 |
 |
- Search
| Asian Spine J > Volume 14(1); 2020 > Article |
|
Abstract
Purpose
To compare the incidence of iatrogenic superior facet joint violation (SFV) in minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) and open TLIF (OPEN-TLIF) at a single lower lumbar fusion level and to evaluate the patient and surgical factors influencing the outcome.
Overview of Literature
Iatrogenic SFV is a significant risk factor for adjacent segment disease (ASD). Blind screw placement technique in MIS-TLIF contributes to the increasing incidence of iatrogenic SFV which can be influenced by several other potential factors. There are only limited studies comparing the incidence of iatrogenic SFV in MIS-TLIF and OPEN-TLIF.
Methods
In total, 225 cases (450 top screws; MIS-TIFL, 120; OPEN-TILF, 105) undergoing single-level lower lumbar fusion were included in the study. Postoperative computed tomography grading system was used to evaluate iatrogenic SFV. Patient and surgical factors such as age, body mass index, top-screw level, side of the top screw, depth of the spine, and superior facet joint angle (SFA) were analyzed in iatrogenic SFV and non-violation groups to determine their influence on iatrogenic SFV. The clinical outcomes in both groups were assessed preoperatively and postoperatively.
Results
The overall incidence of iatrogenic SFV and high-grade violations was higher in MIS-TLIF (41.25%) than in OPEN-TLIF (30.4%). In both groups, bivariate analysis showed a significantly greater incidence of the iatrogenic SFV in patients aged <60 years and those with obesity, top pedicle screws at L4, right-sided top screws, SFA >35°, and depth of the spine >50 mm.
Conclusions
This study demonstrated that the incidence of iatrogenic SFV is greater in MIS-TLIF than in OPEN-TLIF at a single lower lumbar level. MIS-TLIF is effective for lumbar degenerative disease; however, the incidence of iatrogenic SFV was higher. Patient and surgical factors must be considered to protect the facet joints in both TLIF methods to avoid ASD.
The conventional open transforaminal lumbar interbody fusion (OPEN-TLIF) is reportedly successful in treating various symptomatic lumbar spine diseases; however, disadvantages such as extensive muscle dissection, increased blood loss, and prolonged recovery time continue to remain a major concern [1,2]. Minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) has become a popular alternative to address the disadvantages of OPEN-TLIF [2,3]. However, one major concern for MIS-TLIF is its reliance on fluoroscopic guidance rather than direct visualization of anatomic landmarks to insert pedicle screws. With the loss of visualization and lack of tactile perception, the risk of iatrogenic superior facet joint violation (SFV) increases, contributing to biomechanical changes like abnormal facet joint loading and motion, ultimately leading to adjacent segment disease (ASD) [4]. At 10 years, the rate of symptomatic ASD at an adjacent segment requiring reoperation is 36.1% [5], illustrating the urgent need to avoid iatrogenic SFV to decrease healthcare spending by reducing reoperations and improving patient safety and quality of life.
To the best of our knowledge, no study has yet directly compared the incidence of iatrogenic SFV in MIS-TLIF and OPEN-TLIF at a single lower lumbar level. The present study aimed to investigate the incidence of iatrogenic SFV in MIS-TLIF and OPEN-TLIF and to elucidate the factors influencing this incidence with surgeons routinely performing both techniques. Several studies have reported risk factors such as age, sex, weight, and top-screw level impact on iatrogenic SFV in percutaneous pedicle screw placement [6,7]. However, consensus on the etiology of iatrogenic SFV is lacking, mainly due to mixed findings from previous studies [7,8]. Moreover, clinical outcomes of different grades of iatrogenic SFV in patients undergoing MIS-TLIF and OPEN-TLIF have not been analyzed. In this study, we prospectively analyzed 225 cases (450 top screws) of patient who underwent single-level lower lumbar MIS-TLIF and OPEN-TLIF procedures. Incidence of iatrogenic SFV, relevant risk factors, and superior facet joint angle (SFA) were recorded. Comprehensive understanding of the factors involved in different levels of iatrogenic SFV and how they are correlated with clinical outcomes is a critical component in avoiding revision surgery for symptomatic ASD, a knowledge gap of which this study aims to support.
This prospective comparative study was reviewed and approved by the Human Ethics Committee of the Bombay Hospital and Medical Research Centre (IRB approval no., 145/09/2019). Informed consent was obtained from all individual participants included in the study. In total, 225 patients including 120 MIS-TLIF and 105 OPEN-TLIF who underwent single-level lower lumbar fusion from July 2014 to December 2018 were included. The inclusion criteria consisted of patients with lower lumbar canal stenosis with or without spondylolisthesis and in whom preoperative computed tomography (CT) scan was done for various reasons. Patients with revision surgery, spinal tumors, degenerative lumbar scoliosis, and other spinal conditions were excluded from the study. There were no significant differences found between the mean age, gender, the mean body mass index (BMI), and the indications in MIS-TLIF and OPEN-TLIF cases. As all patients had screws placed bilaterally, this study evaluated a total of 450 top screws. Table 1 demonstrates that the MIS-TLIF and OPEN-TLIF groups had a similar baseline and surgical demographics.
Patients who underwent MIS-TLIF had screws placed through paramedian incisions approximately 2 cm long and 3–5 cm lateral to the midline. The pedicle was cannulated with a Jamshidi needle under anteroposterior and lateral fluoroscopic guidance. The needles were exchanged for guidewires. The serial dilators were used to dilate over the guidewires, and the pedicles were tapped using a cannulated tap. Screws were placed with corresponding screw extenders, and the rod was introduced with a device through a separate proximal stab incision. After placement of locking-cap screws through the screw extenders and with application of compression, the screws were torqued, and the screw extenders were removed [9] (Fig. 1).
The appropriate level of the spine was exposed after radiographic identification. The posterior elements were subperiosteally exposed to the tips of the transverse processes. Pedicle screws were placed without fluoroscopy, basing on the anatomical landmarks. A starting hole was made at the intersection of the mid-transverse process, pars, and superior articular facet. The pedicle was cannulated with a pedicle probe, and the track was palpated with a ball-tipped probe to ensure no cortical breach had occurred. The hole was then tapped, and a screw of appropriate diameter was placed based on the surgeon’s discretion. The basic steps of TLIF were followed in both methods [9] (Fig. 2).
The CT scan with sagittal and axial reconstructive images adjusted parallel to the pedicle screws was used to evaluate iatrogenic SFV in all patients within 3–4 weeks of surgery. The grading criterion for iatrogenic SFV was established prior to the CT scan review (Table 2) [8]. Grade 0 was labeled for screws not in the facet joint and which did not encroach upon the joint. If the screw was in the lateral facet but did not enter the articular facet, it was labeled as grade 1. Screws that penetrated the articular facet by ≤1 mm were assigned a grade 2 violation, and those screws traveling within the articular surface of the facet were given a grade 3 designation (Fig. 3). Preoperative cross-sectional CT scan was used to measure the SFA (the angle between the facet joint and the sagittal axis of the vertebral body) at the pedicle level [10] (Fig. 4). Two of the authors reviewed the CT images independently to determine iatrogenic SFV on both sides. The inter- and intra-observer Pearson R coefficients were 0.98 and 1.0, respectively. Iatrogenic SFV in relation to age, obesity (the World Health Organization defines a BMI of 30 kg/m2 or above as obese), top-screw level, side of the top screw, SFA, and depth of the spine was analyzed. Clinical data like length of time of operation, blood loss, and postoperative drainage were collected to compare the therapeutic efficacy of both methods. Visual Analog Scale (VAS) and the Oswestry Disability Index (ODI) were also employed to assess functional outcome in the SFV and the non-SFV groups.
All data were expressed as means±standard deviation. Chi-squared analysis was carried out to determine the association between iatrogenic SFV and various technical factors. The incidence of iatrogenic SFV, considering the total top screws (n=450), was 41.25% in MIS-TLIF and 30.4% in OPEN-TLIF. The CT scans showed 59 screws with grade 1 SFV (24.5%), 25 screws with grade 2 SFV (10.4%), and 15 screws with grade 3 SFV (6.25%) in 240 top screws in MIS-TLIF cases. Among the total 210 top screws in OPEN cases, 45 screws were with grade 1 SFV (21.4%), 11 screws with grade 2 SFV (5.2%), and eight screws with grade 3 SFV (3.8%). The study also showed that pedicle screw placement at L4 had a higher incidence of iatrogenic SFV with 15.3% in OPEN-TLIF and 25% in MIS-TLIF cases (Table 3). Moreover, logistic regression analysis showed that iatrogenic SFV was closely related to BMI with incidence of 15.2% in OPEN-TLIF and 24.2% in MIS-TLIF in patients with BMI >30 kg/m2 which was significantly higher than those with BMI <30 kg/m2. The study also found that the incidence of iatrogenic SFV was 17.27% in cases with the SFA <35° and 30% in cases with the SFA >35° (Table 3). We also found a higher incidence of facet violation for all grades in patients aged <60 years (15.4% in OPEN-TLIF and 25.8% in MIS-TLIF cases). The increased depth of the spine (>50 mm in our study) was also significantly associated with the higher incidence of iatrogenic SFV in both TLIF procedures. We also found a significantly higher incidence of iatrogenic SFV for grades 1 and 2 on the right-sided top screws in both methods but non-statistically significant result for grade 3 between the two groups. There was a significant statistical difference in the mean operative time, mean average blood loss, and mean postoperative drainage between the two groups. The VAS and ODI scores for low back and leg 3 weeks postoperatively significantly improved in the non-iatrogenic SFV group compared to the iatrogenic SFV group (Table 4).
Both OPEN-TLIF and MIS-TLIF are more commonly performed nowadays in the treatment of various lumbar disorders, but postoperative complications including ASD still pose a significant concern for surgeons [11]. Specifically, biomechanical studies reveal increased tensile and shearing stresses and increased facet loads, heightening the possibility of degenerative changes after facet violation with screws [4]. After a 10-year lumbar fusion surgery follow-up in 1,069 cases, Lee et al. [12] found that degeneration of facet joint following transpedicular screw fixation played a critical role in the progression of ASD.
We describe a direct comparison of the incidence of iatrogenic SFV in MIS-TLIF and OPEN-TLIF techniques performed at a single lower lumbar level. In our series, the overall incidence of iatrogenic SFV and the incidence of grade 3 violations were significantly higher in the MIS-TLIF group compared to the OPEN-TLIF group, as these cases rely on radiographic and limited tactile feedback for determination of screw entry site and trajectory. In contrast, the open approach allows for direct visualization of the facet. Even with perfect fluoroscopic images, a slightly poor choice of entry site or too much medial angulations can result in a violation. A thorough review of the literature demonstrates that it is unclear whether open or percutaneous pedicle screw placement results in more facet violations [13-16]. Moshirfar et al. [17] evaluated 204 patients who underwent open screw placement and found that 24% of the cases had cranial facet joint violations. Another study by Shah et al. [11] evaluating facet joint violation during open procedures found violations in 37 of 106 patients (35%). A study by Chen et al. [6] revealed a 100% incidence of facet violation using the Roy-Camille method but only 36% when the Weinstein method was used, establishing the fact that the incidence of facet joint violation varies depending on the method of pedicle screw insertion. Also, a cadaveric study performed to evaluate facet violations with percutaneous pedicle screw placement found a 58% incidence of violations after the placement of 28 screws [18].
Physical conditions play an important role in the development of the iatrogenic SFV and ASD during MIS-TILF [19-23]. Babu et al. [8] found that SFV occurred frequently in patients <65 years old by retrospectively analyzing 279 patients who underwent minimally invasive surgery, while we found a higher violation in patients with <60 years of age explaining similar results. They considered that the pedicle screw placement was affected in younger patients due to their stronger muscle [8]. However, Park et al. [5] held a different point that SFV had no correlation with age and gender. In our study, we found that obese (30 kg/m2) patients were vulnerable to iatrogenic SFV. A potential reason for this could be that the puncture and Jamshidi needle moves easily during screw insertion, which can cause severe damage to the facet joint. Better anesthesia and fluoroscopy imaging techniques can potentially help avoid this damage in obese patients. Most studies suggested that iatrogenic SFV occurred in L4 and L5 more often than L1, L2, and L3. Anatomical studies confirm that the direction of facet joint articular surfaces transferred from sagittal to a coronal plane in the lumbar vertebrae [24]. In this study, among 218 top screws at L4 level, the iatrogenic SFV occurred in 85 screws (38.9%). This could be due to the articular surface of the L4 facet joint in a more coronal presentation. Among 450 total screws on both sides, the incidence of the iatrogenic SFV on the right side was 16% in OPEN-TLIF and 24.8% in MIS-TLIF, while on the left side, it was 12.4% and 19.1%, respectively. A positive correlation was found between the increase of the SFA (>35°) at the pedicle level and depth of the spine >50 mm with the iatrogenic SFV [10]. In a study of Jia et al. [25], the results showed that SFV incidence was 39.39% of the patients and 23.23% of the screws in MIS-TLIF. Logistic regression analysis also showed that screw at L5 in patients with BMI >30 kg/m2 was vulnerable to SFV as seen in our study. Three-dimensional CT navigation was employed perioperatively to help navigate screw insertion, which greatly reduces the damage of facet joints, while fluoroscopy was used in our study [25].
The results of a study of Zeng et al. [26] found a high incidence of adjacent superior vertebral facet joint violation in the MIS-TLIF. Age <60 years old and BMI ≥30 kg/m2 could be viewed as predisposing factors of facet joint violation, supporting the results of our study [26].
Selecting patients with the same indication for lumbar fusion was done to minimize biases in this study. Additionally, our rates of the iatrogenic SFV are similar to those found in the literature. Although we suggest that iatrogenic SFV contributes to the development of post-fusion ASD, the small sample size of patients with short-term follow-up does not allow for conclusive statements about the role iatrogenic SFV may have, and there are many other factors which may contribute to this effect. Finally, the grading scale used in this study was developed for descriptive purposes. This scale has not yet been validated, and future studies are needed to determine the impact of iatrogenic SFV on the clinical setting.
The results of this study showed that MIS-TLIF is associated with a higher incidence of iatrogenic SFV compared to the traditional OPEN-TLIF approach for a single lower lumbar level. The incidence is greater in patients who are <60 years of age and obese (BMI >30 kg/m²) and in L4 top screws, right-sided screws, cases with SFA >35°, and spine depth of >50 mm. As iatrogenic SFV may have potential to increase the risk of ASD, it is vital therefore to limit or reduce occurrence of these injuries. This study will help spine surgeons limit this complication by providing knowledge of the patient and operative factors with the greatest risk.
Fig. 1.
Minimally invasive transforaminal lumbar interbody fusion preoperative (A) and postoperative (B) X-ray.
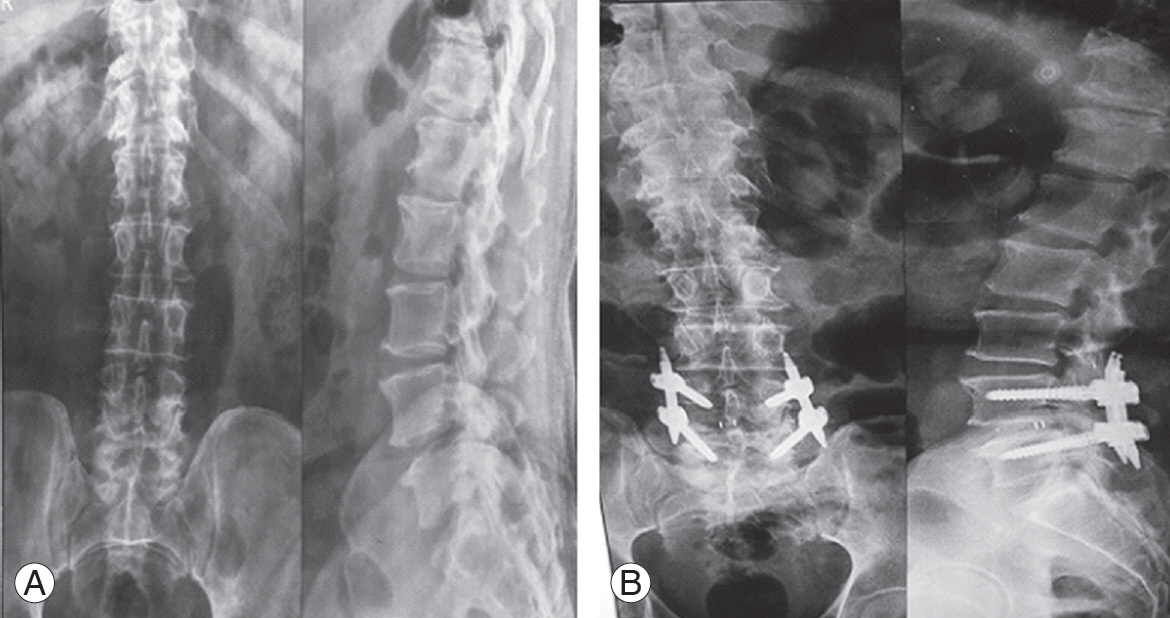
Fig. 3.
Different grades of iatrogenic superior facet joint violation. (A) Grade 1. (B) Grade 2. (C) Grade 3.

Fig. 4.
Facet joint angle measurement. Three red dots represent the medial, lateral, and central part of pedicle (width of pedicle). From Xu et al. Medicine (Baltimore) 2018;97:e10943 [10]. FA, facet angle.

Table 1.
Patient and surgical demographic data
Table 2.
Facet violation radiographic grading
Table 3.
Incidence of the iatrogenic SFV
Table 4.
Clinical outcome: the iatrogenic SFV and non-SFV groups
References
1. Hackenberg L, Halm H, Bullmann V, Vieth V, Schneider M, Liljenqvist U. Transforaminal lumbar interbody fusion: a safe technique with satisfactory three to five year results. Eur Spine J 2005;14:551–8.




2. Rosenberg WS, Mummaneni PV. Transforaminal lumbar interbody fusion: technique, complications, and early results. Neurosurgery 2001;48:569–74.



3. Schwender JD, Holly LT, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech 2005;18 Suppl:S1–6.


4. Rao RD, David KS, Wang M. Biomechanical changes at adjacent segments following anterior lumbar interbody fusion using tapered cages. Spine (Phila Pa 1976) 2005;30:2772–6.


5. Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 2004;29:1938–44.


6. Chen Z, Zhao J, Xu H, Liu A, Yuan J, Wang C. Technical factors related to the incidence of adjacent superior segment facet joint violation after transpedicular instrumentation in the lumbar spine. Eur Spine J 2008;17:1476–80.




7. Patel RD, Graziano GP, Vanderhave KL, Patel AA, Gerling MC. Facet violation with the placement of percutaneous pedicle screws. Spine (Phila Pa 1976) 2011;36:E1749–52.


8. Babu R, Park JG, Mehta AI, et al. Comparison of superior-level facet joint violations during open and percutaneous pedicle screw placement. Neurosurgery 2012;71:962–70.




9. Jones-Quaidoo SM, Djurasovic M, Owens RK 2nd, Carreon LY. Superior articulating facet violation: percutaneous versus open techniques. J Neurosurg Spine 2013;18:593–7.


10. Xu Z, Tao Y, Li H, Chen G, Li F, Chen Q. Facet angle and its importance on joint violation in percutaneous pedicle screw fixation in lumbar vertebrae: a retrospective study. Medicine (Baltimore) 2018;97:e10943.



11. Shah RR, Mohammed S, Saifuddin A, Taylor BA. Radiologic evaluation of adjacent superior segment facet joint violation following transpedicular instrumentation of the lumbar spine. Spine (Phila Pa 1976) 2003;28:272–5.


12. Lee CS, Hwang CJ, Lee SW, et al. Risk factors for adjacent segment disease after lumbar fusion. Eur Spine J 2009;18:1637–43.




13. Sears WR, Sergides IG, Kazemi N, Smith M, White GJ, Osburg B. Incidence and prevalence of surgery at segments adjacent to a previous posterior lumbar arthrodesis. Spine J 2011;11:11–20.


14. Ghiselli G, Wang JC, Bhatia NN, Hsu WK, Dawson EG. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am 2004;86:1497–503.


15. Yson SC, Sembrano JN, Sanders PC, Santos ER, Ledonio CG, Polly DW Jr. Comparison of cranial facet joint violation rates between open and percutaneous pedicle screw placement using intraoperative 3-D CT (O-arm) computer navigation. Spine (Phila Pa 1976) 2013;38:E251–8.


16. Park Y, Ha JW, Lee YT, Sung NY. Cranial facet joint violations by percutaneously placed pedicle screws adjacent to a minimally invasive lumbar spinal fusion. Spine J 2011;11:295–302.


17. Moshirfar A, Jenis LG, Spector LR, et al. Computed tomography evaluation of superior-segment facet-joint violation after pedicle instrumentation of the lumbar spine with a midline surgical approach. Spine (Phila Pa 1976) 2006;31:2624–9.


18. Chung KJ, Suh SW, Swapnil K, Yang JH, Song HR. Facet joint violation during pedicle screw insertion: a cadaveric study of the adult lumbosacral spine comparing the two pedicle screw insertion techniques. Int Orthop 2007;31:653–6.



19. Rahm MD, Hall BB. Adjacent-segment degeneration after lumbar fusion with instrumentation: a retrospective study. J Spinal Disord 1996;9:392–400.


20. Pellise F, Hernandez A, Vidal X, Minguell J, Martinez C, Villanueva C. Radiologic assessment of all unfused lumbar segments 7.5 years after instrumented posterior spinal fusion. Spine (Phila Pa 1976) 2007;32:574–9.


21. Kim HJ, Chun HJ, Kang KT, et al. The biomechanical effect of pedicle screws’ insertion angle and position on the superior adjacent segment in 1 segment lumbar fusion. Spine (Phila Pa 1976) 2012;37:1637–44.


22. Schulte TL, Leistra F, Bullmann V, et al. Disc height reduction in adjacent segments and clinical outcome 10 years after lumbar 360 degrees fusion. Eur Spine J 2007;16:2152–8.




23. Bae JS, Lee SH, Kim JS, Jung B, Choi G. Adjacent segment degeneration after lumbar interbody fusion with percutaneous pedicle screw fixation for adult low-grade isthmic spondylolisthesis: minimum 3 years of follow-up. Neurosurgery 2010;67:1600–7.



24. Van Schaik JP, Verbiest H, Van Schaik FD. The orientation of laminae and facet joints in the lower lumbar spine. Spine (Phila Pa 1976) 1985;10:59–63.









