Factors Related to Proximal Junctional Kyphosis and Device Failure in Patients with Early-Onset Scoliosis Treated with a Traditional Dual Growing Rod: A Single Institution Study
Article information
Abstract
Study Design
Observational study.
Purpose
Investigation of factors related to proximal junctional kyphosis (PJK) and device failure in patients with early-onset scoliosis.
Overview of Literature
The use of growth-friendly devices, such as traditional dual growing rod (TDGR) for the treatment of early-onset scoliosis (EOS), may be associated with important complications, including PJK and device failure.
Methods
Thirty-five patients with EOS and treated with TDGR from 2014 to 2021 with a minimum follow-up of 2 years were retrospectively evaluated. Potential risk factors, including demographic factors, disease etiology, radiological measurements, and surgical characteristics, were assessed.
Results
PJK was observed in 19 patients (54.3%), and seven patients (20%) had device failure. PJK was significantly associated with global final kyphosis change (p=0.012). No significant correlation was found between the rod angle contour, type of implant, connector design, and the risk of PJK or device failure.
Conclusions
Treatment of EOS with TDGR is associated with high rates of complications, particularly PJK and device failure. The device type may not correlate with the risk of PJK and device failure. The progression of thoracic kyphosis during multiple distractions is an important risk factor for PJK.
Introduction
Early-onset scoliosis (EOS) is defined as scoliosis occurring before the age of 10 years, irrespective of the etiology [1]. It is one of the most challenging spinal deformities to treat because of rapid progress despite conservative management, substantial remaining spinal growth potential, and incomplete lung development [1,2]. Early correction and fusion strategies have historically been used for treating EOS. However, they were abandoned because of stunted growth and shortening of the spine and small fixed thoracic cage, causing arrested pulmonary development [3,4]. In 1963, the development of a fusionless procedure using growing rods by Harrington [5] led to a paradigm shift in EOS treatment. Despite initial encouraging results, the traditional growing rod procedure requires multiple surgeries under general anesthesia to gradually lengthen the rod throughout childhood, predisposing it to various complications, including rod fracture, anchor failure, and delayed postoperative recovery [4,6]. The high rate of traditional growing rod complications has led to several modifications over the years, resulting in the development of the traditional dual growing rod (TDGR) construct [7]. TDGR remains superior to a single traditional growing rod because it provides better curve control, a greater T1–S1 length increase, and a lower complication rate [8]. The complication rate of TDGR ranges from 29% to 72% depending on the etiology of EOS, fixation method, surgical strategy, and type of growing rod [6,9]. Owing to the distraction mechanism of TDGR, the risk of proximal junctional kyphosis (PJK) may increase following each lengthening. In this study, we aimed to report the rate of PJK and device failure in a series of patients with EOS treated with TDGR and investigate the factors predisposing to these complications.
Materials an Methods
The medical profiles of patients with EOS who were managed with a TDGR procedure in our tertiary referral hospital between 2014 and 2021 were retrospectively reviewed. This study was approved by the ethics committee of our institute (Ethics code: IR.IUMS.REC.1402.305). The requirement for informed consent from individual patients was omitted because of the retrospective design of this study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the Declaration of Helsinki (1964) and its later amendments or comparable ethical standards. The inclusion criteria were the diagnosis of EOS treated with TDGR and a minimum follow-up of 2 years. Patients with a prior history of spinal surgery and those treated with other growing rod systems were excluded from the study.
1. Surgical technique
All surgeries were performed on patients with progressive curves >45° of the coronal Cobb angle and under general anesthesia using the posterior approach. Four anchor points in two lumbar vertebrae and four or six anchor points in the upper thoracic spine were instrumented with separate incisions using screws, hooks, or their combination. The proximal construction included three anchor points from T2 to T5 and two lumbar anchor points selected according to the type of the scoliosis curve from L1 to L4. Rods were passed in a subfascial way. The upper and lower parts of the divided rods were connected to each other with rod connectors. Two types of rod connectors were applied: “end-to-end” and “side-to-side (Fig. 1). Instrumentation, initial correction, and distraction were performed under neuromonitoring assessment. The location of the connector was described as “lower thoracic,” “thoracolumbar junction,” and “lumbar,” which was related to the location of the middle point of the connector was placed on plain X-ray. The types of implants applied were classified as “hook,” “screw,” “lower screw/upper hook,” and “lower screw/upper hook and screw.”

(A–D) Different surgical techniques using traditional dual growing rod, hooks, screws, and different connector types.
PJK and device failure were checked and recorded according to the radiological findings and medical records of the patients. PJK was defined as a proximal junctional sagittal Cobb angle (Cobb angle between the lower endplate of the intravenous urogram [upper instrumented vertebrae (UIV)] and the upper endplate of two vertebrae above the UIV) >10° and at least 10° larger than the preoperative measurement [10]. Radiological measures, including the kyphosis angle, Cobb angle, and coronal balance, were assessed on the available serial radiographs preoperatively, immediately after the index surgery, and at the last lengthening follow-up. To evaluate the effect of the rod on PJK and device failure, the curvature of the proximal rod was assessed using two different methods: “rod ratio” (RR) and “rod Cobb angle” (RCA) (Fig. 2).

(A–D) Rod Cobb angle (RCA) is defined as the Cobb angle between tangent lines respect to the two ends of the rod (A, B). Rod ratio (RR) is defined as the ratio between the lengths of a line that connecting two ends of the rod and the lengths of a perpendicular line from the latter line to the point of maximum curvature of the rod (A, C). In case of differently shaped rods, a mean of RCA and RR was considered as the index of rod curvature.
2. Statistical analysis
Statistical analyses were conducted using SPSS for Windows ver. 16.0 (SPSS Inc., Chicago, IL, USA). Descriptive data were demonstrated by mean±standard deviation for numerical variables or numbers with percentages for categorical variables. The Kolmogorov-Smirnov test was used to test the normality of the distribution of the numerical variables. A comparison of mean values between the two study groups was performed using an independent t-test or its nonparametric counterpart (Mann-Whitney U test). A comparison of mean values between more than two groups was performed using a one-way analysis of variance test or its nonparametric counterparts (Kruskal-Wallis H test). Categorical variables were compared using the chi-square test or Fisher’s exact test. A p-value <0.05 was considered statistically significant.
Results
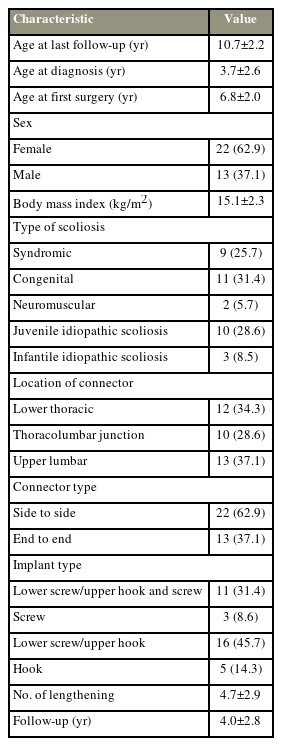
Thirty-five patients who met the study criteria were included in the final analysis. The study population included 22 male and 13 female patients, with a mean age at the last follow-up of 10.7±2.2 years (range, 6–17 years). Data related to demographics, disease etiology, and surgical characteristics of the patients are summarized in Table 1.
The mean preoperative Cobb angle was 59.4°±18.8° and improved to 31.9°±14.7° following the first surgery. The mean Cobb angle of the main curve at the last follow-up was 20.9°±11°. The mean preoperative kyphosis was 30.9°±14.2°, and the mean kyphosis following the first surgery increased to 34.2°±11.7°. At the last follow-up, the mean of the final kyphosis angle was 43.8°±14.6°. In total, nine patients (25.7%) required revision surgery, including seven for device failure and two for PJK.
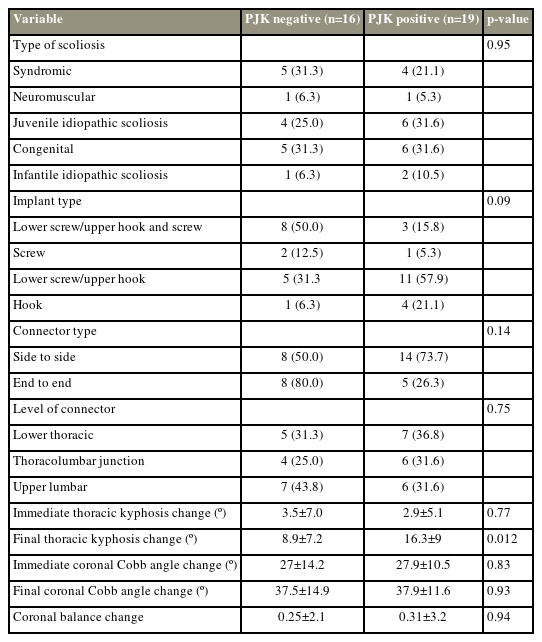
PJK was observed among 19 patients (54.3%), of which two required revision surgery. PJK was significantly associated with global final kyphosis change (p=0.012), and the final kyphosis was significantly larger in the PJK group. However, no statistical correlation was found between other radiological measurements and PJK. While no statistically significant relationship was found between implant type and PJK, PJK was observed less in patients with at least one screw in the upper thoracic spine anchor points (11.4%) than in those with only hooks in the upper thoracic spine anchor points (42.8%) (p=0.09). Side-to-side connectors were more available, and a higher rate of PJK (40%) occurred in this group than in the group using end-to-end connectors (14.3%); however, the latter was not statistically significant (p=0.14). No significant association was observed between PJK and other outcome measures such as the type of scoliosis and connector level (Table 2).
Seven patients (20%) had device failure caused by upper construct dislodgement and rod breakage and required revision surgery. Patients with at least one screw in the upper thoracic spine anchor points had a lower rate of device failure (4.7%) than patients who had only hooks in the upper thoracic spine anchor points (14.2%) (p=0.79). No significant association was observed between the incidence of device failure and the surgical characteristics and radiological measurements of the patients (Table 3).
In the Pearson correlation test, a linear correlation was found between the rod curvature and kyphosis; however, no significant correlation was found between the amount of rod curvature indices and PJK and device failure (Table 4).
Discussion
The use of fusionless techniques for the treatment of EOS aims to correct the spine deformity and allow spinal growth with minimum complications. Despite the introduction of magnetically growing systems for the treatment of EOS to reduce the number of surgeries, other systems, including the TDGR, are still reliable and functional in treating EOS [11,12]. Sometimes, TDGR is the only available system in developing countries to treat EOS. However, the use of this instrument may be associated with two important complications (PJK and device failure) because of the nature of distraction during the lengthening procedure and poor quality of the bone in young children. In this study, the complications of TDGR for treating EOS and the predisposing factors were evaluated. The complications of TDGR for treating EOS and factors predisposing patients to these complications were also evaluated. Altogether, 27 complications (77.1%) were recorded within the mean follow-up of 4 years, including 19 PJK, seven device failures, and one superficial infection. Nine complications (25.7%) required revision.
Bess et al. [4] evaluated the complications of TDGR (single and dual) in 140 patients with EOS. At an average follow-up of 6 years, 177 complications were recorded, including 94 complications in 71 patients who underwent a single TDGR and 83 complications in 69 patients who underwent a dual TDGR. The mean number of complications per patient was 1.2. Nineteen complications (27%) in the single TDGR group and seven complications in the dual TDGR group required revision. Hook dislodgement and rod fracture were the most common complications in both groups. Junctional kyphosis was recorded in one patient in the single TGR group and in two patients in the dual TDGR group. They concluded that regardless of treatment modality, the management of EOS is prolonged; therefore, a high rate of complications should be expected [4]. In the present study, the mean number of complications per patient was 0.8. PJK was the most frequent complication in our series, whereas it was not frequent in the study by Bess et al. [4].
Zarei et al. [13] reported the complications of dual TDGR with all-pedicle screw instrumentation in 42 patients with EOS. At a mean follow-up of 34 months, seven complications (17%) were recorded, including four cases (10%) of superficial surgical site infections and three cases (7%) of PJK. None of the patients required revision surgery. Preoperative thoracic kyphosis is a significant risk factor for PJK development [13]. In the present study, various instruments, including pedicle screws, hooks, and hybrid devices, were used. The complication rate was significantly higher in our study (77.1%). Most patients had PJK as a complication (16 of 27). Similar to the study by Zarei et al. [13], we observed an association between the incidence of PJK and thoracic kyphosis.
Cengiz et al. [14] reported the midterm results of dual TDGR for treating 27 patients with EOS. At an average follow-up of 46.3 months, 18 complications (9.6%) were recorded in 187 procedures, including eight superficial wound infections and ten implant-related complications; however, they did not report any PJK [14]. Although the complication rates of dual TDGR in this study were not considerably different from those reported by Cengiz et al. [14], the nature of the complications was remarkably different. While 16 of 27 complications in this study were PJK, no PJK was recorded in the study by Cengiz et al. [14]. This inconsistency needs to be adequately addressed in future studies.
PJK is a common alignment-related complication in patients with EOS undergoing TGR [15,16], and an incidence rate of 12%–56% has been reported in previous studies [17–19]. The difference rate of PJK in various studies has been attributed to differences in the study sample, EOS etiology, surgical procedure, fixation instrumentation, and follow-up period [17,20,21]. Several risk factors have also been reported for PJK, including the location of the upper or lower instrumented vertebra, proximal thoracic scoliosis of >40°, a main thoracic kyphosis of >60°, a higher correction rate, and location of the UIV in relation to the sagittal apex [17,18,20,22–24]. Recently, the mismatch between the proximal rod contour angle and the proximal junction angle has also been reported as a possible risk factor for PJK among patients with degenerative scoliosis [25]. However, no study has focused on the effect of the proximal rod contour angle and the risk of PJK in patients with EOS. The contour of the rod and the location of the connector had no significant effect on PJK or device failure among patients who underwent spine deformity correction using TDGR.
A younger age at the time of the index surgery and longer procedure times have also been shown to be associated with the incidence of PJK [20]. In this study, the rate of PJK was 54.2% (19 of 35 patients). PJK incidence was significantly associated with a higher global final kyphosis change at the last follow-up. The mean kyphosis change was 16.3º in patients with PJK and 8.9º in those without PJK. Type of implants in the proximal construct (hook or screw), design of the connectors (side-to-side or end-to-end), and rod curvature were not significantly associated with increased risk of PJK.
This study, in line with the results of earlier studies [10–15], shows that TDGR is associated with a high complication rate. Implant failure and PJK could be regarded as the most common complications in patients with EOS managed with TDGR. However, this study was not without limitations. The main limitations of the study were its retrospective design and some patients, who did not allow multivariate analysis of the associations.
Conclusions
Treatment of EOS with TDGR is associated with a high rate of complications, particularly PJK and device failure. The PJK rate can be affected by several risk factors, such as higher kyphosis after index surgery and during lengthening procedures. Moreover, the type of implants in the proximal construct, design of connectors, and curvature of rods were not significantly associated with an increased risk of PJK, and this complication can be attributed to the distraction essence of this type of treatment leading to the progression of thoracic kyphosis. The patient’s parents should be informed of the potential complications to approximate their expectations to reality.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conception or design of the work: MC, JM; acquisition of data: MC, JM; analysis or interpretation of data: MC, JM, BJ; creation of new software used in the work: MC, JM; drafted the work or revised it critically for important intellectual content: FN, MS; approved the version to be published: EAM; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: HG.