|
 |
- Search
| Asian Spine J > Volume 17(5); 2023 > Article |
|
Abstract
The purpose of this research was to compare the therapeutic efficacy of multiple-rod constructs vis-a-vis 2-rod constructs in the treatment of adult spinal deformity. A systematic review and meta-analysis were performed to determine whether the multiple-rod construct outperformed the 2-rod construct. We initially retrieved 357 papers, but only 12 were chosen for further meta-analysis. The rod breakage rates in the multiple-rod and the 2-rod groups were 10.66% and 29.87%, respectively. The multiple-rod construct inhibited rod breakage (odds ratio [OR], 0.28; 95% confidence interval [CI], 0.19–0.41; p<0.001), pseudarthrosis (OR, 0.30; 95% CI, 0.18–0.50; p<0.001) and rod fracture at the osteotomy site (OR, 0.34; 95% CI, 0.13–0.89; p=0.03). Furthermore, the multiple-rod construct reduces the risk of revision surgery (OR, 0.38; 95% CI, 0.20–0.73; p=0.04) as well as the revision risk of pseudarthrosis/rod fracture in the multiple-rod group (OR, 0.31; 95% CI, 0.18–0.52; p<0.001), but increases the risk of caudal screw loosening (OR, 4.99; 95% CI, 1.87–13.30; p=0.001). There was no statistically significant difference in proximal junctional kyphosis (PJK) parameters (p=0.85), cerebrospinal fluid leakage (p=0.09), wound infection (p=0.71), age at surgery (p=0.62), gender distribution (p=0.93), body mass index (p=0.86), smoking status (p=0.05), hospital stay (p=0.09), osteoporosis (p=0.95), CoCr rod material (p=0.15), bone morphogenetic protein-2 (p=0.58), L5/S1 interbody fusion (p=0.07), high-grade osteotomies (p=0.07), the number of fusion levels (p=0.11), operation time (p=0.30), and blood loss volume (p=0.34). Regarding radiographic parameters, only preoperative sagittal vertical axis was found to be higher (weight means difference [WMD], 25.60; 95% CI, 15.43–35.77; p<0.001) in the multiple-rod group. There was no difference in preoperative Oswestry Disability Index (ODI) (WMD, −3.32; 95% CI, −7.38 to 0.73; p=0.11), but the multiple-rod group had a lower ODI at follow-up (WMD, −7.71; 95% CI, −11.62 to −3.86; p<0.001). Multiple-rod constructs could prevent rod breakage and pseudarthrosis while also lowering the revision rate, resulting in a better clinical outcome than the 2-rod construct. Nonetheless, due consideration should be given to PJK and screw loosening in multiple-rod constructs, possibly due to the increased stiffness caused by the multiple-rod structure.
An aging population is accompanied by a high prevalence of adult spinal deformity (ASD), which is known to adversely affect health-related quality of life (HRQoL). In the United States, it is estimated that the rate of ASD is 32%–68% in people over 65 years old and that, by 2050, more than 60 million elderly people will have ASD [1]. Similarly, the number of ASD patients who chose surgical treatment has more than doubled in the last decade [2]. For severe ASD cases, a correction surgery is recommended for the reconstruction of spinopelvic alignments, which is highly associated with HRQoL [3,4]. To achieve optimal alignment, long constructs are always extended to the pelvis [5], and three-column osteotomies may also be performed [6]. In ASD patients with severe coronal malalignment, an asymmetrical pedicle subtraction osteotomy (PSO) could be an effective way to achieve optimal correction in the sagittal and coronal planes [7]. However, complications from the aforementioned surgical procedures, such as rod fracture [8,9], pseudarthrosis [10,11], and proximal junctional kyphosis (PJK) [12], should be taken seriously.
Pseudarthrosis is known to have been linked to the three-column osteotomy site or the lumbosacral junction region. According to Marques et al. [13], 65 of 524 individuals (12.4%) were diagnosed with pseudarthrosis, and 53 of those diagnosed underwent reoperation. Notably, 88% of pseudarthrosis cases are associated with fusion length (odds ratio [OR], 1.17; p=0.004), osteotomy (OR, 0.28; p=0.025), and pelvic fixation (OR, 0.34; p=0.026) [13]. Pseudarthrosis has been linked to decreased HRQoL, correction loss, rod fracture, and increased revision rates [14]. It has been reported that rod fracture and pseudarthrosis are the most common indications for revision surgery requirements in ASD patients [15]. Yamato et al. [16] reported an 18% rod breakage rate in 304 ASD patients and a 66.7% revision surgery rate in rod fracture patients. Furthermore, Martin et al. [17] reported that 62.5% of revision surgeries were due to mechanical complications or pseudarthrosis for the lumbar fusion surgery. Rod fracture may occur as a result of the increased biomechanical load caused by pseudarthrosis. Given the higher revision rate and poor HRQoL, a variety of techniques, including performing an interbody fusion in the osteotomy region, upsizing pedicle screw instrumentation, using bone morphogenetic protein (BMP)-2, and using teriparatide, have been tried to prevent rod fracture and pseudarthrosis [14].
Rod breakage is usually caused by insufficient rigidity of the construct before bony fusion. Hence, reinforcing the rod construct could prevent rod fracture, which could be achieved by a multiple-rod construct, providing greater instrumentation rigidity. Multiple-rod constructs, such as the accessory rod, satellite rod, and kickstand rod, have thus been used to reduce this complication and achieve greater biomechanical stability and resilience to implant fatigue. However, excessive stiffness associated with the constructs may result in other complications, such as PJK [18]. Therefore, several studies have been conducted to determine whether multiple-rod constructs have any advantages over the 2-rod construct. However, different studies’ findings provided different interpretations. Rabinovich et al. [19] reported a significantly higher rate of rod fracture (21%) in patients who received the 2-rod construct than those who received the multiple-rod construct (5.8%). The multiple-rod construct was found to be extremely resistant to rod breakage (OR, 0.231). Similarly, Lamas et al. [20] reported that 33 out of 58 patients in the 2-rod construct group suffered from rod fractures during the follow-up period (averaging around 26.9 months), whereas no rod breakage was observed in the multiple-rod construct group. However, according to Bourghli et al. [21], multiple-rod constructs spanning the PSO region did not affect the incidence or type of mechanical complications. On the other hand, the multiple-rod construct may result in excessive stiffness, which may increase the likelihood of PJK and screw loosening [22]. Furthermore, the auxiliary rod fixing procedure will undoubtedly lengthen the operation, potentially leading to increased blood loss and other perioperative complications.
A lack of evidence so far has hampered efforts to establish the necessity of routine multiple-rod fixation. Therefore, we attempted to conduct a systematic search for relevant documents and a comprehensive meta-analysis to determine whether multiple-rod constructs had any discernible advantage over the 2-rod construct in the ASD-affected population.
We systematically searched the PubMed, Embase, Cochrane library, and Web of Science databases for studies examining whether multiple-rod constructs had any advantage over 2-rod constructs in adults with spinal deformities on September 10, 2022. The following was the search strategy: (multi-rod or multi-rods or 2-rod or 3-rod or 4-rod or satellite or accessory or auxiliary or kickstand) and ASD.
The inclusion criteria were as follows: (1) the case-control design or cohort study was focused on ASD patients; (2) the number of fusion segments was >5; (3) the 3-rod or 4-rod or satellite or accessory or auxiliary or kickstand was fixed; and (4) the literature was in English. Two authors independently read each abstract (or the full article) to select the eligible papers. Disagreements were settled through discussion within the study group. The current study followed the standard Preferred Reporting Items for Systematic reviews and Meta-Analyses Protocol [23].
The following details were extracted from the papers that met the inclusion criteria: (1) the first author’s name, publication year, study design, and follow-up period; (2) surgical age, gender distribution, body mass index (BMI), osteoporosis, CoCr rod material, BMP-2, L5/S1 interbody fusion, high-grade osteotomies, PJK, number of fusion levels, operation time, blood loss volume, pseudarthrosis, rod breakage, screw loosening, revision surgery, and reoperation for pseudarthrosis/rod fracture; (3) preoperative and postoperative radiographic parameters, including thoracic kyphosis (TK), lumbar lordosis (LL), pelvic tilt (PT), pelvic incidence (PI), pelvic incidence minus lumbar lordosis (PI–LL), and sagittal vertical axis (SVA); and (4) Oswestry Disability Index (ODI) scores before and after surgery.
By eliminating papers successively, a sensitivity analysis was performed to determine whether there was a single paper that significantly affected the pooled results.
For binary variables, the OR with a 95% confidence interval (95% CI), was calculated to determine whether the multiple-rod constructs outperformed the 2-rod construct post-ASD surgery. The weight means difference (WMD) was calculated to describe the difference between the groups’ continuous variables. A p<0.05 was chosen as the threshold for statistical significance. The random effect model was used for the pooled statistics when I2≥50% and the fixed effect model was used otherwise. The statistical analyses were conducted using the Review Manager (RevMan) ver. 5.3 software (The Cochrane Collaboration, London, UK).
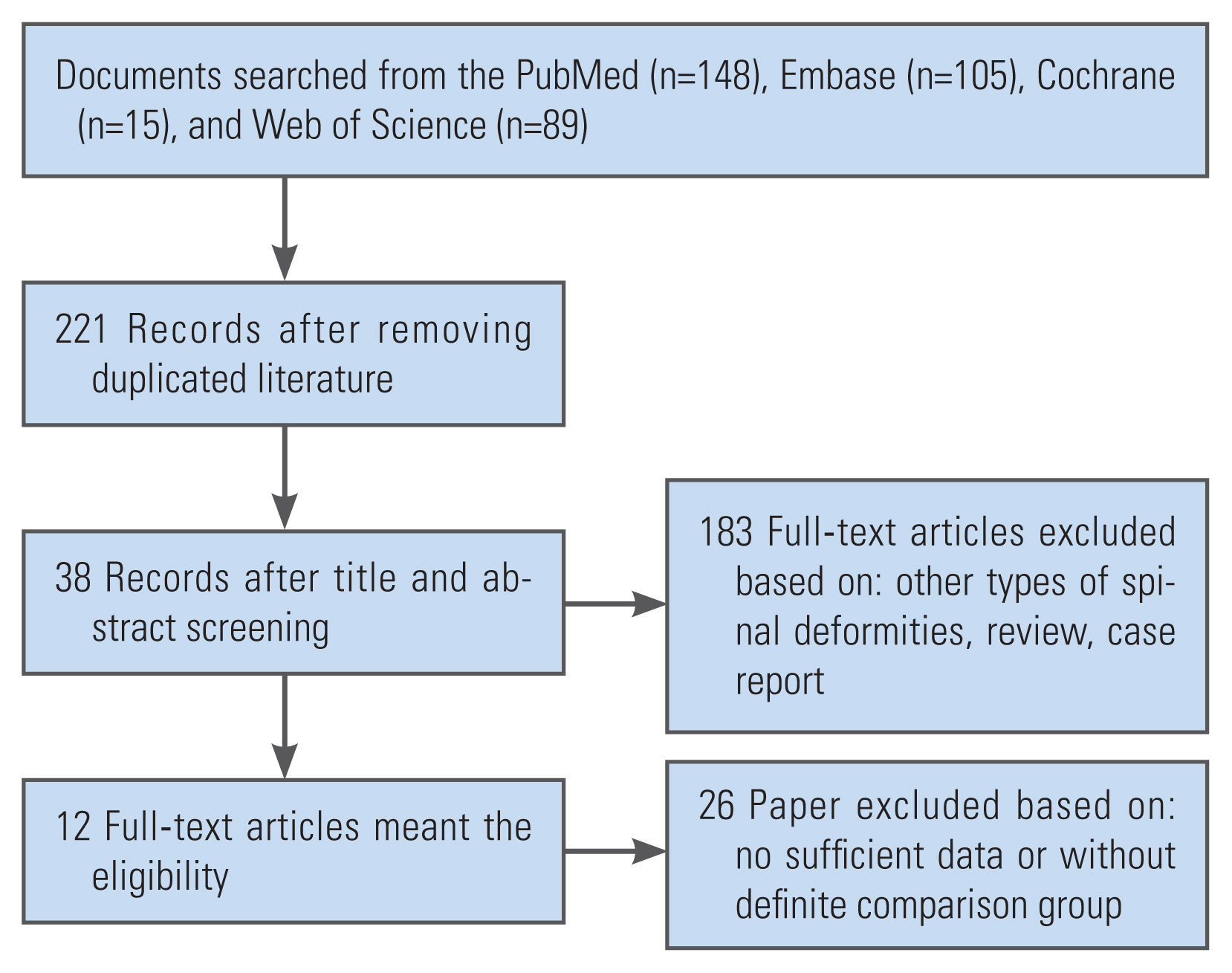
Initially, we retrieved 357 papers from the documents mined from PubMed (n=148), Embase (n=105), Cochrane (n=15), and Web of Science (n=89). After removing duplicate studies, 12 papers met the inclusion criteria [8,10,16,18–22,24–27]. The flow chart in Fig. 1 depicts the selection-elimination process. Long accessory rods were frequently extended to the sacrum or pelvis [8,16,19,20,22,24,25]. The meta-analysis included a total of 830 ASD cases (multiple-rod: n=381, 2-rod: n=449). The rod breakage rate in the multiple-rod group was 10.66% and rose to 29.87% in the 2-rod group. This study used the Newcastle-Ottawa quality assessment scale to evaluate each included paper (Table 1).
There was no substantial difference between groups in terms of age at surgery (p=0.62), gender distribution (p=0.93), BMI (p=0.86), smoking status (p=0.05), hospital stay duration (p=0.09), osteoporosis (p=0.95), CoCr rod material (p=0.15), use of BMP-2 (p=0.58), L5/S1 interbody fusion (p=0.07), high-grade osteotomies (p=0.07), number of fusion levels (p=0.11), operation time (p=0.30), and blood loss volume (p=0.34) (Table 2).
Preoperatively, only SVA was greater (WMD, 25.60; 95% CI, 15.43–35.77; p<0.001) in the multiple-rod group. However, there was no substantial difference in the TK (p=0.59), LL (p=0.37), PT (p=0.94), PI–LL (p=0.14), PI (p=0.84), and TPA (p=0.86). Postoperatively, there was no substantial difference in TK (p=0.87), LL (p=0.23), PT (p=0.12), PI–LL (p=0.82), and SVA (p=0.11). At the final follow-up as well, there was no substantial difference in the preceding radiographic parameters (Table 3).
This meta-analysis found no significance in terms of whole complications (p=0.08), while the multiple-rod construct could noticeably inhibit rod breakage (OR, 0.28; 95% CI, 0.19–0.41; p<0.001) (Fig. 2) and pseudarthrosis (OR, 0.30; 95% CI, 0.18–0.50; p<0.001). The multiple-rod construct could also lower the risk of pseudoarthrosis/rod fracture at the osteotomy site (OR, 0.34; 95% CI, 0.13–0.89; p=0.03), though the risk of caudal screw loosening increased in the multiple-rod construct group (OR, 4.99; 95% CI, 1.87–13.30; p=0.001). No variation was found in terms of PJK (p=0.85) (Fig. 3), cerebrospinal fluid leakage (p=0.09), and wound infection (p=0.71). Furthermore, the pooled results found a lower revision risk (OR, 0.38; 95% CI, 0.20–0.73; p=0.04) and a lower revision risk of pseudarthrosis/rod fracture in the multiple-rod group (OR, 0.31; 95% CI, 0.18–0.52; p<0.001) (Table 4).
Intuitively, multiple-rod constructs would denote an additional operative procedure, which inevitably increases the operation time and blood loss. This study, however, found no statistical difference (p=0.30) in operation time between both groups. Correspondingly, other factors linked to operation time, including age at surgery, fusion levels, BMI, high-grade osteotomies, and preoperative radiographic parameters, were also comparable among the groups. Previously, numerous studies have also found similar findings [16,19,24]. Regarding blood loss, Yamato et al. [16] and Merrill et al. [18] found no significant difference in the case of blood loss volume. This research, similarly, found no distinction in the volume of blood loss. Therefore, the surgical procedures to install the auxiliary rods may not have a significant effect on the amount of blood loss or the operation time, not as intuition may suggest.
The main purpose of the multiple-rod construct is to prevent possible mechanical failures in ASD individuals when long-segment spinal fixations or three-column osteotomies are conducted. This meta-analysis revealed that the rod breakage rate was 9.35% in the multiple-rod group, but this figure rose to 31.09% in the 2-rod group. The rod fracture usually occurs at the three-column osteotomy site and lumbosacral segment, where the multiple-rod structure could markedly bring down the risk of rod fracture at the osteotomy site [8]. However, the rod fracture above or below the osteotomy site could be considered in the multiple-rod group [27]. We could observe that the multiple-rod constructs had a higher potential to prevent rod breakage (OR, 0.28; p<0.001) and pseudarthrosis (OR, 0.30; p<0.001), than the 2-rod construct, which was consistent with the previous results [19,28]. Furthermore, the pooled results found a lower revision risk in the multiple-rod group (OR, 0. 38; 95% CI, 0.20–0.73; p=0.04) and a lower revision risk of pseudarthrosis/rod fracture in the multiple-rod group (OR, 0.31; 95% CI, 0.18–0.52; p<0.001). Therefore, the multiple-rod structure could lower the risk of rod fracture and also lower the risk of revision surgery [16,24,25].
However, it is noteworthy that the multiple-rod construct method was simply one of the strategies to resolve the mechanical failure. A series of complicated factors were linked to rod fractures, including anterior column support, pelvic fixation, and the use of BMP-2. Most studies included in this study reported cases of pelvic fixation, and most of them used interbody fusion at L5/S1 to lower the stress of the rod [8,16,25]. Rabinovich et al. [19] also conducted transforaminal lumbar interbody fusion procedures at L3–4 and L4–5. Anterior lumbar interbody fusion (ALIF) was also employed with multiple-rod constructs [24]. The cage used by ALIF and oblique lumbar interbody fusion has a higher contact area with the vertebrae, which could better reduce rod stress theoretically. Furthermore, in long spinal constructs, reinforcement at the three-column osteotomy site causes a stress concentration in the adjacent segments. Interbody fusion was also tried to reduce the rod stress adjacent to the PSO site [10]. Under such a scenario, the rod fracture rate at the lumbosacral junctional region might aggravate in patients with additional short rods [16]. It was suggested that the long rods should span L5/S1 segments when it is unavoidable to use the long auxiliary rods. Additionally, it was found that the use of BMP-2 could avoid rod fracture [10]. Safaee et al. [29] revealed that the use of BMP lowered the rates of revision surgery due to pseudarthrosis.
It has been determined that sagittal spinal alignment was highly linked to HRQoL. This meta-analysis did not reveal any difference in sagittal spinal radiographic parameters immediately after surgery and at the final follow-up. Hence, it could be postulated that both the multiple-rod constructs and the 2-rod constructs could reconstruct the sagittal spinal alignment effectively. Furthermore, the correction could be sustained during the follow-up. Similar results were also reported by several studies [8,16,18]. Although every multiple-rod construct could give more strength to the whole construct, there are still variations in the various types of multiple-rod constructs. For instance, the “kickstand rod” technique could correct the coronal imbalance effectively [30], whereas the short additional rod construct might have a less significant effect on whole spine alignment [16].
Although the multiple-rod constructs could increase the stability at the three-column osteotomy site and the L5/S1 segment, the increased stiffness of the whole construct could not be prevented. Therefore, an abruptly heightened stiffness is introduced from the flexible segments to the fixed segments in the multiple-rod constructs, entailing a higher rate of PJK [31]. It is prevalently accepted that PJK has a negative effect on the quality of life [12,32]. Multiple studies have assessed this issue in ASD patients who received multiple-rod constructs. Han et al. [22] found a higher PJK rate in the CoCr multiple-rod group than the Ti 2-rod group, which supported the argument of increasing rod stiffness accompanying a higher rate of PJK in ASD surgery. However, our meta-analysis did not discover a significant difference in the prevalence of PJK between these groups, which was consistent with several other reports [19,24,25,27]. Given the small sample size and short follow-up time in previous studies, it could come short of reflecting the true effect of increased stiffness on PJK. Overall, measures such as ligament strengthening, vertebrae augmentation, and osteoporosis treatment are suggested to prevent PJK [12,33].
Furthermore, multiple-rod constructs could also increase the pull-out stress on the caudal screws. This meta-analysis could demonstrate that the caudal screw loosening frequently occurred in the multiple-rod construct group (OR, 4.99; 95% CI, 1.87–13.30; p=0.001). Previously, Banno et al. [8] also found that the multiple-rod construct elevated the risk of iliac screw loosening. To resolve this issue, a series of surgical strategies were suggested to prevent screws from loosening. For example, Ebata et al. [34] found that bilateral dual iliac screws could markedly reduce the loosening rate than the common bilateral single iliac screw (9% versus 61%, p<0.001). For osteoporosis patients, cement-augmented iliac screws could be an optimal method to reduce the loosening rate [35]. Furthermore, effective anti-osteoporotic therapy could also decrease the aforementioned internal fixation-related complications [36].
The main purpose of ASD surgery is to relieve symptoms and improve the quality of life rather than simply correcting deformities. Consequently, several studies have evaluated whether the multiple-rod constructs had any advantage over the 2-rod construct in terms of HRQoL. Multiple scales could be used to assess the clinical outcome after ASD surgery [25], out of which the ODI index is the most widely used. Yamato et al. [16] reported an enhanced ODI value in the multiple-rod construct. However, Lamas et al. [20] and Banno et al. [8] did not find any significant difference in the ODI value between groups. Bourghli et al. [21] reported the ODI, Scoliosis Research Society-22 questionnaire, and 36-item Short Form Health Survey scores and found better HRQoL values in the multiple-rod construct group at 6 months and 2 years follow-up. This meta-analysis discovered no appreciable difference in the preoperative ODI score (p=0.11), but we found an improved ODI score during the final follow-up (p=0.002) in the multiple-rod group. Hence, we could assert that multiple-rod constructs could enhance life quality in the follow-up period.
Although the current meta-analysis systematically retrieved papers revolving around multiple-rod constructs in ASD surgery, the following defects should not be overlooked while referring to the pooled results. Firstly, there is a plethora of multiple-rod constructs with multiple biomechanical properties [37]. Subgroup analyses could not be conducted by different multiple-rod constructs due to insufficient eligible studies. It is hard to directly evaluate just one construct as the most suitable multiple-rod construct, but further biomechanical studies may be valuable in determining the ideal multiple-rod construct. Secondly, the small sample sizes for the included literature may cause a higher heterogeneity while pooling the findings. Thirdly, only retrospective research was reported, and thus, prospective studies were needed to assess whether the multiple-rod construct outperformed the 2-rod construct. Fourthly, the current meta-analysis could not conduct the subgroup analysis based on three-column osteotomy (PSO/vertebral column resection) and long-segment pelvic fixation.
The multiple-rod constructs could avoid rod breakage and pseudoarthrosis, reduce the revision rate, and thus achieve a better clinical outcome vis-a-vis the 2-rod construct. However, due attention is needed in PJK and screw loosening induced by the multiple-rod structure-induced stiffness.
Notes
Author Contributions
Dongfa Liao and Da Liu designed this study. Jian Zhao and Zhengping Zhang searched the literatures. The selection process was performed by Da Liu and Jian Zhao. The data collection was performed by Jian Zhao, Zheng Nie, and Zhengping Zhang. Data analysis was performed by Jian Zhao, and Zhengping Zhang. Jian Zhao and Dongfa Liao wrote the manuscript with the help from the rest of authors.
Fig. 2
The forest plot demonstrated that the multiple-rod construct could prevent rod breakage. M–H, Mantel-Haenszel; CI, confidence interval; df, degrees of freedom.
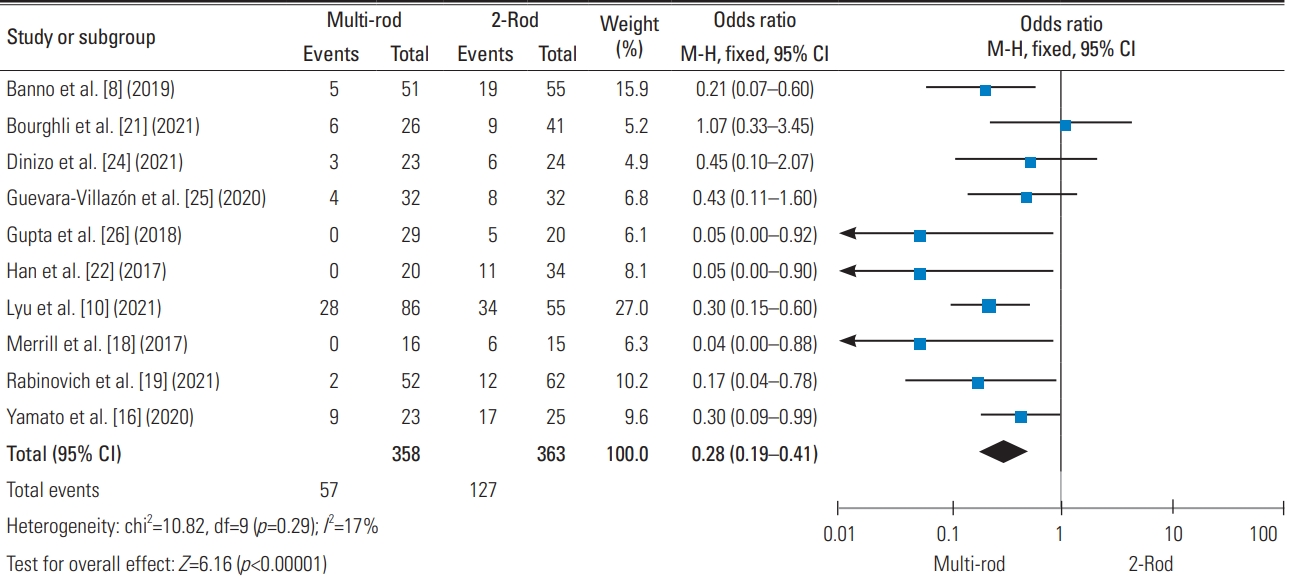
Fig. 3
The forest plot demonstrated no difference between the multiple-rod constructs group and 2-rod group in terms of the occurrence of proximal junctional kyphosis (PJK). M–H, Mantel-Haenszel; CI, confidence interval; df, degrees of freedom.

Fig. 4
The funnel plot was symmetrical, which implied a lower publication bias. SE, standard error; OR, odds ratio.
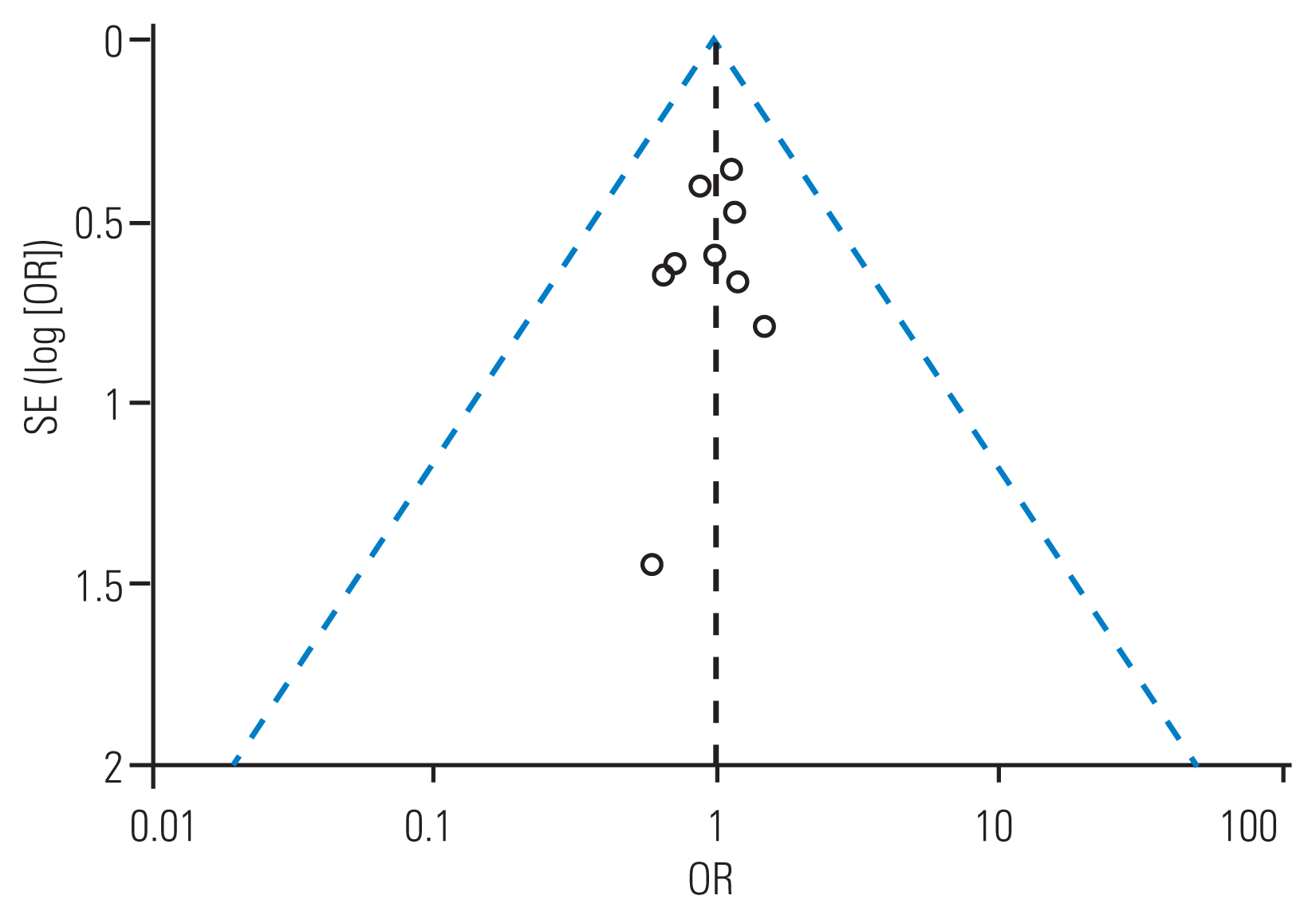
Table 1
The basic information of the included research literature
| Study | Year | Sample | Age (yr) | Follow-up | Study design | NOQAS | ||
|---|---|---|---|---|---|---|---|---|
| Multi-rod | 2-Rod | Total | ||||||
| Lamas et al. [20] | 2021 | 39 | 58 | 97 | Multi-rod: 66.2±7.7; 2-rod: 61.7±9.0 | Multi-rod: 3.1 yr (2.0–5.4 yr); 2-rod: 4.1 yr (2.01–7.5 yr) | Retrospective | 8 |
| Lyu et al. [10] | 2021 | 86 | 55 | 141 | 65.2±10.1 | 33.8±20.2 mo | Retrospective | 8 |
| Bourghli et al. [21] | 2021 | 41 | 26 | 67 | Multi-rod: 59.8±14, 61.5±9; 2-rod: 58.9±13 | Multi-rod: 31±6 mo; 33±7 mo; 2-rod: 30±6 mo | Retrospective | 8 |
| Rabinovich et al. [19] | 2021 | 52 | 62 | 114 | Multi-rod: 68.2±6.3; 2-rod: 67.7±8.4 | Multi-rod: 34.9±9.4 mo; 2-rod: 38.4±11.0 mo | Retrospective | 8 |
| Dinizo et al. [24] | 2021 | 23 | 24 | 47 | Multi-rod: 62±11; 2-rod: 60±11.4 | 2-year follow up | Retrospective | 8 |
| Yamato et al. [16] | 2020 | 23 | 25 | 48 | Case: 66.2±10.2; control: 68.9±8.3 | Additional-rod: 33.5±6.5 mo; 2-rod: 68.9±8.3 mo | Retrospective | 8 |
| Guevara-Villazón et al. [25] | 2020 | 32 | 32 | 64 | Multi-rod: 68.76; 2-rod: 71.94 | Minimum 1-year follow-up | Retrospective | 8 |
| Banno et al. [8] | 2019 | 51 | 55 | 106 | Multi-rod: 67.6±8.9; 2-rod: 68.8±10.2 | 42 mo (13–83 mo) | Retrospective | 8 |
| Gupta et al. [26] | 2018 | 18 | 52 | 70 | Multi-rod: 62; 2-rod: 64 | Minimum 1-year follow-up | Retrospective | 8 |
| Merrill et al. [18] | 2017 | 16 | 15 | 31 | Multi-rod: 63±12; 2-rod: 68±9 | Multi-rod: 36.34±16.87 mo; 2-rod: 28.73±7.98 mo | Retrospective | 8 |
| Han et al. [22] | 2017 | 20 | 34 | 54 | Multi-rod: 67.7 (55–77); 2-rod: 64.8 (50–77) | Multi-rod: 14±3.3 mo; 2-rod: 56.4±39.8 mo | Retrospective | 8 |
| Hyun et al. [27] | 2014 | 66 | 66 | 132 | Multi-rod: 48.5±16.0; 2-rod: 49.4±22.4 | Multi-rod: 7±4 yr; 2-rod: 6.5±2.9 yr | Retrospective | 8 |
Table 2
The pooled results between the multiple-rod group and 2-rod group
Table 3
The pooled results between the multiple-rod group and 2-rod group
Table 4
Comparison of the complications between the multiple-rod group and 2-rod group
References
1. Ames CP, Scheer JK, Lafage V, et al. Adult spinal deformity: epidemiology, health impact, evaluation, and management. Spine Deform 2016 4:310–22.


2. Pellise F, Vila-Casademunt A, Ferrer M, et al. Impact on health related quality of life of adult spinal deformity (ASD) compared with other chronic conditions. Eur Spine J 2015 24:3–11.



3. Arima H, Hasegawa T, Yamato Y, et al. Factors associated with improved quality of life outcomes in patients undergoing surgery for adult spinal deformity. Spine (Phila Pa 1976) 2021 46:E384–91.


4. Kim HJ, Yang JH, Chang DG, et al. Adult spinal deformity: current concepts and decision-making strategies for management. Asian Spine J 2020 14:886–97.




5. Silva FE, Lenke LG. Adult degenerative scoliosis: evaluation and management. Neurosurg Focus 2010 28:E1.

6. Doodkorte RJ, Vercoulen TF, Roth AK, de Bie RA, Willems PC. Instrumentation techniques to prevent proximal junctional kyphosis and proximal junctional failure in adult spinal deformity correction: a systematic review of biomechanical studies. Spine J 2021 21:842–54.


7. Lau D, Haddad AF, Deviren V, Ames CP. Asymmetrical pedicle subtraction osteotomy for correction of concurrent sagittal-coronal imbalance in adult spinal deformity: a comparative analysis. J Neurosurg Spine 2020 33:822–9.


8. Banno T, Hasegawa T, Yamato Y, et al. Multi-rod constructs can increase the incidence of iliac screw loosening after surgery for adult spinal deformity. Asian Spine J 2019 13:500–10.




9. Noh SH, Kim KH, Park JY, et al. Characteristics and risk factors of rod fracture following adult spinal deformity surgery: a systematic review and meta-analysis. Neurospine 2021 18:447–54.




10. Lyu Q, Lau D, Haddad AF, Deviren V, Ames CP. Multiple-rod constructs and use of bone morphogenetic protein-2 in relation to lower rod fracture rates in 141 patients with adult spinal deformity who underwent lumbar pedicle subtraction osteotomy. J Neurosurg Spine 2021 Sep 24 [Epub]. https://doi.org/10.3171/2021.3.SPINE201968

11. How NE, Street JT, Dvorak MF, et al. Pseudarthrosis in adult and pediatric spinal deformity surgery: a systematic review of the literature and meta-analysis of incidence, characteristics, and risk factors. Neurosurg Rev 2019 42:319–36.



12. Zhao J, Chen K, Zhai X, Chen K, Li M, Lu Y. Incidence and risk factors of proximal junctional kyphosis after internal fixation for adult spinal deformity: a systematic evaluation and meta-analysis. Neurosurg Rev 2021 44:855–66.



13. Marques MF, Fiere V, Obeid I, et al. Pseudarthrosis in adult spine deformity surgery: risk factors and treatment options. Eur Spine J 2021 30:3225–32.



14. Penalosa BS, Ramos O, Patel SS, Cheng WK, Danisa OA. Pedicle subtraction osteotomy in adult spinal deformity correction: clinical and radiographic risk factors for early instrumentation failure. J Clin Neurosci 2021 94:266–70.


15. Smith JS, Shaffrey CI, Klineberg E, et al. Complication rates associated with 3-column osteotomy in 82 adult spinal deformity patients: retrospective review of a prospectively collected multicenter consecutive series with 2-year follow-up. J Neurosurg Spine 2017 27:444–57.


16. Yamato Y, Hasegawa T, Togawa D, et al. Long additional rod constructs can reduce the incidence of rod fractures following 3-column osteotomy with pelvic fixation in short term. Spine Deform 2020 8:481–90.



17. Martin BI, Mirza SK, Comstock BA, Gray DT, Kreuter W, Deyo RA. Reoperation rates following lumbar spine surgery and the influence of spinal fusion procedures. Spine (Phila Pa 1976) 2007 32:382–7.


18. Merrill RK, Kim JS, Leven DM, Kim JH, Cho SK. Multi-rod constructs can prevent rod breakage and pseudarthrosis at the lumbosacral junction in adult spinal deformity. Global Spine J 2017 7:514–20.




19. Rabinovich EP, Buell TJ, Wang TR, Shaffrey CI, Smith JS. Reduced occurrence of primary rod fracture after adult spinal deformity surgery with accessory supplemental rods: retrospective analysis of 114 patients with minimum 2-year follow-up. J Neurosurg Spine 2021 35:504–15.


20. Lamas V, Charles YP, Tuzin N, Steib JP. Comparison of degenerative lumbar scoliosis correction and risk for mechanical failure using posterior 2-rod instrumentation versus 4-rod instrumentation and interbody fusion. Eur Spine J 2021 30:1965–77.



21. Bourghli A, Boissiere L, Kieser D, et al. Multiple-rod constructs do not reduce pseudarthrosis and rod fracture after pedicle subtraction osteotomy for adult spinal deformity correction but improve quality of life. Neurospine 2021 18:816–23.




22. Han S, Hyun SJ, Kim KJ, Jahng TA, Lee S, Rhim SC. Rod stiffness as a risk factor of proximal junctional kyphosis after adult spinal deformity surgery: comparative study between cobalt chrome multiple-rod constructs and titanium alloy two-rod constructs. Spine J 2017 17:962–8.


23. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021 372:n71.



24. Dinizo M, Passias P, Kebaish K, Errico TJ, Raman T. The approach to pseudarthrosis after adult spinal deformity surgery: is a multiple-rod construct necessary? Global Spine J 2023 13:636–42.




25. Guevara-Villazon F, Boissiere L, Hayashi K, et al. Multiple-rod constructs in adult spinal deformity surgery for pelvic-fixated long instrumentations: an integral matched cohort analysis. Eur Spine J 2020 29:886–95.



26. Gupta S, Eksi MS, Ames CP, et al. A novel 4-rod technique offers potential to reduce rod breakage and pseudarthrosis in pedicle subtraction osteotomies for adult spinal deformity correction. Oper Neurosurg (Hagerstown) 2018 14:449–56.




27. Hyun SJ, Lenke LG, Kim YC, Koester LA, Blanke KM. Comparison of standard 2-rod constructs to multiple-rod constructs for fixation across 3-column spinal osteotomies. Spine (Phila Pa 1976) 2014 39:1899–904.


28. Yu BS, Yang ZK, Li ZM, Zeng LW, Wang LB, Lu WW. Which is the preferred revision technique for loosened iliac screw?: a novel technique of boring cement injection from the outer cortical shell. J Spinal Disord Tech 2011 24:E49–56.

29. Safaee MM, Dalle Ore CL, Zygourakis CC, Deviren V, Ames CP. Estimating a price point for cost-benefit of bone morphogenetic protein in pseudarthrosis prevention for adult spinal deformity surgery. J Neurosurg Spine 2019 30:814–21.

30. Makhni MC, Zhang Y, Park PJ, et al. The “kickstand rod” technique for correction of coronal imbalance in patients with adult spinal deformity: initial case series. J Neurosurg Spine 2019 32:415–22.

31. Thawrani DP, Glos DL, Coombs MT, Bylski-Austrow DI, Sturm PF. Transverse process hooks at upper instrumented vertebra provide more gradual motion transition than pedicle screws. Spine (Phila Pa 1976) 2014 39:E826–32.


32. Kim HJ, Yang JH, Chang DG, et al. Proximal junctional kyphosis in adult spinal deformity: definition, classification, risk factors, and prevention strategies. Asian Spine J 2022 16:440–50.




33. Gupta A, Cha T, Schwab J, et al. Osteoporosis increases the likelihood of revision surgery following a long spinal fusion for adult spinal deformity. Spine J 2021 21:134–40.


34. Ebata S, Oba H, Ohba T, et al. Surgical outcomes of long fusion using dual iliac screws bilaterally for adult spinal deformities: the effect on the loosening rate and sacroiliac joint correction. Spine Surg Relat Res 2019 3:236–43.



35. Oberkircher L, Masaeli A, Hack J, et al. Pull-out strength evaluation of cement augmented iliac screws in osteoporotic spino-pelvic fixation. Orthop Traumatol Surg Res 2021 107:102945.


- TOOLS
-
METRICS

-
- 0 Crossref
- Scopus
- 1,415 View
- 165 Download
- Related articles in ASJ
-
Endoscopic Anterior Lumbar Interbody Fusion: Systematic Review and Meta-Analysis2023 December;17(6)