Introduction
Lumbar spinal fusion is a popular treatment for instability associated with neurological compression and/or spinal deformity [
1], and there have been significant advances in the approach, techniques, and implants used. Anterior and lateral methods (anterior lumbar interbody fusion, oblique lumbar interbody fusion, and extreme lateral interbody fusion) are available depending on the problematic level. Several posterior approaches, including posterolateral fusion (PLF), posterolateral lumbar interbody fusion (PLIF), and transforaminal lumbar interbody fusion (TLIF), have also been described. The advent of percutaneous screws led to the concept of minimally invasive approaches designed to reduce blood loss, pain, and length of stay; nevertheless, these techniques may be accompanied by increased intraoperative radiation exposure and a steep learning curve [
1,
2].
There is considerable debate in the literature regarding the best lumbar spinal fusion approach, and multiple studies and meta-analyses have compared various outcomes for these procedures. However, the heterogeneity of data and recording techniques makes it difficult to draw definitive conclusions. This large single-center retrospective study aimed to assess the perioperative and intermediate-term clinical outcomes of patients with various lumbar fusion techniques at our institution (Salford Royal Hospital, Northern Care Alliance NHS foundation trust). We present perioperative and patient-reported outcome data from consecutive patients who underwent one- or two-level lumbar fusion using either a minimally invasive or open approach with or without interbody cage placement. As a result, this is one of the largest studies comparing different posterior lumbar fusion techniques.
Materials and Methods
1. Patient population
Patient self-reported outcomes were prospectively collected and retrospectively analyzed for patients undergoing one- or two-level lumbar spinal fusion at our institution between January 2011 and December 2018. Demographic data (age, gender, and body mass index [BMI]) for each patient were collected in addition to predominant pre-surgery symptoms (back pain, leg pain/sciatica, and sensory symptoms/motor deficit), surgical indication (e.g., spondylolisthesis, recurrent disc disease, foraminal stenosis, and scoliosis), previous operative history, perioperative outcomes and complications (i.e., post-surgery stay and intraoperative dural tear), and whether later revision surgery was required.
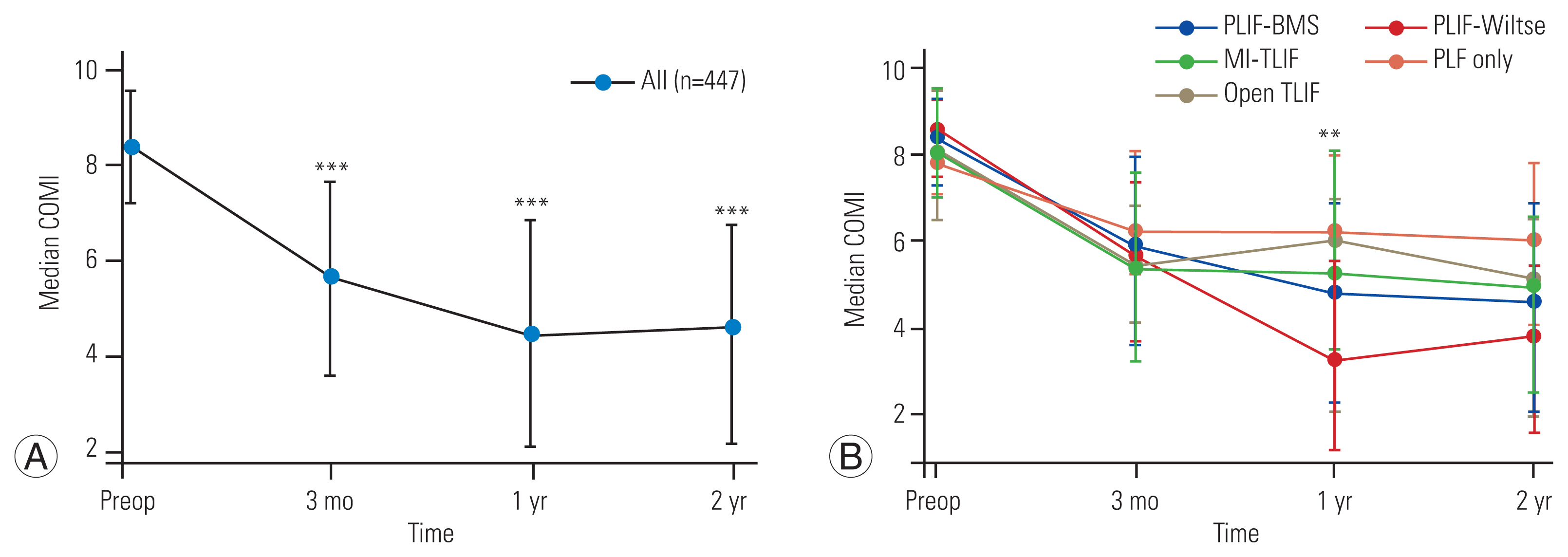
Core outcomes measure index (COMI) questionnaires were used to determine patient self-reported outcome measures. Previous studies have validated the use of COMI questionnaires as a patient-recorded outcome measure, and COMI is the official outcome instrument of the prospectively collected
Eurospine Spine Tango database [
3,
4]. COMI questionnaires were given to patients pre-surgery and at 3 months, 1 year, and 2 years post-surgery. Data were prospectively collected onto the Spine Tango registry by employed clerks independent of the surgical team and were then retrospectively analyzed. The institutional review board at Salford Royal Hospital approved the study, and the requirement for informed consent was waived. The analysis was performed in accordance with the 1964 Helsinki Declaration and its amendments.
2. Surgical procedures
During the study period, our institution used five different lumbar spinal fusion techniques: PLF only, PLIF performed using bilateral muscle strip (PLIF-BMS) or Wiltse approach (PLIF-Wiltse), open TLIF, and minimally invasive TLIF (MI-TLIF).
Cases categorized as PLF underwent pedicle screw instrumentation and fusion using autograft and allograft in the intertransverse plane after decorticating the transverse processes. In PLIF cases, screw instrumentation was also used, and the disc space was accessed by removing bilateral facet joints and inserting bilateral cages packed with autograft and allograft mixture. PLIF cases were subcategorized based on whether the pedicle screws were introduced by a Wiltse approach, followed by smaller midline laminotomy for decompression and cage insertion or traditional bilateral muscle strips from the midline. In most cases, the spinous process, interspinous, and supraspinous ligaments were left intact to retain the posterior tension band. Cases were categorized as TLIF if the access to the disc space was via a single-sided facet joint resection, and fusion was achieved using a single cage through a transforaminal approach. TLIFs were subcategorized based on whether the pedicle screws were inserted via stab incisions (MI-TLIF) or using two paramedian incisions and the Wiltse approach (open TLIF). Facetectomy was performed in MI-TLIF patients via a separate small paramedian incision or by combining the stab incisions for screw insertion on the side from which the cage was inserted.
3. Statistical analysis
Stata ver. 11 (Stata Corp., College Station, TX, USA) and the IBM SPSS statistical software package ver. 25.0 (IBM Corp., Armonk, NY, USA) were used for all statistical analyses. Continuous data were reported as median (±interquartile range) and compared across surgical groups using a Kruskal-Wallis test with Bonferroni correction for multiple comparisons. Pearson’s chi-square test was used to evaluate differences in categorical variables between groups. A repeated measure mixed-effects model with imaging time point as a fixed-effects variable was used to analyze changes in COMI score over time within each surgical procedure group. The Bonferroni method was used for post hoc analysis of pairwise comparisons between different time points.
To evaluate the effect of surgical procedure components on patient-reported outcomes, total COMI scores at each time point were compared across different surgical procedures (PLIF-BMS, PLIF-Wiltse, MI-TLIF, open TLIF, and PLF only) using Kruskal-Wallis test with multiple comparisons. Ordinal logistic regression was used to assess the effect of patient demographics (age, gender, and BMI), surgical indication, operated level, and surgical approach on COMI scores at each pre- and post-surgery time point.
Discussion
In this large, single-center study, we investigated the perioperative and intermediate-term clinical outcomes of patients with various posterior lumbar fusion methods. Our findings show that irrespective of the technique used, postoperative COMI scores were lower than pretreatment, with the largest improvement in patient-reported outcomes recorded in the first 3 months post-surgery. Except for patients undergoing PLF without interbody cage placement, who had worse outcomes at 1 year, all lumbar fusion techniques had comparable patient-reported outcomes, and there was no sustained difference in clinical outcomes following open versus minimally invasive techniques at 2 years post-surgery.
Previous studies have demonstrated benefits of minimally invasive TLIF over open T/PLIF with smaller wounds, reduced blood loss, faster recovery, and shorter hospital stay [
5–
8]. Our center’s findings show that patients receiving MI-TLIF had significantly shorter postoperative visits than open procedure groups. Despite improvements in short-term/perioperative outcomes, our data did not support a significant difference between open and minimally invasive approaches in patient-reported outcome measures, and previous studies and systematic reviews comparing minimally invasive and open lumbar fusion techniques support this finding, demonstrating no differences in intermediate and long-term patient-reported outcome scores [
5–
7,
9].
A key strength of our study is that alongside permitting comparison between minimally invasive TLIF and open P/TLIF, it also allows a comparison between different open fusion procedures with or without using an interbody cage. The main goal of interbody fusion surgery, irrespective of technique, is to decompress neural structures, restore disc height and lumbar lordosis, and stabilize the spine [
10]. The comparable patient-reported outcomes across different fusion techniques in this and other studies indicate that, while some techniques, such as those incorporating a muscle-splitting approach and minimally invasive screw insertion, are expected to produce less tissue trauma and shorter postoperative stay [
6], this ultimately has little bearing on the intermediate to long-term outcomes of these procedures. Our data showed a nonsignificant tendency toward worse patient-reported outcome measures in patients undergoing solely PLF. Previous research demonstrated that open lumbar fusion procedures integrating interbody cage implantation improve fusion rates, back discomfort, and postoperative functional status in patients with lumbar fusion for spondylolisthesis [
11–
13]. The fact that we did not analyze rates of radiological fusion or restoration of lumbar lordotic angles is a limitation of our study [
14], but likely, the reason for the reduced pain and better functional outcomes in patients undergoing interbody fusion compared with PLF alone is multifactorial, reflecting higher fusion rates, better correction of lumbar lordosis, and more complete foraminal decompression [
11–
13].
Although there was a trend in our research cohort toward higher rates of revision surgery in the PLF-only group and higher rates of dural tear rate in the PLIF-BMS group, these differences did not reach statistical significance. Although some previous studies have indicated greater revision rates for displaced allografts in MI-TLIF patients [
15], other authors have found reduced complication rates when using MI-TLIF [
16,
17]. The overall revision surgery rate in this analysis was higher than in some recent series [
6]. This could be due to differences in the patients and procedures included in the studies, but it could also be due to the extended length of follow-up (>10 years) for some of the earliest recruited patients in our analysis compared with other series. Previous authors have discussed the challenging learning curve associated with minimally invasive fusion, which makes certain complications, particularly those related to instrumentation, more likely [
17]. For example, the use of tubular dilator retractors has been proposed to result in an increased incidence of radiculopathy due to poorer visualization of spinal structures and hence less adequate decompression, and this learning curve may explain the discordant findings across the literature in terms of complication rate and revision surgery rate [
17].
Although the primary goal of this study was to evaluate the clinical outcomes of patients undergoing different lumbar fusion techniques, our finding that higher BMI was associated with worse preoperative and postoperative patient-reported outcomes is consistent with previous studies [
18]. Other authors, however, have shown no clear relationship between BMI and pain outcomes following lumbar surgery, particularly in patients undergoing MI-TLIF [
19,
20]. Our demonstration that advancing age was not a predictor of poorer postoperative outcomes, with younger patients having worse preoperative and postoperative scores, is consistent with the literature showing equivalent, if not improved, outcomes from lumbar fusion in patients over 65 years [
21]. A previous study has also indicated inferior outcomes of lumbar fusion in patients with recurrent degenerative disc disease [
22] and lytic spondylolisthesis [
23], and our data support this, demonstrating an association with poorer outcome measures at 2 years.
To the best of our knowledge, this is one of the largest single-institution studies comparing patient-reported clinical outcomes across open and minimally invasive lumbar fusion techniques. Other large studies have often reported outcomes at just one postoperative timepoint [
6,
10], and a key strength of this study is that through a prospective collection of COMI data by a dedicated spinal research team, we were able to achieve assessment of both short-term (3 months) and intermediate-term (1 or 2 years) outcomes. There are, nonetheless, limitations to our study. Recent large series have used propensity-score matching to reduce bias and balance surgical groups on preoperative factors, including age, sex, previous surgery, and preoperative reported outcomes [
10]. However, debate in the literature about the use of propensity-score matching for identifying treatment effects [
10,
24] and the strength of the regression analysis adopted within this study is that alongside interrogating treatment-related effects, it also allowed the identification of other key variables (age, BMI, and preoperative COMI score) that impact on postoperative patient-reported outcomes in addition to interrogating treatment-related effects. An advantage of our single-center study is that collection of patient-reported outcome data, length of stay, and other perioperative outcomes was standardized. However, surgeries were performed across different consultant neurospinal and spinal surgeons. While we were able to compare across different open and minimally invasive lumbar fusion techniques, the effect of individual surgeon technique data was not analyzed. There was also heterogeneity within each surgical approach regarding the technique used and surgical indication. A further source of heterogeneity and potential bias is that complete COMI follow-up data were unavailable for all patients. Within our study, we have sought to account for this heterogeneity through dedicated subgroup analyses of patients with complete COMI data and patients undergoing surgery for the most common surgical indications. These subgroup analyses demonstrate comparable results to the entire study cohort and support our main finding that irrespective of the lumbar fusion approach used, patients improve following surgery with equivalent patient-reported outcomes at 2 years posttreatment.
We do not routinely perform postoperative imaging on lumbar fusion patients with a symptomatic improvement in our center. Therefore, radiographic variables were not evaluated, such as pelvic incidence, pretreatment and posttreatment alignment, restoration of normal lordosis, and correction of focal kyphosis [
10]. Therefore, future studies incorporating radiographic data and longer follow-up beyond 2 years to capture later postoperative malalignment should be undertaken.