Effect of Osteoporosis on Clinical and Radiological Outcomes Following One-Level Anterior Cervical Discectomy and Fusion
Article information
Abstract
Study Design
Retrospective study.
Purpose
This study aimed to evaluate how osteoporosis affected the clinical and radiological outcomes of patients who underwent anterior cervical discectomy and fusion (ACDF) with plating.
Overview of Literature
The incidence of complications associated with implants is high when ACDF is performed in patients with poor bone quality.
Methods
In total, 101 patients without (T-score ≥1.0, group A) and 25 with (T-score ≤−2.5, group B) osteoporosis who underwent single-level ACDF with plating were followed up for >2 years. The clinical and radiological outcomes were compared between the two groups. The fusion rate and implant-related complications were evaluated.
Results
Although clinical outcomes such as visual analog scale scores for the arm (2.0±2.3 vs. 2.4±2.9, p=0.490) and neck pain (1.4±1.9 vs. 1.8±2.2, p=0.343) and neck disability index (7.7±7.1 vs. 9.9±7.5, p=0.225) were slightly higher in group B, no statistically significant difference was noted. Cage subsidence (13.9% vs. 16.0%, p=0.755) and plate migration (7.9% vs. 8.0%, p=1.000) rates did not differ between the two groups. The fusion rate at 1 year postoperatively was higher in group A than in group B (80.3% vs. 68.2%, p=0.139) and slightly increased in both groups (94.6% vs. 86.4%, p=0.178) at the final follow-up.
Conclusions
Osteoporosis did not significantly affect the rate of cage subsidence or plate migration after cervical fusion. After ACDF, increased cage subsidence and implant migration rates had no significant effect on clinical outcomes.
Introduction
Numerous spine surgeries are thought to be significantly affected by osteoporosis, and as the population ages, surgeries for the cervical spine have become more common [1,2]. A significant rate of implant-related problems is anticipated when anterior cervical discectomy and fusion (ACDF) with or without anterior plating is performed in patients with osteoporosis [1]. Postoperatively, these problems may result in neck pain, functional impairment, or revision surgery [3]. Several authors have reported that segmental kyphosis, acceleration of adjacent segmental disease, and decreased fusion rate may occur after the development of cage subsidence [4–6]. However, some debates exist over whether patients with osteoporosis have poor clinical and radiological outcomes after ACDF surgery.
Various ACDF techniques, such as stand-alone cage insertion, cages with plates, and zero-profile devices, have been developed [7,8]. Although some studies have demonstrated that an anterior cervical plate is a key factor in increasing the fusion rate, preventing subsidence, and restoring cervical alignment, weak evidence shows that different ACDF surgical techniques yield different clinical outcomes in patients with poor bone quality [5,9–11].
Only a few studies have analyzed both clinical and radiological outcomes as a function of bone mineral density (BMD) following anterior cervical fusion surgeries. Therefore, this study aimed to determine the effect of osteoporosis on clinical and radiological outcomes in patients who underwent one-level ACDF with plating surgery and confirm the efficacy and stability of anterior plate augmentation.
Materials and Methods
Records of 156 patients who underwent one-level ACDF for cervical myelopathy, radiculopathy, or myeloradiculopathy between April 2011 and December 2020 were retrospectively reviewed. Among these patients, 126 with a T-score for spinal BMD of ≥−1.0 or ≤−2.5 were included. The spine BMD from L1 to L4 was evaluated using dual-energy X-ray absorptiometry (Lunar Prodigy Advance; GE Healthcare, Chicago, IL, USA). According to their T-score, patients were divided into those without osteoporosis (group A: T-score ≥1.0) and with osteoporosis (group B: T-score ≤2.5) [12]. A single surgeon performed all surgeries, and the patients were followed up for >2 years. Patients who underwent revision surgery and surgery for spine tumors, infections, or trauma were excluded.
Demographic data, including age, sex, height, weight, body mass index, and comorbidities, were collected from electronic chart reviews. Clinical parameters were obtained, including Visual Analog Scale (VAS) scores for neck and arm pain and Neck Disability Index (NDI) scores. All patients were followed up 1, 3, 6, and 12 months postoperatively and annually thereafter.
This study was approved by the institutional review board of Asan Medical Center (A20220807), which waived the requirement for informed consent because of the retrospective nature of the analysis.
1. Radiological assessment
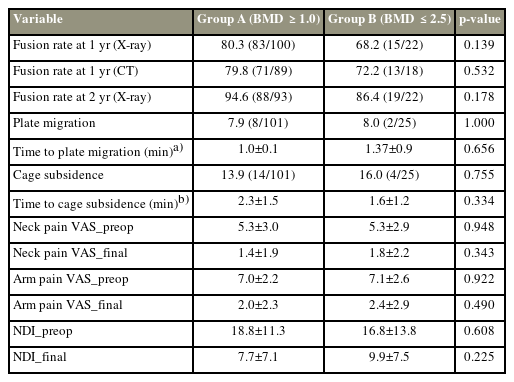
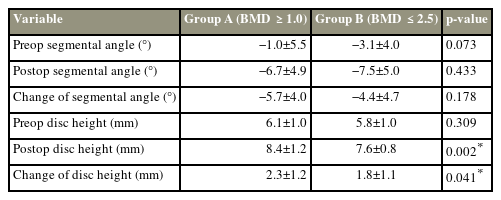
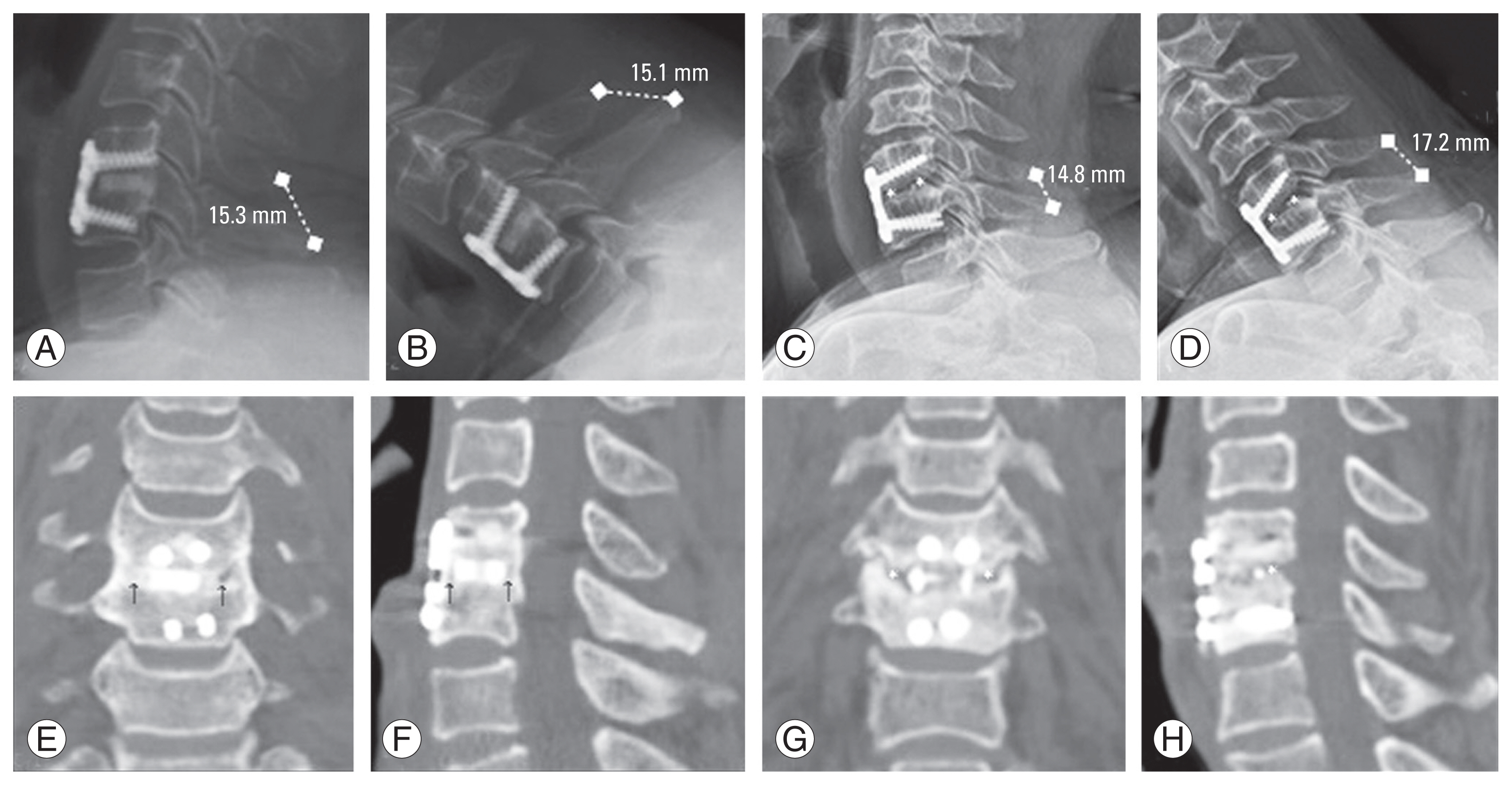
Plain cervical spine anteroposterior and lateral radiographs were obtained within 1 week and 1, 3, 6, 12, and 24 months postoperatively. Furthermore, dynamic (flexion and extension) lateral radiographs were obtained 3, 6, 12, and 24 months postoperatively. Three-dimensional computed tomography (CT) was performed 1 year postoperatively. Fusion status was assessed by the following two methods: (1) absence of mobility in dynamic lateral (flexion and extension) radiographs (<1 mm in the interspinous motion) and (2) existence of extra graft-bridging bone and mature bony trabeculae bridging the interbody space in CT (Fig. 1) [13]. Height loss of >2 mm from the immediate postoperative images was considered cage subsidence. Plate migration was assessed with a displacement of the plate or screws >2 mm in the follow-up radiographs or CT images (Fig. 2) [14]. Because the cervical spine is a small structure, the digital images were enlarged by 200% and assessed. The segmental angle was measured using Cobb’s angle between the upper endplate of the upper vertebral body and the lower endplate of the lower vertebral body. The height of the discs was measured as the distance between the center of the upper and lower endplates. Two spine surgeons independently measured all radiological parameters. Subgroup analysis was also performed for cage subsidence and plate migration.
Radiological assessments. (A, B) Measurement of interspinous movement (ISM) at operated levels on dynamic radiographs. ISM is consistent with our definition of fusion (<1 mm). (C, D) Evaluating bone bridging on multiaxial reconstructed coronal and sagittal computed tomographic (CT) images. It appears to be fused with bone bridging formation at both C5–6 levels. (E, F) ISM >1 mm is observed on dynamic radiographs, indicating pseudarthrosis. (G, H) Coronal and sagittal CT images demonstrate a cleft and no extragraft bridging bone, which indicates pseudoarthrosis.

Lateral radiograph of the cervical spine taken at the immediate postoperative period (left) and at follow-up visit (right). (A, B) Cage subsidence >1 mm, (C, D) screw migration >1 mm in lateral plane radiograph, (E, F) distinct plate tilting in anteroposterior plane radiograph, and (G, H) cage subsidence with screw migration in lateral plane radiograph are shown.
2. Surgical procedure
Smith and Robinson’s method was used to approach the anterior cervical spine. The intervertebral discs and osteophytes were resected using an endplate preparation. The superior and inferior endplates were minimally decorticated; however, the cortical bone remained intact to prevent cage subsidence. In cases of radiculopathy, uncoforaminotomies were performed for neural foraminal decompression and fusion bed formation [15]. A trial cage was used to determine the appropriate cage size. A freeze-dried fibular cortical ring allograft (Bone Bank Allografts, San Antonio, TX, USA) was filled with local bone, and it was harvested during spur removal and endplate preparation. All surgical levels were concomitantly fixed with an anterior cervical plate and variable screw constructs, which allowed graft compression with gradual settling. The cage was located at a depth of 2–3 mm from the anterior margin of the vertebral body. Neck collars were applied to the patients for 6–12 weeks after ACDF.
3. Statistical analyses
The differences in demographic, clinical, and radiological parameters between groups A and B were compared using independent t-tests, the chi-square test, or Fisher’s exact test. p<0.05 was used to determine statistical significance for all statistical analyses, which were performed using IBM SPSS Statistics ver. 21.0 (IBM Corp., Armonk, NY, USA).
Results
No significant differences were found between the groups in terms of age, cervical pathologies, or surgical segments. Of the 126 patients, 101 and 25 comprised groups A and B, respectively. The most common lesion was observed at C5/6. No patient required revision surgery or experienced any neurological complications. Compared with group A, group B had a significantly higher proportion of female patients and included more patients on medication for osteoporosis. Group B included more patients with previous thoracolumbar spine fractures; however, the difference was not statistically significant. Table 1 summarizes the patients’ demographic and preoperative clinical characteristics. In the preoperative and final follow-up periods, clinical assessments such as NDI and VAS scores for the arm and neck pain did not differ between the groups.
The rates of plate migration (7.9% versus 8.0%, p=1.000) and cage subsidence (13.9% versus 16.0%, p=0.755) did not differ between the two groups, and most implant-related complications were observed in the early postoperative period. The fusion rates assessed using simple dynamic radiography were higher in group A than in group B (80.3% versus 68.2%, p=0.139) 1 year postoperatively. Two years postoperatively, the fusion rate increased in both groups, and this difference diminished (94.6% versus 86.4%, p=0.178). However, group A still showed a higher fusion rate than group B. Five patients in group A and four in group B with delayed union eventually showed union 2 years postoperatively although no fusion was observed at the 1-year follow-up. Table 2 presents the comparisons of radiological and clinical outcomes between the groups. As shown in Table 3, the segmental angles were comparable between the groups both preoperatively and postoperatively. However, the postoperative disc height and change in disc height were higher in group A than in group B.
Table 4 summarized the subgroup analyses of cage subsidence and plate migration. Cage subsidence and plate migration did not affect clinical outcomes. Furthermore, an increased prevalence of cage subsidence was associated with older age (p=0.030), and sex distribution affected the incidence of cage subsidence (p=0.042). The proportion of male patients in patients with cage subsidence was higher than that in the nonsubsidence group. Contrary to our expectations, neither cage subsidence nor plate migration was associated with bone quality (p=0.711 and p=0.540, respectively). Meanwhile, the 1-year (50.0% versus 86.1%, p=0.001) and 2-year (66.7% versus 98.1%, p<0.001) fusion rates postoperatively were affected by cage subsidence (66.7% versus 98.1%, p<0.001) but not by plate migration. In contrast, in the plate migration subgroup, the disc height difference before and after surgery was relatively high (2.9±1.6 mm versus 2.1±1.1 mm, p=0.055).
Discussion
Cage subsidence has been frequently reported following ACDF and can affect fusion rates and clinical outcomes. Various factors affect cage subsidence, including overdistraction, endplate preparation, and appropriate cage size. However, information concerning the factors affecting subsidence following ACDF is limited [3,5–7,14,16,17]. Lee et al. [3] analyzed the risk factors for subsidence following ACDF. In their study, subsidence occurred in 26 of 78 patients (33.3%), and the main factors affecting subsidence were old age, nonuse of plates, preoperative cervical kyphotic alignment, and preoperative lower anterior disk height. Moreover, patients who underwent surgery without using plates were 6.0-fold more likely to display subsidence than those who underwent surgery using plates [3]. However, they did not address the effect of poor bone quality on cage subsidence.
Cadaveric experiments revealed that BMD is closely related to mechanical properties such as elastic modulus, strength, stiffness, and yield load [18]. We generally believe that the inherent poor bone quality increases bone–implant failure, decreases screw pullout strength, and may predispose to interbody cage subsidence. Moreover, compared with patients without osteoporosis, those with osteoporosis undergoing spine surgery experience longer and more expensive hospital stays [2].
However, in this study, the incidence of mechanical complications, such as cage subsidence and plate migration, following ACDF was not higher in patients with osteoporosis. This appears paradoxical given that significant experimental associations between BMD and biomechanical behavior have been demonstrated. Because the cervical vertebrae support less weight than the lumbar vertebrae and the size of the vertebral body is small relative to other joint structures constituting spinal segments, such as the uncovertebral and facet joints, the load applied to the cervical vertebrae will not be greater than that of the lumbar spine [19,20].
The incidence of cage subsidence was quite different in the literature and reported to be higher following ACDF alone than when combined with anterior plating [4,7,21]. Schmieder et al. [10] performed ACDF using only a titanium cage without anterior plate augmentation, and the subsidence rate was 44.8% (30 of 67). In a randomized prospective study, Kast et al. [6] reported a subsidence rate of 29% following ACDF alone using a PEEK cage. In our series, the overall incidence of cage subsidence was 14.29% (group A, 13.9%; group B, 16.0%), which was less than that reported by most other studies on stand-alone cages. In this study, most cage subsidence cases occurred approximately 1 month postoperatively. In addition, gradual cage subsidence, which would have destroyed the anterior cervical column, was not observed.
The clinical significance of cage subsidence remains unclear. According to some authors, segmental height loss of up to 2 mm is defined as “implant settling” or “minor subsidence,” and height loss above that value is referred to as “major subsidence” [6]. However, determining absolute values from simple radiographs is difficult.
Studies have suggested that cage subsidence is associated with symptomatic deterioration after cervical spine surgery [10,21]. Subgroup analysis was performed based on the presence or absence of cage subsidence. Subgroup analysis revealed significantly lower fusion rates in patients with cage subsidence. Segmental instability resulting from cage subsidence may affect the fusion rate. However, no significant difference in the clinical outcomes was found between the groups with and without cage subsidence.
Pseudarthrosis following anterior cervical fusion surgery increases the likelihood of poor clinical outcomes, such as sustained neck pain and recurrent radiculopathy, occasionally leading to revision surgery [22]. The overall pseudarthrosis rate following ACDF varies from 2.6% to 30%, with a higher rate for multilevel surgery [15,23]. The varying pseudarthrosis rates reported in the literature result from differences in surgical techniques, detection methods, diagnostic criteria, and study design. In this study, the pseudarthrosis rates 1 year postoperatively were 17% (17/100) in group A and 31.8% (7/22) in group B. However, without any intervention, many patients with pseudarthrosis achieved successful fusion after 2 years. The pseudarthrosis rate at the final follow-up decreased in both groups (group A, 5.4%; group B, 13.6%). The results of this study demonstrated that patients with normal BMDs had a higher fusion rate at the 1-year and 2-year follow-ups; however, the difference was not statistically significant. Although the results were not statistically significant, patients with osteoporosis have slower and less reliable bone healing, which could contribute to a higher likelihood of pseudarthrosis.
The results of the subgroup analysis revealed that cage subsidence occurred more frequently in male patients. At our institution, patients are recommended to wear cervical collars for at least 6 weeks postoperatively to prevent excessive cervical motion. Although male patients had greater average bone mineral densities than female patients, they also had significantly greater absolute neck muscle strength and head mass weights than female patients [19]. A possible explanation is that increased isometric torque during neck movement in the early postoperative period can cause greater axial and rotational stress at the interbody/cage interface, which can result in cage subsidence before solid fusion in male patients.
When performing ACDF, cages are inserted to maintain the efficacy of the decompressed disc space and support the anterior column of the cervical spine [24]. However, overdistraction of the disc space can increase the risk of cage subsidence [3]. According to Yamagata et al. [25], a cage of 6.5 mm or 7.5 mm for ACDF resulted in a higher rate of subsidence than a cage of 4.5 mm or 5.5 mm. In our subgroup analysis, according to the presence or absence of plate migration, plate-/screw-related complications occurred more frequently in the group with greater disc height changes postoperatively. Thus, the results of this study suggest that excessive distraction of the disc height should be avoided to reduce the risk of potential cage subsidence during ACDF.
This study has some limitations. First, it follows a retrospective design and lacks randomization between the groups. Second, BMD measured in the lumbar spine was used to evaluate bone quality because no studies are currently investigating the measurement of cervical spine-specific bone quality and standard values for osteoporosis. Although this is a generally accepted method for diagnosing osteoporosis, it has limitations in representing cervical spine-specific bone quality. Third, the long-term consequences of cage subsidence and plate migration were not evaluated. Finally, the relatively small sample size in group B raises concerns about its potential to exert a significant influence on the overall result. Despite these limitations, this direct comparison of patients with and without osteoporosis offers a foundation for future explanations of how the condition affects the outcomes of cervical fusion surgery.
Conclusions
Osteoporosis did not significantly affect the rate of cage subsidence or implant migration after cervical fusion. In addition, higher cage subsidence and implant migration rates following ACDF did not significantly affect clinical outcomes. Thus, ACDF with anterior plating may be a good option for achieving good clinical outcomes in patients with osteoporosis. However, a lower fusion success rate is associated with a higher rate of cage subsidence, which occurs more frequently in male patients and in those with greater disc height changes. Therefore, surgeons should be careful not to overdistract during surgery to reduce implant-related complications because they are related to cage subsidence and nonunion.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conception and design: CGH, DHL; data acquisition and analysis of data: CGH, YJL, WDN; drafting a manuscript: CGH, YJL; manuscript review & editing: CGH, YJL, DHL; critical revision: CGH, DHL; administrative support: CGH, WDN; supervision: CGH, DHL; and final approval of the manuscript: all authors.