A Comparison of Short-Term Outcomes after Surgical Treatment of Multilevel Degenerative Cervical Myelopathy in the Geriatric Patient Population: An Analysis of the National Surgical Quality Improvement Program Database 2010–2020
Article information
Abstract
Study Design
Retrospective review of the American College of Surgeons-National Surgical Quality Improvement Program database from 2010 to 2020.
Purpose
To compare the short-term complication rates of anterior cervical decompression and fusion (ACDF), posterior cervical laminoplasty (LP), and posterior cervical laminectomy and fusion (PCF) in a geriatric population.
Overview of Literature
The geriatric population in the United States has increased significantly. Degenerative cervical myelopathy (DCM) is caused by cervical spinal stenosis, and its prevalence increases with age. Therefore, the incidence of multilevel DCM requiring surgical intervention is likely to increase. ACDF, LP, and PCF are the most commonly used surgical techniques for treating multilevel DCM. However, there is uncertainty regarding the optimal surgical technique for the decompression of DCM in geriatric patients.
Methods
Patients aged 65 years who had undergone either multilevel ACDF, LP, or PCF for the treatment of DCM were analyzed. Additional analysis was performed by standardizing the data for the American Society of Anesthesiologists classification scores and preoperative functional status.
Results
A total of 23,129 patients were identified. Patients with ACDF were younger, more often female, and preoperatively healthier than those in the other two groups. The estimated postoperative mortality and morbidity, mean operation time, and length of hospital stay were the lowest for ACDF, second lowest for LP, and highest for PCF. The readmission and reoperation rates were comparable between ACDF and LP; however, both were significantly lower than PCF.
Conclusions
PCF is associated with the highest risk of mortality, morbidity, unplanned reoperation, and unplanned readmission in the short-term postoperative period in patients aged 65 years. In contrast, ACDF carries the lowest risk. However, some disease-specific factors may require posterior treatment. For these cases, LP should be included in the preoperative discussion when determining the ideal surgical approach for geriatric patients.
Introduction
The American geriatric population has grown significantly in recent years. Between 2009 and 2019, the number of Americans aged ≥60 years increased by 34%, whereas the number of Americans aged 45–64 years increased by only 4% [1]. Furthermore, the older population became increasingly older [1]. The geriatric population aged ≥80 years is projected to make up 4.3% of the population by 2050, which is nearly a fivefold increase from the current population [2]. In addition, the number of Americans aged ≥90 years is projected to quadruple during a similar timeframe [3].
As a result, the number of spine surgeries performed in the older population will undoubtedly increase. The geriatric patient population often has medical comorbidities, which puts them at higher risk of perioperative complications and mortality [4]. Such complications increase healthcare utilization, particularly inpatient care [5]. Therefore, the differences in postsurgical outcomes and complications in older patients must be elucidated to adequately prepare for this demographic change and optimize the surgical care of this increasing population subgroup.
Degenerative cervical myelopathy (DCM) is a spinal cord dysfunction due to spinal canal stenosis caused by degenerative disease [6]. Its prevalence increases with age, and DCM has become a major public health concern with the projected demographic shift [6–9]. DCM includes cervical spondylotic myelopathy, ossification of the posterior longitudinal ligament, ossification of the ligamentum flavum, and degenerative disc disease [6,10]. Without proper treatment, these degenerative changes can lead to permanent disability resulting from myelopathy [6]. Patients with DCM may experience a wide spectrum of symptoms, including upper limb neurological deficits, gait instability, sphincteric disturbance, and ultimately spastic quadriparesis [11,12]. These profound effects of DCM result in worse functional abilities and quality of life compared with cancer or myocardial infarction [13].
Studies have repeatedly demonstrated long-term quality of life and functional improvements after surgery for DCM [14–18]. Even for patients with mild DCM, the AOSpine and Cervical Spine Research Society guidelines recommend consultation with a spine surgeon because based on the natural history of DCM, 20%–60% of patients will eventually experience neurological deterioration without surgical intervention [7,18]. Anterior cervical discectomy and fusion (ACDF), cervical laminoplasty (LP), and posterior cervical laminectomy and fusion (PCF) are the most commonly used procedures, and several factors must be considered when deciding on the surgical approach [8]. However, the optimal surgical technique remains controversial and largely depends on the surgeon’s preference and the patient’s anatomy, stenosis level, and sagittal alignment.
In the context of the aging US population, this study aimed to evaluate and compare postsurgical complications and mortality of patients with DCM aged 65 years who underwent ACDF, LP, or PCF. Based on the results of prior studies comparing different surgical approaches for the treatment of DCM, we hypothesized that patients aged >65 years would not have significantly different complications or mortality among these different surgical techniques [19,20].
Materials and Methods
1. Materials and methods
The National Surgical Quality Improvement Program (NSQIP) collects approximately 300 clinical variables, including preoperative demographics, pre- and postoperative laboratory values, intraoperative factors, and 30-day postoperative outcomes, such as estimated mortality and morbidity. The HIPAA (Health Insurance Portability and Accountability Act)-compliant participant use data files (PUFs) from 2010 to 2020 consist of nearly nine million patient cases from over 700 medical institutions. Institutional Review Board approval is not necessary for studies using this database. The requirement for informed consent from individual patients was omitted because of the retrospective design of this study using de-identified data.
2. Data collection
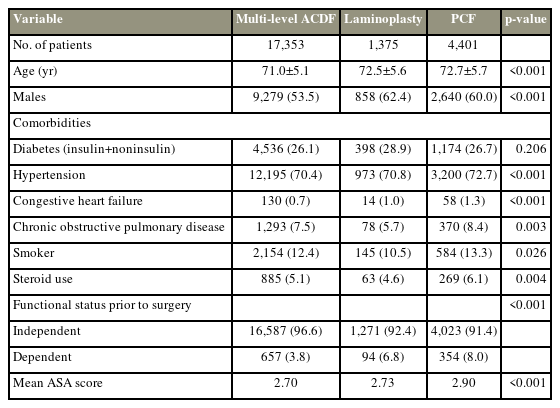
In this study, NSQIP patient cases from 2010 to 2020 were included. Individual PUF files were merged using IBM SPSS Statistics for Windows ver. 28.0 (IBM Corp., Armonk, NY, USA), and variable coding was standardized to ensure proper statistical analysis. Initial inclusion criteria were adult (≥65 years) patients who had undergone surgical procedures including posterior cervical laminectomy and instrumented fusion, multilevel (≥2) ACDF, or LP for the treatment of DCM. Patients were stratified into three cohorts for comparative analysis (Table 1). (1) ACDF: 22551 (arthrodesis anterior interbody decompression cervical below C2) with a concomitant code of 22552 (for each additional interspace, cervical below C2). Only patients with codes 22551 and 2255 were included to ensure a multilevel ACDF. (2) LP: 63050 (LP, cervical, with decompression of the spinal cord, ≥2 vertebral segments) or 63051 (LP, cervical, with decompression of the spinal cord, ≥2 vertebral segments; with reconstruction of the posterior bony element). (3) PCF: 22600 (arthrodesis, posterior or posterolateral technique, single level; cervical below the C2 segment). Stratification into these cohorts is similar to that in previous studies [21,22].
3. Independent variables
Patient demographics, including age and sex, were extracted from the NSQIP database. Comorbidities included functional health status before surgery (independent versus partially/totally dependent), American Society of Anesthesiologists (ASA) physical status classification, diabetes with oral agents or insulin, hypertension requiring medication, congestive heart failure (CHF) within 30 days before surgery, history of severe chronic obstructive pulmonary disease (COPD), smoking status within 1 year, and steroid use for chronic conditions. These variables were extracted directly from the NSQIP database, except functional status before surgery, which was recoded to merge “partially dependent” and “totally dependent” and ASA classification, which was extracted as a numerical variable, thus excluding the descriptor to allow further statistical analysis.
4. Postoperative outcome and complication variables
Dependent variables in the NSQIP are collected up to 30 days after an operation. The outcome variables extracted for this study included estimated mortality, estimated morbidity, reoperation, readmission, operation time (mins), and length of hospital stay (days). The variables for complications included superficial incisional surgical site infection (SSI), deep incisional SSI, pneumonia, unplanned reintubation, pulmonary embolism, deep vein thrombosis, urinary tract infection (UTI), bleeding requiring transfusion, stroke, sepsis, septic shock, cardiac arrest requiring cardiopulmonary resuscitation, myocardial infarction), progressive renal insufficiency, and acute renal failure (AKI).
5. Statistical analysis
For comparative analysis, chi-square and analysis of variance (ANOVA) tests were used for categorical and continuous variables, respectively. Additional ANOVA and chi-square analysis were performed by standardizing data for ASA classification scores and functional status before surgery (independent and dependent cohorts). Multiple comparisons (post-hoc comparisons) between cohorts were conducted using Tukey’s test. Statistical significance was defined as p-value of <0.05. IBM SPSS software (IBM Corp.) was used for all statistical analyses.
Results
A total of 23,129 patients aged 65 years were included among the three surgical groups, including 17,353 multilevel ACDF cases, 1,375 LP cases, and 4,401 PCF cases. The ACDF group was younger (71.0 years old) than the LP group (72.5 years old, p<0.001) or PCF group (72.7 years old, p<0.001). The ACDF group had a predominance of female patients (46.5%) compared with the LP (37.6%, p<0.001) and PCF (40.0%, p<0.001) groups. The PCF group generally had a higher burden of medical comorbidities, including higher ASA scores, hypertension, CHF, COPD, and chronic steroid use. The ACDF group was more often functionally independent (96.6%) before surgery than the LP (92.4%, p<0.001) and PCF (91.4%, p<0.001) groups. The ACDF (12.4%, p<0.001)) and PCF (13.3%, p<0.001) groups included more prior/current smokers than the LP group (10.5%). No significant differences were observed with diabetes between the groups (Table 2).
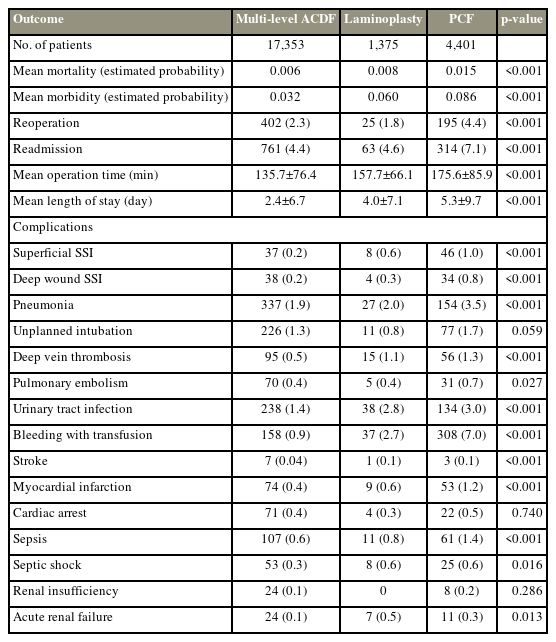
The overall postoperative mortality and morbidity were significantly different between the treatment groups: ACDF with the lowest probabilities (0.6% and 3.2%, respectively), LP (0.8% and 6%, respectively) being the second, and PCF (1.5% and 8.6%, respectively), with the highest. Similarly, the mean operation time and mean length of stay (LOS) were the shortest for ACDF (135.7 minutes and 2.4 days, respectively), followed by LP (157.7 minutes and 4.0 days, respectively), and the longest for PCF (175.6 minutes and 5.3 days, respectively) (Table 3).
No difference was found in the readmission and reoperation rates within 30 days postoperatively between ACDF (4.4% and 2.3%, respectively) and LP (4.6% and 1.8%, respectively). However, the PCF group showed significantly higher readmission and reoperation rates (7.1% and 4.4%, respectively; p-values <0.001) than the ACDF and LP groups (Table 3).
Individual complication rates were not significantly different between the ACDF and LP groups, with a few exceptions, including AKI, UTI, and transfusion. In particular, the incidence rates of superficial SSI, deep SSI, and pneumonia did not differ between the ACDF and LP groups; however, they were significantly more frequent after PCF than after the other two treatments. PCF demonstrated significantly higher rates than ACDF in most of the individual complications, except for unplanned intubation, progressive renal insufficiency, and AKI (Table 3).
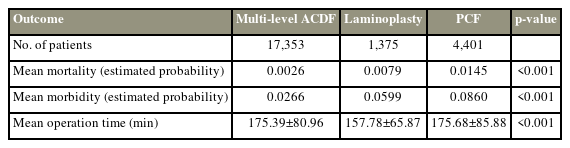
When ASA classification scores were standardized between the cohorts, the mean mortality was still the highest in PCF (1.5%, p<0.001) and lowest in ACDF (0.26%, p<0.001). The mean morbidity was also the highest in the PCF group (8.6%, p<0.001) and the lowest in the ACDF group (2.7%, p<0.001). The mean operation times were the highest in the PCF group and the lowest in the LP group (175.68 minutes versus 157.78 minutes, p<0.001) (Table 4).
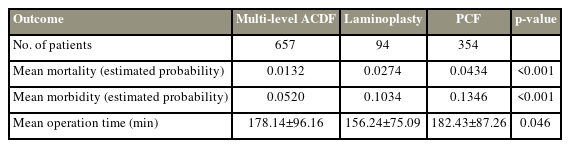
When the preoperative functional health status was held constant, the mean mortality and morbidity were the highest in the PCF group and the lowest in the ACDF group (p<0.001). In patients with independent functional status, the mean operation times were the highest in the PCIF group and the lowest in the ACDF group (174.92 minutes versus 149.22 minutes, p<0.001). In patients with dependent functional status, the mean operation times were highest in the PCF group and the lowest in the LP group (182.43 minutes versus 156.24 minutes, p<0.001) (Tables 5, 6).
Discussion
ACDF, LP, and PCF are the most commonly performed surgical techniques for treating multilevel DCM. Generally, this approach aims to decompress the source of myelopathy and is determined by preoperative imaging findings [23]. However, multiple pathologies often coexist, and the optimal surgical technique remains controversial because of the lack of disparate evidence in clinical outcomes among them. In addition, the indications for each procedure may differ based on several factors, such as the number of levels involved, cervical alignment, disease pathology, surgeon preference, and patient’s age.
In 2013, Fehlings et al. [20] reported the outcomes of a multicenter prospective trial that evaluated 264 patients who had undergone either anterior or posterior surgery for DCM. Moreover, 169 patients were treated anteriorly and 95 posteriorly. They found that patients demonstrated significant improvements with either the anterior or posterior approach. No significant difference was noted in the complication rates between the groups despite the posterior cohort undergoing a greater number of cervical levels. Postoperative functional improvement in both groups at 12 months was equivalent. Certain complications were specific to each group (i.e., dysphagia from the anterior approach); however, this did not significantly affect the functional outcomes. Importantly, patients treated with anterior techniques were younger and had less severe impairment and more focal pathology [20]. More recently, Kato et al. [24] reviewed multicenter prospective data and demonstrated magnetic resonance imaging-based propensity score-matched analysis to compare postoperative outcomes between anterior and posterior surgical approaches for DCM. They included 435 cases and 80 pairs of 1-to-1 matched anterior and posterior surgical cases. In addition, 99% of the matched patients had multilevel compression. They found no significant difference between the two groups in postoperative functional scores or overall perioperative complication rates (16% versus 11%, p=0.48). However, dysphagia/dysphonia was reported only in the anterior group, whereas SSI and C5 radiculopathy were reported only in the posterior group.
Many studies have attempted to compare two different posterior techniques. Fehlings et al. [25] compared surgical outcomes after LP versus posterior laminectomy and fusion for patients with DCM using prospective multicenter data. They analyzed 100 patients with LP and 166 patients with posterior laminectomy and fusion. They reported that both LP and posterior fusion surgeries were effective in improving the functional status and quality of life of patients with DCM, and no significant difference was found between the two groups. In addition, the rates of treatment-related complications were comparable (LP 28.31% versus posterior fusion 21.00%, p=0.1079). Varthi et al. [26] conducted a retrospective review of 779 patients (342 LP and 437 posterior fusions) who underwent LP or posterior decompression and fusion using the American College of Surgeons (ACS)-NSQIP database from 2010 to 2012 [26]. The posterior decompression and fusion group was found to have increased comorbidities at baseline compared with the LP group based on ASA scores and Charlson comorbidity index. They performed propensity-adjusted multivariate analysis to control for differences in baseline patient characteristics and noticed that the posterior decompression and fusion group had increased LOS (+1.2 days, p<0.001), greater rates of any adverse event (odds ratio [OR], 1.7; p=0.018), and a higher readmission rate (OR, 2.3; p=0.028) than the LP group.
Wadhwa et al. [27] compared ACDF and LP for multilevel DCM using the MarketScan Commercial Claims and Encounters database from 2007 to 2016. A total of 1,521 LP cases were included, and a matched cohort of ACDFs was identified. The overall 90-day postoperative complication rate (OR, 1.48; p<0.0001), 90-day readmission rate (OR, 1.41; p<0.01), and the mean length of LP stay (LP 2.96 days versus ACDF 2.17 days, p<0.0001) were greater in the LP group. Hospital costs and total costs of index hospitalization were greater in the ACDF group. No difference was found in the reoperation rates between ACDF and LP.
Similar to our study, Lee et al. [21] used the 2016–2017 ACS-NSQIP database to compare the short-term outcomes for multilevel (≥3) ACDF (with and without corpectomy), LP, and laminectomy/fusion. In the study, 182 patients were included in each cohort after propensity score matching. The study showed that the overall complication and mortality rate was the highest for laminectomy/fusion (any adverse event, 11.5%; mortality, 2.2%) versus ACDF (any adverse event, 3.9%; mortality, 0%; p=0.006) and versus LP (any adverse event, 7.7%; mortality, 0.55%; p=0.286). Furthermore, the laminectomy/fusion group had the highest risk for requiring unplanned readmission (9.9%) versus the LP group (4.4%, p=0.042) and versus the ACDF group (4.4%, p=0.042). The most common reason for unplanned readmission after laminectomy/fusion was wound complications (33.3%). ACDF required the shortest hospital stay (LOS ≥2: ACDF 56.6%) compared with laminectomy/fusion (93.4%, p<0.001) and LP (89.6%, p<0.001).
Regarding postoperative complications, the most statistically significant differences were observed between ACDF and laminectomy/fusion. These included overall complications (ACDF, 3.9%; laminectomy/fusion, 11.5%; p=0.006), mortality (ACDF, 0%; laminectomy/fusion, 2.2%; p=0.044), wound complications (ACDF, 0%; laminectomy/fusion, 2.2%; p=0.044), perioperative transfusion (ACDF, 0.55%; laminectomy/fusion, 3.9%; p=0.032), and unplanned readmission (ACDF, 4.4%; laminectomy/fusion, 9.9%; p=0.042). The complication rates for LP were not significantly different from those for ACDF and laminectomy/fusion, except for pulmonary complications (LP, 0%; ACDF, 2.2%; p=0.044), unplanned readmission (LP, 4.4%; laminectomy/fusion, 9.9%), and LOS >2 days (LP, 89.6%; ACDF, 56.6%; p=0.005).
To the best of our knowledge, this is the first study to assess the short-term outcomes of cervical spine procedures in geriatric patients aged 65 years with DCM. In comparison with the previous literature that included all adults, the present study demonstrated that geriatric patients with DCM were less likely to develop postoperative morbidity and mortality in the short term following ACDF, LP, and PCF, in ascending order. Similarly, geriatric patients with DCM experienced the shorter average operative time and length of hospital stay after ACDF, followed by LP, and the longest for PCF, except for LP, which showed the shortest operative time for patients with dependent functional status prior to surgery. The reoperation and readmission rates were not different between ACDF and LP; however, they were significantly higher for PCF than for the other two.
Postoperative wound infection is one of the most common complications after posterior cervical surgery, whereas it is less of a concern after anterior cervical surgery [21,28]. Interestingly, our study showed that the occurrences of superficial and deep SSI were significantly increased in the PCF group; however, they did not differ between ACDF and LP. This may be because LP requires less lateral soft tissue dissection and less implant burden than PCF.
ACDF demonstrated the least overall short-term postoperative complications. However, oftentimes, the extent and severity of DCM play an important role in deciding the anterior versus posterior approach. Perhaps older patients are prone to have diseases at more spinal levels, which may be more effectively addressed via the posterior approach. This could explain why the ACDF group was the youngest and most functionally independent group, whereas the PCF group carried the overall highest burden of preoperative comorbidities.
Between the two posterior approaches, the present study supported LP over PCF in contrast to previous studies. No significant difference was found in the mean age and functional status before surgery between the LP and PCF groups. These findings suggest that LP is a better option for geriatric patients with DCM undergoing posterior surgery. LP is likely to result in a shorter operation time/hospital stay, fewer occurrences of overall morbidity and mortality, and a lower chance of readmission/reoperation/SSIs within 30 days after surgery than PCF. There is also a financial advantage to performing LP, as Goh et al. [29] demonstrated that the total operative supply cost for PCF is an average of 2.3 times the cost for LP when adjusted for the number of operative levels.
Postoperative adverse events in geriatric patients are affected by not only the type of surgery but also by many other factors. Implementing a perioperative optimization program involving multidisciplinary teams, such as geriatricians, anesthesiologists, physical therapists, and nursing staff, has been shown to reduce the incidence of postoperative complications and shorten the length of hospitalization after spine surgery [30,31]. In addition, preoperative risk stratification should be performed on this patient population. Among the many suggested scoring systems, the modified frailty index is predictive of adverse postoperative outcomes after cervical spine surgery, and it can be utilized to stratify risks and counsel patients undergoing surgery for DCM [32].
This study has several limitations. First, the NSQIP database is limited to the 30-day postoperative period and limited to readmission to participating hospitals. Therefore, our study did not capture complications that occurred beyond this follow-up period or at nonparticipating centers. Second, a significant difference was found in preoperative conditions between the treatment groups. Third, the NSQIP data were not specifically intended for spine surgery, and certain surgery-specific variables of interest are unavailable. For example, we were unable to evaluate complications specific to cervical spine surgery, such as pseudoarthrosis, adjacent segment disease, C5 nerve palsy, dural tear, dysphagia, and hoarseness. Fourth, the number of levels of pathology was not fully controlled between the different treatment groups. For the ACDF group, only patients with both CPT 22551 and 22552 were included to eliminate single-level fusions. However, no data were available for LP and PCF procedures regarding the exact number of levels affected, which could lead to selection bias as the posterior procedures might have involved a higher number of levels. In addition, surgical approaches are often determined by patients’ disease-specific factors, such as the cause of stenosis, alignment, and location. Therefore, our study may have limited clinical applications to a subset of equivocal cases. Finally, this study is a retrospective analysis of a national dataset, which makes it vulnerable to selection/information bias and coding errors.
Conclusions
For patients aged 65 years, PCF carries the highest risk for early postoperative morbidity, mortality, unplanned readmission, unplanned reoperation, and SSI as well as the longest operation time and length of hospital stay. In contrast, ACDF carries the lowest risk for the geriatric patient population. However, there are specific aspects of the disease, such as the number/location of affected levels, presence of ossification of the posterior longitudinal ligament, and body habitus, for which a posterior approach may be advantageous over an anterior approach. For those cases, LP should be included in the preoperative discussion when determining the ideal surgical approach because our study showed that LP has a lower risk for early postoperative morbidity, mortality, unplanned readmission, unplanned reoperation, and SSI than PCF.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conceptualization: JHC, SZH, NNB, YL; data curation: PSB, JL; formal analysis: JHC, PSB, JL; funding acquisition: not applicable; methodology: JHC, PSB, JL; project administration: JHC, SZH, NNB, YL; visualization: writing–original draft: JHC; writing–review & editing: SZH, NNB, YL; and final approval of the manuscript: all authors.