss, surgical methods with or without interbody fusion, and fusion level (upper or lower thoracic). Clinical outcomes were assessed using the Oswestry Disability Index (ODI) and the satisfaction score of the Scoliosis Research Society Outcomes Questionnaire (SRS-22 satisfaction) 2 years postoperatively. Neuromuscular disease (e.g., Parkinson’s disease), total hip arthroplasty (THA), and severe obesity (body mass index >35 kg/m2) were considered risk factors for RFs.
Pre- and postoperative radiographic parameters, including coronal Cobb angle, thoracic kyphosis, lumbar lordosis (LL), PI–LL, PT, and SVA were measured. The pre- and postoperative L5–S1 disc angles and anterior disc heights were measured by computed tomography (CT).
Statistical analysis was performed using IBM SPSS Statistics ver. 26.0 (IBM Corp., Armonk, NY, USA). The p-values were based on the Mann-Whitney test, and p-values <0.05 were considered significant.
Results
After surgery, RFs were observed in one patient (6.7%) in 1 year, 9 (60.0%) in 2 years, and 15 (100%) in ≥3 years. Patient demographics were analyzed in each group (Table 1). THA history (p=0.01) and severe obesity (p=0.04) were significantly greater in the RF group. Other demographic data were not significantly different between the two groups. There were no between-group differences in preoperative, postoperative, or changes were found between pre- and postoperative radiographic parameters (Table 2).
Changes between pre- and postoperative L5–S1 disc angles were lower (−1.7° versus 0.2°, p=0.027), the preoperative anterior disc height was higher (11.2 mm versus 8.9 mm, p=0.017), and the postoperative anterior disc height was higher (12.2 mm versus 10.3 mm, p=0.026) in the RF group. Other parameters were not significantly different (Table 3).
The receiver operating characteristic (ROC) curves were used to determine the cutoff values for the changes between pre- and postoperative L5–S1 disc angles (−2.5°), preoperative anterior disc height (10.2 mm), and postoperative anterior disc height (10.5 mm). The areas under the ROC curve for pre- and postoperative changes in the L5–S1 disc angle, preoperative anterior disc, and postoperative anterior disc height were 0.679±0.071, 0.694±0.065, and 0.681±0.072, respectively (Fig. 1). Multiple logistic regression analysis indicated that THA (odds ratio [OR], 34.2; 95% confidence interval [CI], 2.8–410.9; p=0.005), severe obesity (OR, 14.0; 95% CI, 1.8–108.5; p=0.011), and preoperative anterior disc height (OR, 1.2; 95% CI, 1.0–1.4; p=0.027) significantly affected the incidence of RFs. Other variables were not statistically associated with RFs.

Receiver operating characteristic (ROC) curves for changes between pre- and postoperative L5–S1 disc angle (A), preoperative anterior disc height (B), and postoperative anterior disc height (C). The cutoff values for changes between pre- and postoperative L5–S1 disc angle (−2.5°), preoperative anterior disc height (10.2 mm), and postoperative anterior disc height (10.5 mm) were determined by the largest angle of “sensitivity–(1–specificity)”. The area under the ROC curve of changes between pre- and postoperative L5–S1 disc angle was 0.679±0.071, for preoperative anterior disc height was 0.694±0.065, and for postoperative anterior disc height was 0.681±0.072.
ODI and SRS-22 satisfaction were used to evaluate clinical outcomes at the final follow-up. In both groups, the ODI (1.1±0.9 versus 1.3±0.9, p=0.583) and SRS-22 satisfaction (3.8±0.6 versus 3.6±0.8, p=0.477) were comparable.
Five patients underwent revision surgery with continuous low back and/or buttock pain and local kyphosis at the RF site (Fig. 2). Ten patients received nonoperative treatment (Fig. 3). Of those 10 patients, eight were asymptomatic. One patient complained of temporary low back pain without local kyphosis at the RF site and chose nonoperative treatment, and the pain improved with conservative treatment. One patient complained of continuous low back pain with local kyphosis at the RF site; however, reoperation was canceled because of cerebral infarction immediately before the operation. The follow-up period was significantly longer in the reoperation group. No differences in patient demographics, radiographic parameters, L5–S1 disc angles, anterior disc height, or clinical outcomes were found between groups other than the follow-up period (Tables 4, 5).

A 55-year-old woman presented with adult spinal deformity (rod fracture [RF] group, with revision surgery). (A) Preoperative X-rays revealed severe lumbar kyphosis. She was severely obese with a body mass index greater than 35 kg/m2, and preoperative anterior disc height was 14.3 mm. (B) Postoperative radiographs show correction of the severe kyphosis. (C) Two years postoperatively, bilateral RFs were found at L5/S1 with proximal junctional kyphosis (PJK). She complained of severe low back pain and loss of correction associated with the RF and PJK. (D) Revision surgery was performed for RF and PJK, and low back pain was improved.
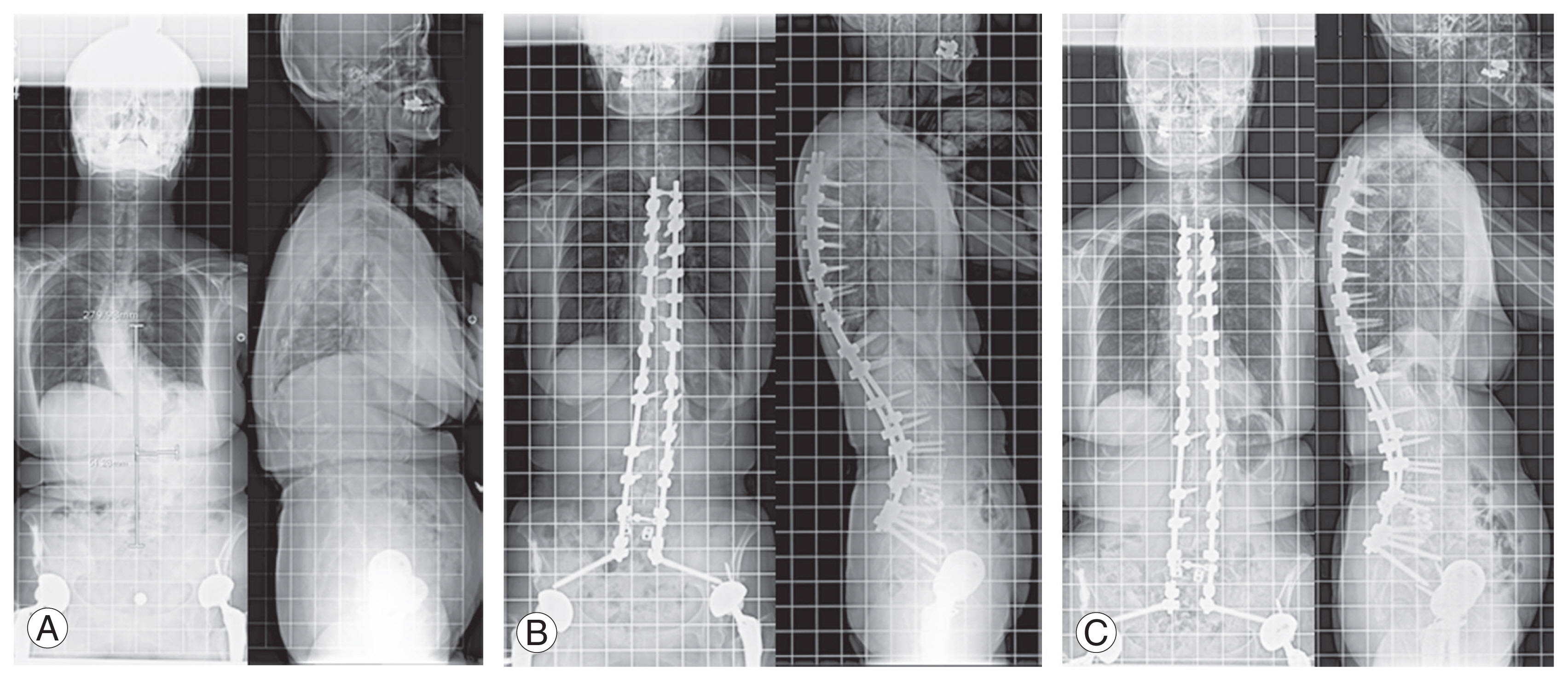
A 61-year-old woman presented with adult spinal deformity (rod fracture [RF] group, no revision surgery). (A) Preoperative X-rays revealed severe kyphoscoliosis. She had previously undergone bilateral THA, and preoperative anterior disc height was 11.0 mm. (B) Postoperative radiographs showed that the severe kyphoscoliosis had been corrected. (C) Three years postoperatively, bilateral RFs were found at L5/S1, although there was no complaint and no loss of correction associated with the RF.
Discussion
The high rates of pseudarthrosis and implant complications at the lumbosacral junction following ASD surgery have been reported [5,8]. Loosening of the S1 screws was an issue; however, this became less of a problem with sacropelvic fixation (e.g., iliac and S2 alar iliac screws) and interbody fusion at L5–S1 [5]. However, as rigid sacropelvic fixation was achieved, an excessive load was applied to the rods in the lumbosacral junction, increasing the risk of RFs [5]. In some cases, diagnosing pseudarthrosis is difficult because of interbody fusion or facet joint fusion using CT. However, the RF site was diagnostic of pseudarthrosis; thus, we focused on RFs.
RFs are among the most common implant-related complications of ASD surgery [3], with an incidence of 10%–30%, and 50%–60% of those require reoperation. RFs requiring reoperation may cause pain and/or loss of correction. The most common RF sites were reported to be the lumbosacral junction and the 3CO sites [4–8]. However, these results included RF cases in areas other than the lumbosacral junction.
Several studies have focused on pseudarthrosis at the lumbosacral junction [9–13]. Pseudarthrosis at the lumbosacral junction occurs in approximately 15.6%–46.9% of cases, and most cases present with RFs at L5–S1. Risk factors for pseudarthrosis at the lumbosacral junction included large PI, revision surgery, failure to restore the optimal sagittal balance, and older age [9,10,13]. In the present study, we focused on patients aged ≥50 years with sagittal plane deformity who underwent ASD surgery including lumbosacral fusion. Our results indicate that THA, severe obesity, and preoperative anterior disc height of ≥10 mm are the greatest risk factors for RFs. In addition, postoperative anterior disc height of ≥10 mm and a postoperative decrease in lumbosacral lordosis angle are also risk factors. To the best of our knowledge, no studies have reported the intervertebral disc height, so our results have unique features. Our results suggested that pseudoarthrosis and RFs are caused by global mechanical stress rather than by fusion biology [12]. Patients with long spinal fusion to the pelvis demonstrated less adaptability of the lumbosacral junction with a critical effect on the hip–spine biomechanics. Specifically, the ability to compensate in the standing-to-sitting transition was significantly affected in patients with THA undergoing long spinal fusion to the sacrum [16]. In addition, severe obesity and larger intervertebral disc height increased stresses on the rod, particularly at the lumbosacral junction on the most caudal side of fixation. In these cases, higher mechanical forces are applied at the lumbosacral junction; thus, prevention strategies for RFs are necessary.
In recent years, multirod constructs have been reported as a prevention strategy for RFs [17]. Multirod constructs show improved biomechanical stability compared with standard dual-rod constructs. However, multirod constructs complicate the surgical procedure, extend the operative time, and can result in the protrusion of the rods and connectors, particularly in the sacral area [18,19]. Our results suggest that the patients with risk factors for RFs may benefit from multirod or dual-rod constructs in ASD surgery.
Groups with or without interbody fusion were compared; however, no difference was found between the two groups. Posterior lumbar interbody fusion using polyether ether ketone cages was performed for cases requiring interbody fusion. Laminectomized local autologous bone graft was used in all cases. The iliac bone and other materials such as the demineralized bone matrix and bone morphogenetic protein were not used. Facet fusion and posterolateral fusion using local autologous bone graft were performed on patients who did not require interbody fusion. Expectedly, interbody fusion would make a difference if the RF was caused by global mechanical stress. The lack of differences was due to our general practice of performing interbody fusion at the lumbosacral junction following ASD surgery. In cases where interbody fusion was not performed, the disc heights were so small that would not allow cage insertion. This reduced the mechanical stress on the rod. We considered this a limitation of this retrospective study. Several studies have reported that interbody fusion was an important factor in RFs and pseudarthrosis [5,11,19], and that the cage material made a difference [11]. We agree with these opinions and mainly performed interbody fusion at the lumbosacral junction following ASD surgery.
The indications for reoperation following RFs vary depending on the surgeons and previous literature. Smith et al. [6] reported that 12 of 18 patients with RFs underwent reoperation. Six patients without reoperation had no apparent clinical symptoms attributed to RFs. Yamato et al. [7] reported that 36 of 54 patients with RFs underwent reoperation. Of the 18 patients who did not, 17 reported no additional symptoms and minimal alignment changes. In the present study, five of 15 patients with RFs underwent reoperation. All patients had continuous back and/or buttock pain and progression of local kyphosis at the RF site. Of the 10 patients who did not undergo reoperation, eight were asymptomatic and found incidentally during routine radiographic follow-up. One of the two patients who were symptomatic had continuous low back pain, but had no local kyphosis, and the pain improved with medication. The other patient who was symptomatic had continuous low back pain and local kyphosis and planned to undergo reoperation; however, the reoperation was canceled because of a cerebral infarction immediately before the operation. Based on these results, immediate reoperation is not indicated for asymptomatic RFs. If the pain is present, but local kyphosis is not observed, improvement can be expected with medication alone.
This study has some limitations. First, this is a retrospective study with a small sample size. Other factors may be identified as the number of cases increases. Second, there may be risk factors other than those identified here. More prospective studies are needed to validate our results.
Conclusions
In this study, 15 of 100 patients who underwent ASD surgery had RFs at the lumbosacral junction. The greatest risk factors for lumbosacral RFs after ASD surgery were THA history, severe obesity, and preoperative anterior disc height of ≥10 mm. A postoperative anterior disc height of ≥10 mm and a decrease in the postoperative lumbosacral lordosis angle were also moderate risk factors. For patients with THA, severe obesity, and preoperative anterior disc height of ≥10 mm, the use of multirods is considered necessary.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conceptualization: TS; methodology: TS; resources: TS, TK, YI, TA, SM; investigation: TS, TK, YI, TA, SM; formal analysis: TS; drafting of the manuscript: TS; project administration: TS, TK; supervision: TK, YI, TA, SO, SM; and final approval of the manuscript: all authors.