|
 |
- Search
| Asian Spine J > Volume 17(5); 2023 > Article |
|
Abstract
Purpose
To compare the clinical outcomes and radiological findings of revision discectomy alone versus revision discectomy with fusion as surgical treatment for recurrent lumbar disc herniation (RDH).
Overview of Literature
RDH is a common complication following a primary discectomy. The optimal surgical procedure for RDH is still debated.
Methods
Sixty patients with RDH were randomly divided into two equal groups: the first group underwent revision discectomy alone and the second underwent revision discectomy with fusion. The primary outcomes evaluated were Visual Analog Scale (VAS) for low back and limb pains, Oswestry Disability Index (ODI), disc height indexes, foraminal height index, and disc height subsidence. Secondary outcomes included operative time, blood loss, postoperative hospital stay, and complications.
Results
Revision discectomy with fusion showed superior pain relief and improved functional outcomes, including better VAS scores for both back and leg pain and ODI at 24-month follow-up. Additionally, it restored the stability of the spine better with lower disc height subsidence without significant complications. However, these advantages came at the cost of increased blood loss and longer operative time and hospital stays.
Recurrent lumbar disc herniation (RDH) occurs in 5%ŌĆō25% patients undergoing discectomy and is defined as the presence of herniated disc material at the same level, whether ipsilateral or contralateral, in a patient who has experienced a pain-free interval of at least 6 months following initial discectomy [1,2]. Almost half of all recurrent herniations occur within the first year of the index operation; nevertheless, re-herniation may occur within 8 years after the initial procedure [3].
Multiple studies have examined the risk factors attributed to an increased rate of re-herniation [1]. Old age, male gender, smoking, obesity, diabetes mellitus, heavy work, and lack of regular physical activity were reported as significant predictors for RDH [4ŌĆō9]. The increased disc height and segmental motion are associated with a high recurrence risk [10]. Furthermore, a sagittal range of motion (at the disc level) greater than 10┬░ is associated with a higher recurrence rate of 26.5% compared with a recurrence rate of 4.1% in patients with a range of motion less than 10┬░ [11].
The management of RDH includes nonoperative and operative treatment. Symptomatic patients without neurologic deficits should certainly be considered for nonoperative interventions [12]. Indications for operation are intractable pain that had not responded to conventional management for 6ŌĆō8 weeks, positive tension sign, and recurrent disc herniation with compression of the nerve root confirmed by magnetic resonance imaging (MRI) [13]. Operative intervention mainly comprised two surgical techniques: discectomy alone or discectomy with fusion [3]. However, the debate on which procedure would be the most effective for these patients remains unresolved [14].
Some authors have proposed that repeat discectomy alone is often successful in treating patients with RDH unless patients have an absolute indication for instrumented fusion [15]. It is characterized by less intraoperative blood loss and shorter durations of surgery and postoperative hospital stay than revision discectomy with fusion [14]. However, concerns over repeat RDH may lead many surgeons to advocate instrumented fusion in the absence of instability [16].
Revision discectomy with fusion reduces the postoperative incidence of mechanical instability that tends to occur following the repeated surgeries and decreases the intraoperative risk of dural tear [4]. However, this procedure has its own challenges, such as higher blood loss, longer operative duration and hospitalization time, more complications, and extra cost due to the more expensive materials used [4ŌĆō14,17].
In summary, we state that there is no level I evidence indicating the superiority of one approach over another and that there is no clear recommendation for the surgical treatment of RDH [3,18]. Thus, the aim of this study was to compare the benefits and drawbacks of revision discectomy alone versus revision discectomy with fusion via clinical outcomes and radiological findings.
The current study is a prospective randomized comparative clinical study of 60 patients with RDH who underwent redo-discectomy with or without fusion at Cairo University Hospitals and Nile Badrawy Hospital between October 2018 and January 2022. This study was approved by the Ethical Committee of the Orthopedic Department, Cairo University. Inclusion criteria were patients with RDH confirmed by MRI, who had at least 6 months of pain relief after primary disc surgery, aged between 20 to 70 years and the absence of instability. Patients with multiple levels of disc herniation, spine instability, cauda equina syndrome, inflammatory disease, or any concurrent medical condition that contraindicates further surgery were excluded from the study. Eligible patients were informed in detail about the operative procedures, including potential complications and subsequent postoperative management, and their written consent was obtained prior to the surgery. They were randomized by the sealed envelope method into two groups each consisting of 30 patients: group A underwent revision microdiscectomy alone and group B underwent revision discectomy with fusion by pedicle screws and transforaminal lumbar interbody fusion (TLIF) cage application from the ipsilateral side of disc herniation and posterolateral fusion on the contralateral side using autogenous local bone graft. All surgeries were performed by a senior spine surgeon with 14 years of experience. Personal and demographic patient data were recorded including gender, age, marital status, occupation, special habits e.g., smoking, history of present illness, past medical history, and complete past surgical history including the date of previous surgical procedure.
Comparative evaluation of the two groups was conducted via clinical and radiological assessments and assessment of secondary outcomes. Clinical assessment was performed using Visual Analog Scale (VAS) [19] to evaluate low back and limb pains, together with the Oswestry Disability Index (ODI) [20] to assess the disability. VAS and ODI were performed preoperatively; immediately postoperation; and at 1, 3, 6, 9, 12, and 24 months postoperation. Preoperative radiological assessment was conducted through MRI with contrast and plain lumbosacral radiographs (anterior-posterior [AP], lateral, and dynamic views). Plain lumbosacral radiographs (AP and lateral) at 6, 12, and 24 months postoperation were used for postoperative radiological assessment. To calculate the amount of subsidence, the intervertebral disc height index (DHI) and foraminal height index (FHI) were measured preoperatively, postoperatively and at the last follow-up in accordance with KimŌĆÖs method [10]. The subsidence was calculated as the difference in DHI immediately postoperation and at the last follow-up [10]. Secondary outcome parameters, including surgery time, blood loss, hospital stay, and intra and postoperative complications were recorded.
Statistical analysis was performed using independent-samples t-test and chi-square test by IBM SPSS software ver. 23.0 (IBM Corp., Armonk, NY, USA). Results were considered statistically significant when the p-value was Ōēż0.05.
The demographic data of the two study groups are presented in Table 1. The mean age of the revision discectomy group was 40.87 years compared to 46.2 years of the revision discectomy with fusion group. A positive smoking history was recorded in 10 patients of group A (33.3%) and in six patients of revision discectomy with fusion group B (20%). No statistically significant difference between the two groups with respect to these findings was identified. The same was observed for associated comorbidities, spinal affection, and the side of limb pain, which also revealed no statistical difference between the two groups.
The operative data of the two study groups are presented in Table 2. The revision discectomy with fusion group exhibited significantly longer operative time and hospital stay and higher amount of blood loss than that of the revision discectomy alone group.
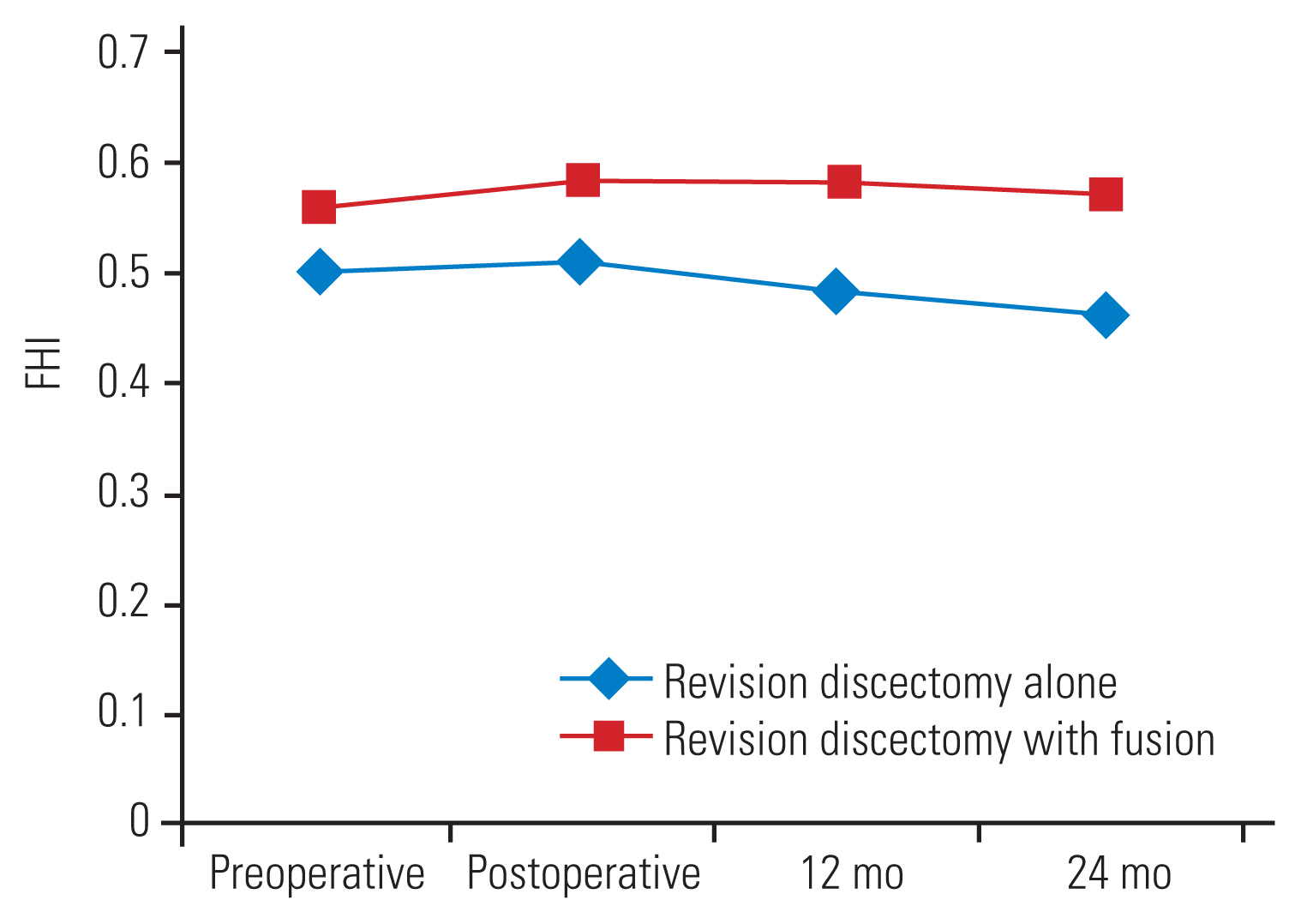
The VAS scores for severity of back and limb pains at various follow-up intervals are presented in Fig. 1. The results indicated that there was no significant difference in VAS for back pain between the two groups preoperatively; postoperatively; and at 1-, 3-, and 6-month follow-ups. However, at 9-, 12-, and 24-month follow-ups, VAS for back pain in the revision discectomy with fusion group was significantly lower than that in the revision discectomy alone group (with p-values of 0.048, 0.046, and 0.008 at 9, 12, and 24 months, respectively) (Table 3).
With respect to VAS for limb pain, there was no significant difference between the two groups preoperatively; postoperatively at 1, 3, and 6 months; and at 9-month follow-up. However, it was significantly lower in group B than in the revision discectomy alone for group A at 12- and 24-month follow-ups (with p-values of 0.04 and 0.001 at 12- and 24-month follow-ups, respectively) (Table 3).
With respect to ODI, results showed no significant difference between the two groups preoperatively; postoperatively; and at 1-, 3-, and 6-month follow-ups. However, at 9-, 12-, and 24-month follow-ups, ODI in revision discectomy with fusion group B showed significantly lower values than those in group A (Table 4).
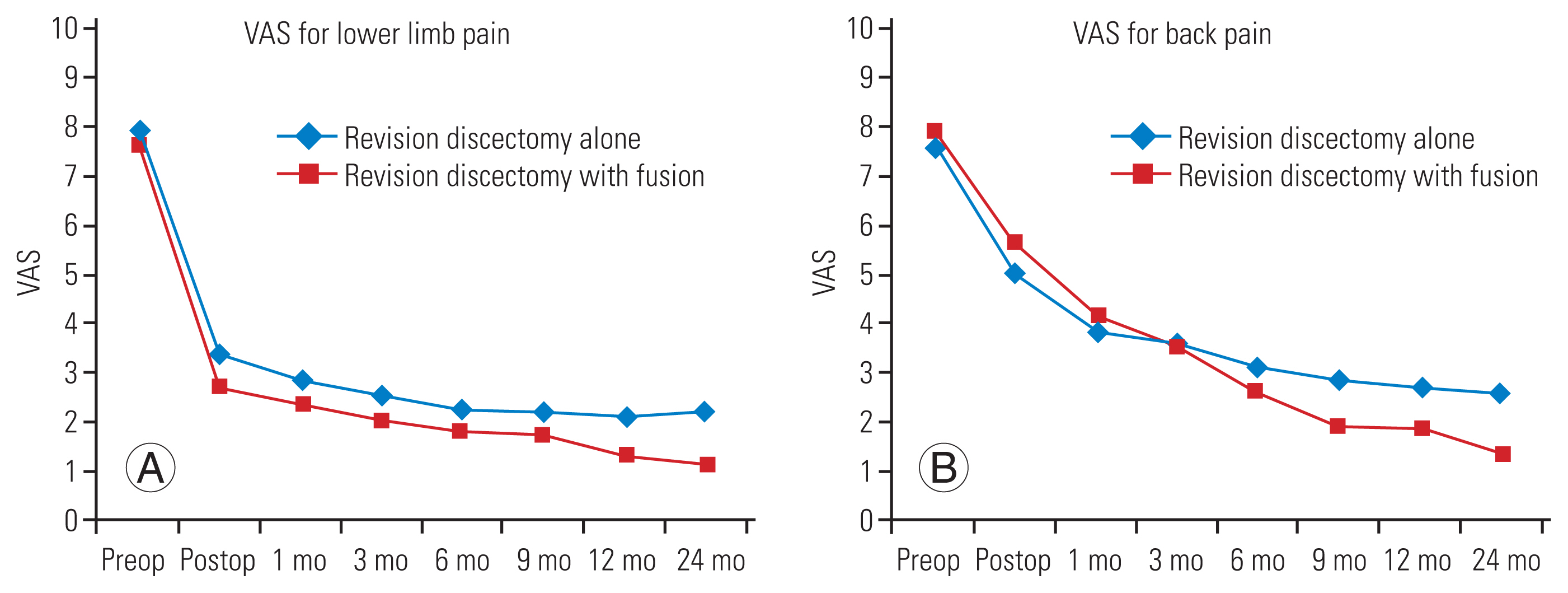
DHI and FHI were measured preoperatively and postoperatively at 12 and 24 months and are presented in Figs. 2 and 3, respectively. Preoperative and postoperative DHI in group A showed nearly the same values, after 12 months, the DHI decreased by 9.5% without significant difference. In contrast, in the fusion group B, there was a significant increase in the DHI directly postoperation in comparison with preoperative DHI (10.3% increase), and the value of DHI remained nearly unchanged at 24-month follow-up.
FHI exhibited similar results, as there was no statistical difference between preoperative (FHI) of the two groups (p=0.272). In revision discectomy group A, there was 5% decrease in FHI at 12- and 24-month follow-ups without any significant difference. In the fusion group B, a significant increase was observed in FHI postoperatively (4.6%) which remained nearly unchanged at 24-month follow-up (p=0.006).
With respect to subsidence, revision discectomy without fusion group A showed a significantly higher degree of subsidence (mean┬▒standard deviation [SD], 0.023┬▒0.01; range, 0.007ŌĆō0.04) than that of fusion group B (mean┬▒SD, 0.00253┬▒0.0022; range, 0ŌĆō0.007) (p<0.0001).
Complications in both groups are summarized in Table 5 and can be divided into two categories. Intraoperative complications: 10 dural tears were recorded throughout the entire hospitalization period (16.7%); six patients (20%) in the revision discectomy with fusion group B and four patients (13.3%) in the re-discectomy alone group A. All dural tears were repaired during the operation and no cerebrospinal fluid leaks were observed postoperation. Four patients (13.3%), belonged to group B required blood transfusion. Postoperative complications: overall 26 patients (43.3%) experienced paresthesia; 10 (33.3%) were in the revision discectomy alone group A and 16 (53.3%) were in group B. All these patients improved with conventional treatment. Four patients, that is two patients in each group (13.3%) experienced superficial infection and all improved with conventional treatment.
Revision spinal surgery is often more challenging than primary surgery because the surgeon faces challenges, such as scar tissue and altered anatomical landmarks [21].
Due to the lack of comparative comprehensive studies and their inconsistent results, the optimal surgical technique for treating RDH remains controversial [22]. Hence, the objective of this study was to conduct direct comparative evaluation of revision discectomy alone versus revision discectomy with fusion as surgical treatment procedures for RDH through the assessment of clinical outcomes and radiological findings.
The underlying results demonstrated that the demographic data of the two study groups were homogeneous and comparable. Regarding the operative data, group B exhibited significantly longer operation time and hospital stay and higher amount of blood loss than group A. Nearly all previous reports reported similar findings. Awad and Faisel [23] compared conventional redo-discectomy to TLIF with unilateral pedicle screw fusion as surgical procedure for RDH and observed that the conventional re-discectomy group had less intraoperative blood loss and shorter operative time and hospital stay. Similarly, Khayat et al. [24] who assessed fusion versus nonfusion to identify the ideal treatment method for RDH reported comparable findings. Furthermore, a systematic review and meta-analysis in 2019 comparing outcomes of fusion versus repeat discectomy in RDH reported that operative time and postoperative hospital stay were significantly lower in the re-discectomy group [25].
The application of screws and cage during the fusion technique requires additional time which leads to longer operative time, more blood loss, and lengthier hospital stay as this is tedious approach.
The clinical outcomes revealed that there is significant improvement in pain and disability after surgery in both groups. Comparing the VAS scores and ODI of the two groups at each time interval revealed that revision discectomy with fusion led to significantly lower VAS score for back pain and significantly lower ODI at 9-, 12-, and 24-month follow-ups. In addition, revision discectomy with fusion resulted in significantly lower VAS score for leg pain at 24-month follow-up. Therefore, revision discectomy with fusion demonstrated a superior clinical outcome during intermediate-term follow-up.
Consistent with previous findings, Awad and Faisel [23] reported that patients operated by TLIF experienced less pain and lower disability scores throughout the follow-up period than those operated with conventional redo-discectomy [26]. Moreover, a systematic review aiming to compare treatment options for RDH concluded that discectomy with fusion resulted in greater improvement in pain and functional outcomes compared to discectomy alone [27].
However, reported clinical outcomes displayed a notable inconsistency. A systematic review and meta-analysis in 2018 comparing the outcomes of fusion versus repeat discectomy in RDH reported that the changes in VAS-back pain, VAS-leg pain, and ODI from baseline to the last follow-up were similar in both groups [28].
Another review in 2019 comparing outcomes of redo lumbar discectomy and discectomy with instrumented fusion reported that the clinical outcomes in both groups are comparable; where the limb pain improvements were similar, early postoperative low back pain was worse in the fusion group but significantly better at 1 year after operation [25]. In a more recent systematic review conducted in 2020, which evaluated the surgical management of RDH, the fusion group showed a superior improvement in postoperative VAS-back scores, while the discectomy alone group demonstrated a favorable improvement in postoperative VAS-leg scores [20]. Controversy regarding clinical outcome may be attributed to the heterogeneity of the patient population and the varying surgical techniques used by the different authors.
Regarding the radiological findings, in the revision discectomy alone group, the values of preoperative and postoperative DHI and FHI were more or less similar. After 24 months, the DHI and FHI decreased, however this was not statistically significant (with p-values of 0.338 and 0.881, respectively). In the revision discectomy with fusion group, a significant increase in the postoperative DHI and FHI was observed when compared to the preoperative situation. Moreover, at 24 months, the values remained virtually unchanged.
In contrast, the amount of subsidence after 24 months in the revision discectomy alone group was significantly higher than that in the revision discectomy fusion group.
Consistent with our findings, a previous study by Chen et al. [28] which aimed to evaluate the efficacy of the TLIF technique for patients with RDH reported an increase in post-treatment mean disc height. The post-treatment mean disc height at the herniated level was 91.5%┬▒11% of the level above the fusion, while the preoperative mean disc height at the herniated level was 58.6%┬▒12.3% of the cephalic adjacent level (p<0.001) [28].
In previous studies comparing surgical treatment options for RDH, the amount of disc height subsidence was not well reported. To our knowledge, the current study is the first to compare the amount of subsidence in revision discectomy alone versus revision discectomy with fusion.
Some earlier studies stated that after conventional discectomy, postoperative degenerative changes can occur with time. Gradual disc space subsidence and impingement of the superior facet could lead to foraminal stenosis [23]. The magnitude of subsidence observed in the revision discectomy alone group could consequently increase the probability of segmental instability [2].
In contrast, during revision discectomy with fusion, adequate foraminal decompression can be easily accomplished due to the exposure of the foraminal portion [21].
This finding can be a significant factor in selecting the proper procedure for the treatment of RDH as fusion was demonstrated to prevent segmental instability or reduction of intervertebral space and compression on the nerve root. We could also correlate the greater subsidence observed in the revision discectomy alone group with an inferior clinical outcome.
Although the occurrences of more dural tears, the need for blood transfusions, and postoperative paresthesia were more often in the fusion group, no statistically significant differences could be confirmed between the groups.
There is a controversy between the findings of previous reports and this result. Some authors assumed that both approaches have comparable complication rates. However, other reports observed less complication frequencies in revision discectomy alone [28].
In agreement with our finding, Hlubek and Mundis [3] reported that both repeat lumbar discectomy and instrumented fusion appear to effectively treat patients with similar complication rates.
However, Khayat et al. [24] reported that revision discectomy with fusion showed slightly higher incidence of dural tears without statistical significance, but a significantly greater need for blood transfusions compared to redo-discectomy alone group. On the other hand, Arif et al. [22] reported that redo-discectomy alone led to a lower complication rate (3.2% lower, p>0.05) than redo-discectomy with fusion group.
Nonetheless, revision discectomy with fusion is more expensive than standalone revision discectomy due to the longer duration of the procedure, hospital stay and the superadded implant costs [17].
The confounding factors of this study include the small sample size and short follow-up period, and the surgeries were performed by a single surgeon.
Patients who underwent revision discectomy with fusion exhibited prolonged operation time, greater blood loss, and an extended hospital stay than those who underwent revision discectomy alone; however, they reported a better VAS score for back and leg pains and an improved ODI. Moreover, lower amount of disc height subsidence was observed after 2 years of follow-up with a lesser incidence of segmental instability. Furthermore, there was no significant difference in the complication rate between the two groups. Thus, revision discectomy with fusion is preferable in the management of RDH owing to its ability to alleviate pain, improve disability, and restore the spine stability without significant complications.
Notes
Author Contributions
Conceptualization: all authors. Data curation: all authors. Formal analysis: all authors. Funding acquisition: all authors. Methodology: all authors. Project administration: all authors. Visualization: all authors. WritingŌĆōoriginal draft: all authors. WritingŌĆōreview & editing: all authors. Final approval of the manuscript: all authors.
Fig.┬Ā1
(A, B) Visual Analog Scale (VAS) for back and leg pain in both groups. Preop, preoperative; Postop, postoperative.
Table┬Ā1
The demographic data of the two study groups
Table┬Ā2
The operative data of the two study groups
Table┬Ā3
VAS for back and leg pain of the two study groups
Table┬Ā4
ODI score of the two study groups
Table┬Ā5
Complications in the two study groups
References
2. Dower A, Chatterji R, Swart A, Winder MJ. Surgical management of recurrent lumbar disc herniation and the role of fusion. J Clin Neurosci 2016;23:44ŌĆō50.


3. Hlubek RJ, Mundis GM Jr. Treatment for recurrent lumbar disc herniation. Curr Rev Musculoskelet Med 2017;10:517ŌĆō20.




4. Akar E, Yolcu A, Erdogan B, et al. Recurrent lumbar disc herniation: one clinicŌĆÖs experience. Eurasian J Med Investig 2018;2:18ŌĆō21.
5. Huang W, Han Z, Liu J, Yu L, Yu X. Risk factors for recurrent lumbar disc herniation: a systematic review and meta-analysis. Medicine (Baltimore) 2016;95:e2378.


7. Yaman ME, Kazanc─▒ A, Yaman ND, Bas F, Ayberk G. Factors that influence recurrent lumbar disc herniation. Hong Kong Med J 2017;23:258ŌĆō63.


9. Shimia M, Babaei-Ghazani A, Sadat BE, Habibi B, Habibzadeh A. Risk factors of recurrent lumbar disk herniation. Asian J Neurosurg 2013;8:93ŌĆō6.



10. Kim KT, Park SW, Kim YB. Disc height and segmental motion as risk factors for recurrent lumbar disc herniation. Spine (Phila Pa 1976) 2009;34:2674ŌĆō8.


11. McGirt MJ, Eustacchio S, Varga P, et al. A prospective cohort study of close interval computed tomography and magnetic resonance imaging after primary lumbar discectomy: factors associated with recurrent disc herniation and disc height loss. Spine (Phila Pa 1976) 2009;34:2044ŌĆō51.

12. Awad JN, Moskovich R. Lumbar disc herniations: surgical versus nonsurgical treatment. Clin Orthop Relat Res 2006;443:183ŌĆō97.

13. Greenleaf RM, Harris MB, Bono CM. The role of fusion for recurrent disk herniations. Semin Spine Surg 2011;23:242ŌĆō8.

14. Onyia CU, Menon SK. The debate on most ideal technique for managing recurrent lumbar disc herniation: a short review. Br J Neurosurg 2017;31:701ŌĆō8.


15. Moschetti W, Pearson AM, Abdu WA. Treatment of lumbar disc herniation: an evidence-based review. Semin Spine Surg 2009;21:223ŌĆō9.

16. Guan J, Ravindra VM, Schmidt MH, Dailey AT, Hood RS, Bisson EF. Comparing clinical outcomes of repeat discectomy versus fusion for recurrent disc herniation utilizing the N2QOD. J Neurosurg Spine 2017;26:39ŌĆō44.


17. Selva-Sevilla C, Ferrara P, Geronimo-Pardo M. Cost-utility analysis for recurrent lumbar disc herniation: conservative treatment versus discectomy versus discectomy with fusion. Clin Spine Surg 2019;32:E228ŌĆō34.

18. Mehren C, Wanke-Jellinek L, Korge A. Revision after failed discectomy. Eur Spine J 2020;29(Suppl 1): 14ŌĆō21.


19. Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res 2008;31:165ŌĆō9.


20. Kim GM, Yi CH, Cynn HS. Factors influencing disability due to low back pain using the Oswestry Disability Questionnaire and the Quebec Back Pain Disability Scale. Physiother Res Int 2015;20:16ŌĆō21.



21. Hentenaar B, Spoor AB, de Waal Malefijt J, Diekerhof CH, den Oudsten BL. Clinical and radiological outcome of minimally invasive posterior lumbar interbody fusion in primary versus revision surgery. J Orthop Surg Res 2016;11:2.



22. Arif S, Brady Z, Enchev Y, Peev N. Is fusion the most suitable treatment option for recurrent lumbar disc herniation?: a systematic review. Neurol Res 2020;42:1034ŌĆō42.


23. Awad T, Faisel S. Recurrent lumbar disc herniation: conventional re-discectomy versus TLIF with unilateral fixation. Egypt Spine J 2016;20:18ŌĆō27.

24. Khayat R, Khallaf M, Hassan HM, Gamal M. Evaluation of treatment of recurrent lumbar disc prolapse: fusion versus non fusion. Int Ann Med 2017;1:6ŌĆō12.

25. Tanavalee C, Limthongkul W, Yingsakmongkol W, Luksanapruksa P, Singhatanadgige W. A comparison between repeat discectomy versus fusion for the treatment of recurrent lumbar disc herniation: systematic review and meta-analysis. J Clin Neurosci 2019;66:202ŌĆō8.


26. Drazin D, Ugiliweneza B, Al-Khouja L, et al. Treatment of recurrent disc herniation: a systematic review. Cureus 2016;8:e622.