C1-C3 Lateral Mass Screw-Rod Fixation and Fusion for C2 Pathologies and Hangman's Fractures
Article information
Abstract
Study Design
Retrospective clinical study.
Purpose
We report our experience of eight patients treated with C1-C3 lateral mass rod-screw stabilization and fusion in the treatment of Hangman's fracture and other axis pathologies.
Overview of Literature
Different surgical approaches, both anterior and posterior, have been described for treating Hangman's fracture and other pathologies where surgery is indicated.
Methods
All patients who underwent surgical treatment for Hangman's fracture and axial pathology where C1-C3 lateral mass screw-rod stabilization and fusion done, following reduction of the fracture or removal of the pathology were included in this series. The recorded patient management data was retrospectively studied.
Results
There were 8 cases in total. All were male, with an average age of 40.75 years. Hangman's fracture occurred in 6 cases (75%), one with metastatic squamous cell carcinoma and the remaining with plasmocytoma. Among the Hangman's fractures 4 (66.66%) had no neuro-deficit. Reduction and bilateral C1-C3 lateral mass screw and rod fixation with posterior fusion by bone graft was performed in all cases. In 2 cases, a C2 body tumor was removed transorally. All patients with neuro-deficit fully recovered, except one who expired in the early post-operative period. Rest of all patients were leading a normal life till last follow up.
Conclusions
Although the number of cases was very small with a relatively short follow up period, C1 and C3 lateral mass screw-rod fixation followed by fusion showed promise as an effective and biomechanically sound way for the treatment of properly selected Hangman's fracture cases, and may also be suitable in other axial pathologies.
Introduction
Hangman's fractures or traumatic spondylolisthesis of the axis commonly affect young people following trauma [1,2]. Nontraumatic pathologies include lymphoma, myeloma, tuberculosis, metastasis and other rare bone tumors [3,4]. In Hangman's fracture, surgical reduction and stabilization is usually indicated in cases with neuro-deficit with spinal cord compression, cases with instability, or after failure of conservative treatment. In other pathologies, stabilization and fusion is usually needed along with removal of the C2 pathology. Different surgical approaches, both anterior and posterior, have been described for treating Hangman's fractures and other pathologies [1,2,3]. We report our experience of eight patients treated with C1-C3 lateral mass rod-screw stabilization and fusion in the treatment of Hangman's fracture and other axis pathologies.
Materials and Methods
All patients who underwent surgical treatment for Hangman's fracture and axial pathology where C1-C3 lateral mass screw-rod stabilization and fusion were done following reduction of the fracture or removal of the pathology from January 2009 to December 2012 in the department of Neurosurgery, Dhaka Medical College Hospital and a few other private hospitals in Dhaka, Bangladesh were included in this series. Patient management data was recorded prospectively with special attention on stabilization by C1-C3 lateral mass screw-rod. Patient history, clinical features, imaging findings, surgical approaches, preoperative findings, postoperative clinical and imaging follow up (including any complications) were properly recorded. All recorded data were reviewed retrospectively.
1. Operation
Operations were performed with the patient kept under skeletal tong traction in the prone position. The head end of operating table was elevated to create a table angle of 35° with the floor. Cervical spine of the patient was kept in a neutral position (not in flexion or extension). Proper alignment was achieved under fluoroscopic control, and the region from C1 to C3 was exposed through posterior midline incision. The C2 root and ganglion were identified and sectioned on both sides, and the C1 lateral mass was exposed with proper hemostasis of venous bleeding. The C3 lateral masses were exposed on either side. 3.5 mm×28 mm polyaxial titanium screws were inserted into the C1 lateral masses on either side followed by insertion of 3.5 mm×14 mm polyaxial screws into the lateral masses of C3. For insertion of the C1 lateral mass screw, the entry point was the middle of the lateral mass with a 10° medial angulation aiming for the anterior tubercle of Atlas. For the C3 lateral mass screw, the entry point was 1mm medial to the center of the lateral mass, with 20° lateral and 15° rostral angulation. The exposed posterior surfaces of C1, C2, and C3 were decorticated, and autologous or heterogenous grafts obtained from the posterior iliac crest or heterogenous bone grafts was applied as an onlay graft, then the wound was closed in layers. Then transoral microsurgical removal of mass lesions causing spinal cord compression was performed in the same sitting, where needed.
2. Representative cases
1) Case 2
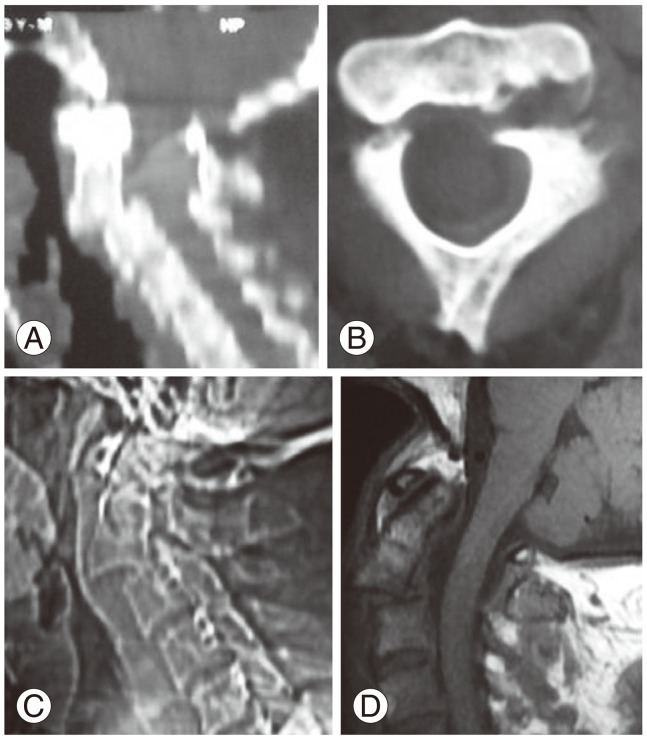
A 60-year-old male presented with a history of neck pain, and progressive weakness in all limbs for 5 months. He was a chronic alcoholic, diabetic and hypertensive. Upon examination, he was ill looking, morbidly obese (128 kg at a height of 175 cm), moderately anemic, and had a respiratory rate of 25 breath/min. Neurologically, he was conscious and oriented. His neck was short, neck muscle was taught, and neck movements were restricted and very painful. There was tenderness at the cranio-vertebral junction. His muscle power in all limbs was Medical Research Council grade 0/5 with a sensory level C2, bilaterally. There were signs of upper motor neuron lesions in all limbs. His autonomic functions seemed to be normal, and radiographs showed destruction of the C2 body and dens with atlanto-axial dislocation (Fig. 1A, B). A computed tomography (CT) scan of the cranio-vertebral junction showed the C2 destruction with dislocation (Fig. 1C, D), while C1 and C3 seemed to be intact. A magnetic resonance imaging (MRI) showed spinal cord compression at the level of C2 (Fig. 1E). Other investigations (complete blood count, chest X-ray, electro cardio gram, abdominal ultrasound, blood film, renal and liver function test) showed no abnormality. After the correction of anemia with proper counseling, we decided to operate using both a posterior and anterior approach in the same sitting. Under general anesthesia with transnasal fiberoptic endotracheal intubation, the C1-C3 lateral mass screw-rod fixation and fusion was performed first through a posterior approach, with a heterologus bone graft. After positional change, the C2 vertebra was approached transoraly. The C2 body and dens were destructed, and there was a vascular, soft, suckable and curatable tumor tissue at the C2 body level compressing the dura. The C1 arch and C3 body were intact. Bone grafting and anterior fixation were not performed at the time of transoral microsurgery, with the hope that a second surgery could be performed after having histopathology and non-surgical treatment, if needed (i.e., chemo or radiotherapy). The dura was decompressed adequately. Postoperatively, the patient was nursed in the intensive care unit. Histopathology reported plasmocytoma. Oncologists advised the bone marrow examination was normal, and local radiotherapy was given for six weeks postoperation. He began to recover neurologically very rapidly from the fourth postoperative day. Early postoperative imaging showed good alignment with the screws and rod in position (Fig. 2). Three weeks later, the patient could sit with a hard cervical collar. By the end of the third month, he became freely ambulant. Though he was counseled for the necessity of another operation, he disappeared from follow up for the next two years, as he was staying abroad. Two years later he returned home, and received follow up. He was doing well. X-rays showed reduced space of the C2 vertebral area with disalignment of the left C1-C3 screw and rod, but there were signs of posterior fusion. He was found to be doing well up to the last follow up (three years postoperation).

(A, B) X-ray of cervical spine later view in extension and flexion, respectively, showing destruction of the C2 body with translation in flexion and extension of the neck. (C, D) Computed tomography scan of cranio vertebral junction sagital sections showing C2 body destruction (by plasmocytoma). (E) Magnetic resonance imaging of the cervical spine TW2 sagital section showing the C2 body lesion with spinal cord compression.

(A, B) X-ray of cervical spine anterio-posterior and lateral view of Case 2, Fig. 1, after C1-C3 lateral mass screw and rod fixation. (C, D) Postoperative computed tomography scan of the cervical spine showing the sagital section (C) and axial section (D) at the level of C3, (E)-axial section at the level of C1, showing screws and rods in situ after operation.
2) Case 4
A 79-year-old male was involved in an accident while riding a microbus. He briefly lost consciousness, and complained of neck pain after regaining consciousness. He was transferred to a nearby hospital, where radiographs revealed a Hangman's fracture, and the patient was subsequently transferred to our department for surgical management. He had no neurological deficits, but had tenderness over the cervical spine. His cranial CT examination was normal, and CT scan and radiographs of the cervical spine revealed a type III Hangman's fracture (Fig. 3A-C). MRI of the spine revealed no spinal cord compression or hematoma (Fig. 3D). In view of the unstable nature of the fracture and the presence of angulation, it was believed that immobilization with external orthosis would not be effective and hence, surgical fixation was opted for. Pre-operative traction was not attempted. CT examination of the spine showed that the fractured fragments were displaced, hence direct fixation of the pars fracture with pars screws was not considered safe or feasible. This led to the decision to use C1-C3 lateral mass screw-rod fixation and fusion. With the patient kept under skeletal traction in the prone position, proper alignment was achieved under peroperative X-ray control, and C1-C3 lateral mass screw-rod fixation and fusion was performed (Fig. 4A, B). The exposed posterior surfaces of C1, C2, and C3 were decorticated, autologous grafts obtained from the posterior iliac crest were applied as an onlay graft, and the wound was closed in layers. Postoperative radiographs showed good alignment with proper placement of the screws. Postoperatively, the patient developed occipital numbness due to cutting of the C2 ganglion, which was improved by six months postoperation.
Preoperative images. (A, B) Computed tomography scan of cervical spine sagital and axial sections, respectively. (C) X-ray of cervical spine lateral view and (D) magnetic resonance imaging of cervical spine sagital section (T1W) showing Hangman's fracture type III.
Results
There were 8 cases in total. Details of the cases are given in Table 1 and in Figures (Figs. 1,2,3,4,5,6,7). All were male, with an average age of 40.75 years (range, 16-79 years).
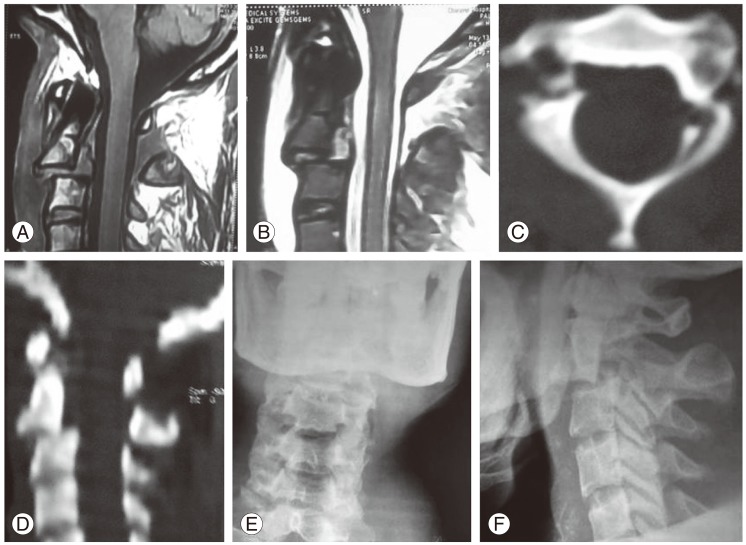
(A, B) Magnetic resonance imaging of cervical spine sagital section in T1-weighted and T2-weighted images, respectively. (C, D) Computed tomography scan of cervical spine axial and sagital sections, respectively. (E, F) X-ray of cervical spine anterio-posteror and lateral view showing Hangman's fracture.
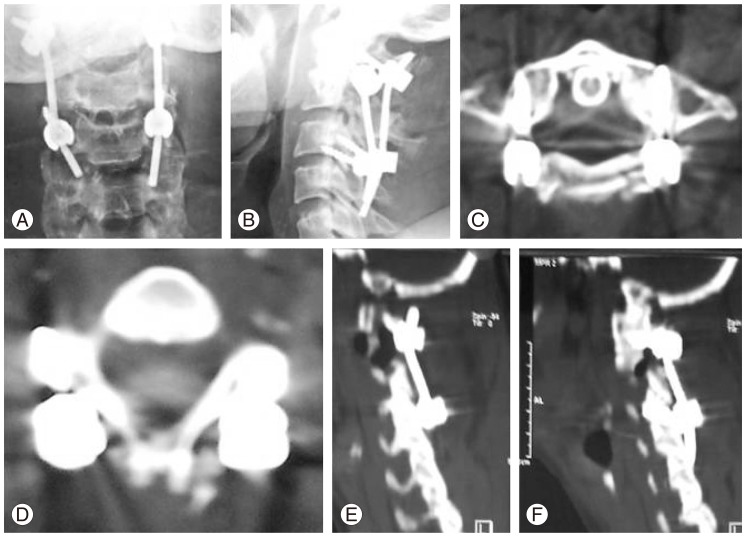
(A, B) Postoperative X-ray of cervical spine anterio-posterior and lateral view, respectively, after fixation of the C1-C3 lateral mass. Computed tomography scan of the cervical spine (postoperative). (C, D) Axial section at the level of C1 and C3, respectively. (E, F) Sagital sections showing screws and rod in proper places.
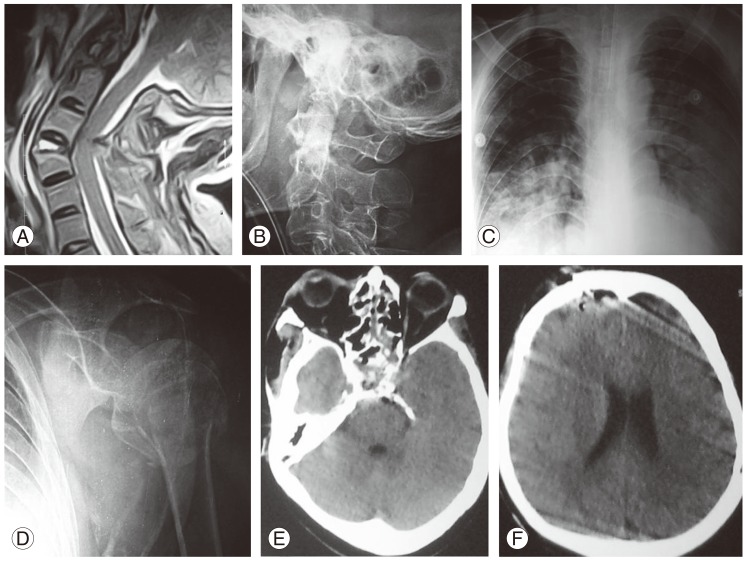
(A) Magnetic resonance imaging of the cervical spine T2-weighted image showing fused cervical vertebral bodies (ankylosing spondylitis) with fracture of C2 and C3 with angulation and spinal cord injury. (B) X-ray of cervical spine lateral view after ventilatory support with endotracheal intubation and cervical traction. (C) Chest X-ray posterio-anterior view, showing crowding of the ribs on the right side with bilateral lung contusion. (D) Shoulder X-ray showing fractured humeral neck with dislocation of the shoulder. (E, F) Computed tomography scan of the brain, showing anterior skull base fracture with frontal fracture and extradural hematoma with pneumocephalus.
C2 Pathologies were: six cases of traumatic Hangman's fracture (75%); one metastatic squamous cell carcinoma (12.5%); one plasmocytoma (12.5%). Clinical features included the following: History of road traffic accident in six cases of Hangman's fracture (75%); neck pain and restricted neck movements in seven cases (88.5%); quadriparesis in two cases (25%); quadriplegia in two cases (25%); autonomic dysfunction in one case (12.5%); respiratory difficulty in two cases (25%), one of mild difficultyand one requiring ventilatory support. Among the Hangman's fracture cases, 4 (out of 6) had no neuro deficit.
Investigations performed on the patients are as follows: plain X-ray with an anterior-posterior and neutral lateral view were done in all cases (100%), while flexion and extension lateral view and open mouth views were performed in 3 cases (37.5%); MRI and CT scans of the cranio-vertebral junction were done in all cases (100%). Operative procedures were performed in the cases as follows: reduction and bilateral C1-C3 Lateral mass screw and rod fixation with posterior fusion by bone graft was performed in all cases (100%); C2 body tumor was removed transorally in 2 cases (25%). During transoral surgery, the soft palate was not cut. In the 2 cases with tumors, radiotheray and chemotherapy were given postoperatively. In the C2 metastetic squamous cell carcinoma (Table 1; case 1), the primary site was occult.
All patients with neurodeficit recovered fully except one: an old patient with ankylosing spondylitis accompanying a type-3 Hangman's fracture and a spinal cord injury, with aspiration peumonia, expired on the third postoperative day (Table 1; case 6). In the case with C2 plasmocytoma (case 2) (Table 1, Fig. 7), the patient was unavailable for follow-up and re-surgery as advised, after receiving chemo and radiotherapy (Figs. 1, 2). When the patient returned from abroad two years later, he was doing well without any complaints. X-ray showed reduced space of the C2 vertebral area with disalignment of the left C1-C3 screws and rod, but there were signs of posterior fusion. The patient was found to be doing well up to the last follow up. In the rest of the cases, all patients were leading a normal life without any symptoms at the time of the last follow up.
Discussion
Traumatic spondylolisthesis of the axis (TSA) has been classified in many ways. The Modified Effendi's [5] classification is as following: type 1, non-displaced fractures with no angulation between C2 and C3, and a fracture dislocation of less than 3 mm; type 2, fractures with significant angulation (>11°) and displacement (>3.5 mm); type 2A, fractures with minimum displacement and significant angulation (>11°); type 3, fractures with severe angulation and displacement associated with unilateral or bilateral C2-3 facet dislocation. Using the aforementioned classifications, many conservative and surgical approaches to TSA have been recommended [1]. Hangman's fractures constitute 4% of all cervical fractures [6]. Among the different types of axis fractures, Hangman's fractures constitute 20% [7]. Among the different types of Hangman's fractures, type I constitutes 65%, type II 28%, and type III 7% [1]. Most Hangman's fractures can be treated by rigid external immobilization [8]. Rigid external immobilization for Levine-Edwards type I and type II fractures is recommended, but surgical intervention is favored when there is evidence of instability, as in type IIa and type III fractures; however, the reported failure rates of rigid orthosis eventually requiring surgical fusion varies from 9% to 32% [6,9]. Classically, type 1 TSA cases can be treated conservatively, but type 2 and 3 fractures require an anterior or posterior surgical treatment [1]. When choosing a surgical procedure, the goals of surgery are to reduce the fracture, maintain alignment of the spine, confer stability, achieve fusion, preserve mobility, and protect the neural structures. It can be quite difficult to balance these factors, equally when determining the most effective operation to perform [10].
Surgical approaches to TSA include: 1) anterior discectomy and fusion; 2) posterior approaches, which include (a) occipitocervical fusion, (b) C1-C3 fusion, and (c) direct screw fixation of the fractured pars. Each approach has advantages and limitations, and the approach is chosen depending upon the degree of translation, angulation, morphology of the fracture, the patient's anatomy, and the surgeon's experience and skill [11]. An anterior approach, transoral or extraoral C2-3 fusion and fixation, addresses C2-3 disc herniation and C2-3 stabilization [1,12]. On the other hand, a posterior approach can fixate posterior and anterior parts of the C2 vertebra, and the addition of posterior C2-C3 fixation can stabilize this segment. A combined approach covers all the elements of the C2-3 segment. An alternative surgical option includes direct screw fixation of the C2 pars or pedicle. The C2 pars and pedicle connect the posterior elements of the C2 vertebra to the C2 body [1,13].
Anterior discectomy and screw plate fixation is an effective, but not very popular technique, due to difficulty in exposing the C2-C3 region, difficulties associated with anterior screw placement in the axis, and the elimination of C2-C3 rotation [1,11]. This approach also puts vital structures, such as the facial and hypoglossal nerves, contents of the carotid sheath and the superior laryngeal nerve, at risk [14]. Posterior approaches include: 1) occipitocervical fusion, 2) direct fixation of the fracture with pars screw, and 3) C1-C3 lateral mass fusion. Due to elimination of occipitocervical movements, as well as atlantoaxial rotation, occipitocervical fusion should be used only as a last resort, or as a salvage procedure [1].
Direct screw fixation of the C2 pars fixes the fracture without compromising movement [11]. This technique is only feasible in patients where the fracture is posteriorly located and the screw can be placed safely without risking injury to the vertebral artery [11]. Another disadvantage of this method is the need for complete manual reduction of the fracture intraoperatively before the placement of lag screws in the fractured pars [11,14]. Moreover, the screw passes through the narrowest part of the vertebra, which is bounded medially by the spinal cord and laterally by the vertebral artery. The diameter of the screw is 3.5 mm, while the space available for the screw varies between 5 mm and 7 mm [14]. The rate of vertebral artery injury for this method varies between 11% and 66% [15,16]. Direct pars screw fixation is not suitable for type III Hangman's fractures with associated disruption of the C2-C3 disc [17], because direct pars screw fixation is not effective in limiting flexion and extension if there is disc disruption [18]. In our patients of Hangman's fracture, we did not consider direct pars screw fixation as an option.
C1 and C3 lateral mass screw-rod fixation with fusion for Hangman's fractures has the following advantages: 1) risk of vertebral artery injury is minimized; 2) risk of displacement of the fractured fragments into the spinal canal is eliminated; and 3) conventional lateral mass screws can be used, unlike in the direct pars screw fixation technique, which requires the use of appropriate sized lag screws. Biomechanically, fusion of C1 and C3 lateral masses with C2 sparing provides sufficient stability [19]; however, it is not without disadvantages, including elimination of atlantoaxial rotation [20]. Though few cases of C1 and C3 lateral mass screw-rod fixation with fusion for Hangman's fractures have been reported, the efficacy of the posterior C1-C3 fusion technique was confirmed by a recent biomechanical study by Chittiboina et al. [21], who showed that both anterior C2-C3 discectomy and fusion, as well as posterior C1-C3 fusion, were equally effective biomechanically. The technique of C1-C3 fusion is based on the cervicocranial concept of Hangman's fracture initially elucidated by Effendi et al. [9] and later elaborated by Chittiboina et al. [21]. In this concept, Hangman's fracture consists of two parts, the ventro-cranial part consisting of the atlas, the dens and the body of the axis, and the dorso-caudal part consisting of the posterior elements of the axis and C3 [21]. Accordingly, fusion of C1 and C3 lateral masses effectively fixes the ventro-cranial and the dorso-caudal components. Moreover, type II and type III fractures with disruption of the C2-C3 disc space and posterior longitudinal ligament are best treated by posterior stabilization, as these injuries are more likely to fail in flexion [1,10]. This technique is easy to use, and avoids the above mentioned risks of anterior discectomy and plating, as well as the risks associated with direct pars screws [1].
Cranio-spinal junction tumors are rare lesions that have a natural history towards tetraplegia, usually being a serious threat to the life of the patient. The treatment of these upper cervical spine tumors involving C1 and C2 segments has improved considerably in the last few decades. The upper cervical spine tumor pathology C1-C2 imaging investigations that allow the precise definition of the anatomical structures involved in tumor pathology, together with refined surgical techniques including more and more complex fixation instrumentation allows for the complete removal of craniospinal junction tumors with the preservation or the regaining of stability [3,22]. Tumors located in the region of the upper cervical spine and the craniocervical junction may be benign or malignant, and are quite rare. The most frequent type is chordoma, which accounts for 1%-4% of all primary bone tumors [23,24]. These tumors are found in the sacrococcygeal region in 45% of cases, on the skull base in 40%, and the remaining 15% relate to the spine (cervical, in particular). Chordoma develops from the persistent portions of the primitive notochord that is an embryological precursor of the axial skeleton [23,24,25]. Most often, it is soft and gelatinous, but it may also be fibrous and rigid, complicating its surgical removal [26]. Chordoma of the cervical vertebra typically affects the vertebral body and expands into perivertebral soft tissues and the epidural space [27]. It grows slowly, and may become quite sizeable prior to the development of symptoms leading to diagnosis. Most frequently, it is diagnosed in the age group of 50-69 years, with men affected twice more often than women [23,24,25]. Excluding chordoma, other tumors that may affect the C2 vertebra and cranio-vertibral junction are osteoid osteomas, osteo-chondromas, plasmocytomas, histiocytoses, fibrous dysplasia, aneurysmatic bone cysts, osteo-blastomas, Ewing sarcoma, and giant-cell tumors of bone and metastases [4]. Presenting symptoms of such tumors are cervical pain, occipital neuralgia, medullary compression syndrome, and/or cranio-spinal junction instability. The purpose of surgery is to establish a histopathologic diagnosis, and to decompress the neural elements by attempting a total tumor removal, as well as to stabilize the cranio-cervical junction in order to improve the patient's quality of life [3]. Preoperative work-up included an MRI with a minimum of T1, T2, and T1 with contrast, useful both as a diagnostic tool and for surgical planning. In most situations, plain X-rays and CT scans are required for better visualization of bony structures, but the MRI is by far the most valuable investigation tool in this pathology. CT scanning is impractical for the screening of vertebral tumors, but extremely valuable for preoperative planning. Plain X-rays act as a screening investigation, and dynamic flexion-extension X-rays establish the degree of instability preoperatively and for the postoperative control of stability. Patients with suspected metastatic lesions should receive brain, thoracic and abdominal CT-scans, chest X-ray, bone scan, ultrasonogram, blood film, and bone marrow examination evaluation. Angio CT and spinal angiography are sometimes very helpful in the planning of surgery. Tumor biopsy is reserved for cases which lack neurological signs or spinal instability. A reasonable enough indication for biopsy is the suspicion of a certain histopathological type of tumor that is essentially treatable by non-surgical therapy (radio/chemotherapy or percutaneous vertebroplasty with polyacrilic cement, etc.) [3]. The surgical treatment for cranio-spinal junctional tumors challenges the neurosurgeon with many difficulties due to the less frequent tumoral pathology at this level, and the unique biomechanical characteristics of the region.
Surgical success depends on the location, extension, and nature of the tumor, as well as on the neurosurgeon's experience. Difficulties are seen in cases of tumors that involve the bone and ligaments at the C1-C2 level. Decisions over approach and stability methods are essential. The chosen surgical approach should ensure tumor resection, or at least tumor tissue biopsy for histopathological examination. It must also take into account the tumor location and the patient's prognosis. Patient survival is directly related to the extent of the resection and the histopathological type of tumor. If both anterior and posterior approaches are needed, they can be performed in same or different settings. A transoral approach is most commonly used for anterior cervical spinal cord decompression. A submandibular retropharyngian approach may sometimes be useful but it is accompanied by disadvantages in the depth of the operating field, the long dissection time, compression on the nerves IX, XII and on the pharynx, with possible paresis of these nerves and post operatory deglutition impairment (usually transient) [3,28]. A postero-lateral and posterior approach is used more commonly. The advantages of this approach are that it has become familiar to many neurosurgeons as it is frequently used, and allows posterior rahisynthesis with bone grafts or metallic fixation [3,28]. When total tumor resection is planned, total spondylectomy is done through combined anterior and posterior approaches with anterior spinal column reconstruction and posterior stabilization and fusion [4]. Most tumors that involve the cranio-spinal junction, especially the axis, lead to instability. Fusion techniques have been chosen according to the nature and location of the tumor, the degree of bone involvement, and the patient's prognosis. The most widely used procedure in obtaining cranio-spinal junction stability has been the posterior occipito-cervical fusion. Postoperatively, patients have been immobilized with a halo for 4 to 8 weeks. When C1 and C3 are intact and pathology only involves the axis, then C1-C3 lateral mass screw-rod fixation with fusion can be used; however, to date, report on C1-C3 lateral mass screw-rod fixation with fusion in axial pathology is inadequate. In the case of malignant disease of the axis, postoperatively patients may need radiotherapy or chemotherapy, or both.
Conclusions
Although number of cases was very small and the follow up period was relatively short, C1 and C3 lateral mass screw-rod fixation followed by fusion showed promise as an effective and biomechanically sound way of treatment of properly selected Hangman's fracture cases, and may also be useful in other axial pathologies.
Notes
No potential conflict of interest relevant to this article was reported.

