 |
 |
- Search
| Asian Spine J > Volume 17(5); 2023 > Article |
|
Abstract
Purpose
To look into the age- and gender-matched incidences of morphological changes and their severities.
Overview of Literature
There have been several prior research on the prevalence and severity of age-related diseases, both related and unrelated. Those offer some fundamental clinical data for clinicians.
Methods
Radiograms of 1,496 patients (555 males and 941 females) from the first to 9th decade were examined for this study. Sagittal and coronal alignment, disc space narrowing, spur formation including diffuse idiopathic spinal hyperostosis (DISH), spondylolisthesis, and ballooned discs associated with biconcave bodies due to osteoporosis were among the parameters of lumbar spine morphologies examined on high-quality radiographs by both human observers and computers.
Results
The alignment of the lumbar spine altered after birth and set at growth maturity, and then the curve was maintained till the end of the 5th decade afterward and the curve gradually hypolordotic. There were three types of coronal alignment abnormalities can be seen: idiopathic, osteopathic, and discogenic (degenerative lumbar scoliosis [DLS]). DLS developed after 6th decade. There was no scoliosis associated with spondylolysis or the post-laminofacetectomy period. Disc space narrowing and corporal spur formation were not seen till the end of 3rd decade comparatively speaking, the corporal spurs generated in the non-scoliotic spine were smaller than those in the scoliotic spine. DISH began to appear in the 5th-decade patients and its incidences increased gradually afterward. Porosis-related vertebral body collapse started to happen after 6th decade. There are three different types of spondylolisthesis: anterior, posterior, and lateral. The lateral slip occurred only in the scoliotic spine. All types were related to degenerative discs.
There have been many previous investigations of lumbar spine morphology in the English and Korean literatures [1-12]. According to the senior authorsŌĆÖ understanding, no one has yet conducted a systematic study of the age-related morphological alterations of the lumbar spine. Based on this information, the current authors created and performed the current study to give clinical material data for the practicing spine surgeons for their reference.
Case numbers of each decade (from 1st to 9th) are listed in Table 1. The study materials included 1,496 Jeju islanders from Korea from the first to 9th decade, including 555 men and 941 women, who had high-quality anteroposterior and lateral radiograms of their lumbar spines (Table 1).
This study was approved by the Institutional Review Board of Cheju Halla General Hospital (IRB approval no., CMC-MKIOR 121). Informed consent were not obtained because of a non-patient study using simple radiograms.
We performed in this study as follows: (1) age-related normal lumbar curve: coronal alignment, sagittal alignment; (2) abnormal alignment: coronal, sagittal; (3) disc degeneration: incidences; (4) disc degeneration associated spur formation (spur sizes and alignment): coronal alignment-related (normal alignment, abnormal alignment [scoliotic]), diffuse idiopathic spinal hyperostosis (DISH) (normal disc); (4) olisthesis: normally aligned lumbar spine, abnormally aligned lumbar spine; and (5) ballooned discs with biconcave vertebral body.
Different morphological parameters such as anteroposterior and sagittal alignment in an upright posture, incidences of disc space narrowing, corporal spur formation, dorsolumbar kyphosis, degenerative lumbar kyphosis, lumbar scoliosis (idiopathic, osteopathic, and degenerative), spontaneously and/or minor-trauma-induced vertebral body collapse, DISH, ballooned discs related to biconcave vertebral bodies without a cortical break due to severe osteoporosis, and so forth.
Type of alignment and factors contributing to alignment abnormalities include idiopathic, osteopathic, congenital hemivertebra, trauma-induced lateral wedged vertebra, and discogenic and iatrogenic alignment abnormalities brought on by disc degeneration
It is measured by defining the lumbar spine into four categories: normal (40┬░ lordosis), hypolordosis (20┬░ lordosis), kyphosis (<5┬░ lordosis), and hyperlordosis (>75┬░ lordosis).
The 1st decadeŌĆÖs normal alignment was altered during the growth phase, set at growth maturity, and then maintained along the lordotic curve to the end of the 5th decade. Afterward, the curve is gradually hypolordotic. The trend of changing alignment is depicted in Table 2 and Fig. 1. A case of compensatory hyperlordotic lumbar spine secondary to osteopathic (osteoporosis) dorsolumbar kyphosis is shown (Fig. 2).
Incidences in 221 6th-decade patients were zero in 113 males and 0.9% in 108 females, 0.9% in 108 males, and 1.0% in 199 females among the 307 7th-decade patient. Patients in the 38 4th decade had 1.3% of men and 3.2% of women, whereas those in the 23 9th decade had 4.5% of men and 5.6% of women (Fig. 3). Post-trauma (fracture) dorsolumbar kyphoscoliosis: There were a few cases of trauma-induced dorsolumbar kyphosis were discovered (Figs. 4ŌĆō6).
In none, this type of deformity was seen till the end of the 7th decade. A few elderly people in the 8th and 9th decades of life experienced this kind of malformation.
Incidences were 0% in 108 men and 1.5% in 199 women among the 307 patients in the 7th decade, 0% in 75 men and 3.9% in 384 (75 men and 309 women) in patients in the 8th decade, and 2.3% in 44 men and 9.7% in 195 women among the 239 patients in the 9th decade. There was a case of congenital kyphoscoliosis (Table 8).
The degree of narrowing is graded into six categories: normal (0), douftful (┬▒), 25% narrowing (+), 50% narrowing (++), 75% narrowing (+++), and 100% narrowing (++++).
None of the patients exhibited disc space changes by the end of the 3rd decade. In the 101 4th-decade patients two patients (1.9%; one male and one female) had questionable disc space narrowing. Twenty-six patients (25%; 15 males and 11 females) had narrowing (+), nine (five males and four females) had 50% bringing the total of 37 patients (36.0%). None of 3rd- and 4th-decade patients had narrowing over 75% (+++) to 100% (++++) (Table 9). The remainders in the 5thŌĆō9th decades are depicted in Tables 3ŌĆō7.
Two distinct spur shapes (claw and traction) were measured as one in this study. Small size is less than 3 mm in 5 lengths, and large size is over 3 mm. A significant corporal spur that projects horizontally from the spine on sagittal radiographs indicates the presence of DISH.
The average percentile incidence of lumbar spine curvature in the 4th, 5th, and 6th decades was 2.9%, 4.5%, and 7.2%, respectively. Coronally scoliotic lumbar spine: The average percentile incidences of the 4th, 5th, and 6th decades were 9.5%, 10.7%, and 11.8%, respectively.
Coronally straight lumbar spines: Incidences of the 4th, 5th, and 6th decades were 3.9%, 5.2%, and 9.5%, respectively. Coronally scoliotic lumbar spines: The incidences of the 4th, 5th, and 6th decades were 16.8%, 17.4%, and 22.2%, respectively.
ISH cases were nonexistent in the 1st, 2nd, 3rd, and 4th decades. The incidences of DISH in the 5th, 6th, 7th, 8th, and 9th were 1.3% (0.9%/1.9%), 2.3% (2.7%/1.9%), 3.6% (6.5%/1.5%), 39% (12%/1.9%), and 5.0% (15.9%/2.7%), respectively.
Vertebral body shape is analyzed by its images on coronal and sagittal radiograms from T11 to L5. The evaluation was conducted using the classification by Genant [13]. of wedged, biconcave, and crush (flat) fractures in osteoporotic bone.
Dorsolumbar kyphosis is assessed by its shape: angular and round back shape.
The incidences of all types of spontaneous and/or minor trauma-induced vertebral body collapses from T11 to L5, including the wedge, biconcave, and crush described by Genant [13], were examined. Additionally, fractures severity was divided into four categories: grade 0: no fracture; grade I: mild fracture (approximately 20%ŌĆō25% height reduction); grade 2: moderate fracture (approximately 25%ŌĆō40% height reduction); and grade 3: severe fracture (>40% height reduction).
Asymmetric disc degeneration-related lateral tilting and/or osteopathy (congenital or fracture-induced laterally wedged vertebral body) are the two main characteristics of lumbar scoliosis (Table 8).
Three types of coronal alignment abnormalities can be observed: idiopathic, osteopathic, congenital, or fracture-induced laterally wedged vertebra and discogenic. In the current study series, only three patients had idiopathic hemivertebra: one in the 2nd decade and two in the 7th decade. No one had congenital hemivertebra. The remainder were discogenic (discopathic), especially in females.
1) Idiopathic scoliosis: Only three cases were found: one in the 2nd-decade female and two in the 7th-decade females (Figs. 12, 13).
2) Vertebral body fracture-related (osteopathic) scoliosis: There was one case (0.3%) among the 307 7th-decade patients, 19 (6.1%) among the 309 8th-decade females, and 8 (3.0%) among the 195 9th-decade patients.
3) There was one case of L1 congenital kyphoscoliosis case (Fig. 14).
4) Degenerative lumbar scoliosis (Table 9): The occurrences of 29 degenerative lumbar scoliosis (DLS) (13.1%; three males/26 females) among the 221 6th-decade patients (113 males/108 females), 45 (14.7%; 10 males/35 females) among 307 7th-decade patients (108 males/199 females), 64 (16.7%; 11 males/53 females) among the 383 (44 males/309 females) 8th-decade patients, and 64 (25.8%; 18 males/46 females) among 239 (44 males/195 females) 9th-decade patients (Figs. 15ŌĆō24).
5) SpondylolysisŌĆōrelated scoliosis: In this series, none had scoliosis.
6) Post-laminofactectomy-related scoliosis: There were none. Sondylolisthesis is defined when the vertebral body displaces at the disc level anteriorly, posteriorly, or laterally (rotatory lateral). Vertebral body displacement at the disc level in an anterior, posterior, or lateral direction is known as sondylolisthesis (rotatory lateral). Vertebral bodies typically shift one level, although on rare occasions they shift two levels in the same or the opposite direction.
No cases having either type of spondylolisthesis till the end of the 4th decade. The 155 5th-decade patients had spondylolisthesis nine patients (five males/four females) with a coronally straight spine. There were no cases of scoliosis. Among the 221 6th-decade patients (113 males/108 females), there were 19 patients with olisthesis (three anteriolisthesis and one retrolisthesis), while in the patients with scoliosis, eight had olisthesis (two anteriolisthesis, one retrolisthesis, and five laterolisthesis). Table 13 and Table 14 lists the prevalence of olisthesis in the 7th, 8th, and 9th┬Āgrades (Fig. 15).
Incidences of slip in coronally normally aligned spine is as follows. There were no olisthesis in the 1st-, 2nd-, 3rd-, and 4th-decade patients. Overall incidences in the 5th-decade patients were two (zero in males and two in females): one antero-listhesis and one retrolisthesis at L3, four cases (one male and three females) at L4 levels, and four males at L5. Overall incidences in the 6th-decade patients were zero at L1 and L2, one anterolisthesis at L3, 14 (13 anterolisthesis: five males, 18 females) at L4 disc level, and three anterolisthesis (one male/12 females) at joint L5 level. Overall incidences in the 7th, 8th, and 9th decades and listed in Table 15.
None slip was found. In the 6th-decade patients, there were five laterolisthesis in females at L3 disc level, two slips (one anterolisthesis and one retrolisthesis) at L4 disc level, and one anterolisthesis at L5. In the 7th-decade patients, there were one anterolisthesis and four retrolisthesis in five females at L3 disc level and 16 olisthesis (three males/13 females; 15 anterolisthesis and one laterolisthesis at L4 disc level and one anterolisthesis in one female at L5). In 8th- and 9th-decade patients, slips were not found.
The incidences of all types of vertebral body collapse (wedged, biconcave, and crush [flat]) in the 5th, 6th, 7th, 8th, and 9th decades were 12.3% (6.5% in male and 23.5% in female), 18.5% (10.0%/25.9%), 25.4% (18.5%/29.1%), 32.5% (34.7%/32%), and 38.4% (27.3%/41.0%), respectively. In patients in the 7th, 8th, and 9th decades, the overall percentile occurrences of biconcave vertebral bodies linked to inflated discs were 0.95% (0.9%/1.0%), 4.4% (1.3%/5.1%), and 16.7% (9.1%/18.5%), respectively (Tables 14, 16).
It was stated by the authors in the introduction that there are many previous studies related to lumbar spine morphology. However, nobody has yet carried out repeated systematic research on the age-related morphology of the lumbar spine. In the current study, the senior author created the survey chart and performed the roentegenological study of the lumbar spine, according to the study design.
A recent study on sagittal alignment revealed that once normal lordosis in the lumbar spine develops, it is maintained through the end of the third decade, and that disc degeneration causes it to become increasingly hypolordotic after that. The incidences of disc degeneration in the 4th decade lumbar spine were higher (36.6%) than those (13.2%) of the cervical spine. More load-bearing is thought to be the root of the higher occurrence. When vertebrae collapsed, the lumbar spine in certain cases became hypolordotic.
Dorsolumbar kyphosis is created by osteoporotic vertebral fractures of dorsolumbar spine (Table 2), and in some cases developed lumbar kyphosis due to disc degeneration.
Regarding the three types of coronal lumbar spine alignment abnormalities in the present series, there were no congenital ones (hemivertebra), and only three patients among the 1,496 surveyed patients had idiopathic scoliosis. The majority of discogenic remaining syndromes (DLS) were found in females over 50 years, and as time went on, the prevalence of DLS increasingly rose. This fact has great clinical significance related to lumbar spinal stenosis in DLS patients. There were no incidences of spondylolysis- and post-laminofacetectomy-related scoliosis in the current series (Table 12).
It is a known fact that spondylolisthesis can occur either in the normally aligned or scoliotic lumbar spine. No cases were having degenerative spondylolisthesis till the end of the 4th decade in the current series. It is interesting to notice that anterior- and retro-listhesis occurred both in the normally aligned and scoliotic lumbar spine, while laterolisthesis (rotatory) occurred only in the scoliotic spine. Additionally, these facts imply that disc degeneration owing to facet disease is what drives the progression of scoliosis with age.
It was discovered that age-related disc degeneration begins to develop in the 4th decade and steadily increases in incidence and severity in conjunction with the growth of the corpus callosum (Tables 8, 9). Spur formation in association with the disc space narrowing occurred only in the non-porotic spine, while disc space narrowing and spur formation did not occur in porotic spine, and the osteoporotic spine revealed wedged, biconcave, and crushed bodies (Genant [13]). In contrast to the coronally scoliostic spine with a huge spur, the straight-aligned spineŌĆÖs spur diameters were smaller. This fact suggests the reason for the clinically relatively higher incidence of lumbar stenosis in the degenerative scoliosis patient in comparison with those of the non-scoliotic spine.
DISH was not discovered in first to 4th-decade patients and then occurred from the 5th decade onward. However, the current authors failed to find out reasonable causes.
Regarding vertebral body collapse brought on by spontaneous or minor trauma, collapses were noted in patients as early as the 5th decade and gradually increased over time, and biconcave vertebral bodies related to the ballooned disc were observed in the 7th-, 8th-, and 9th-decade patients with an increasing tendency (Table 14).
The shortcomings of this research are inequality of case numbers in each decade, lack of computed tomography and magnetic resonance imaging images in all cases, and lack of study on the musculature contribution to the lumbar spine morphology.
Fig.┬Ā1.
Upright standing anteroposterior (AP) and lateral view of lumbar spine of first-, second-, and third-decade patients. (AŌĆōC) First decade patients: 4-year-old girl, 19-year-old girl, and 23-year-old lady. (DŌĆōF) Second decade patients: 36-year-old lady, 47-year-old lady, and 55-year-old lady. (GŌĆōI) Third decade patients: 64-yearold lady, 78-year-old lady, and 81-year-old lady.
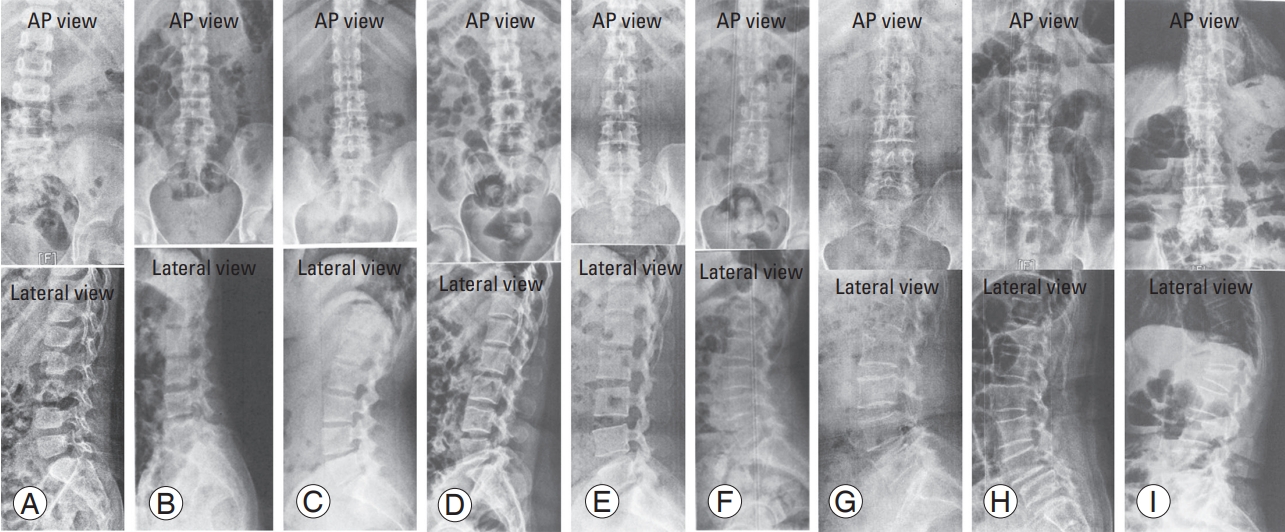
Fig.┬Ā2.
An example of an 88-year-old lady with a hyperlordotic lumbar spine due to biconcave vertebral and ballooned discs. Anteroposterior (A) and lateral (B) view.
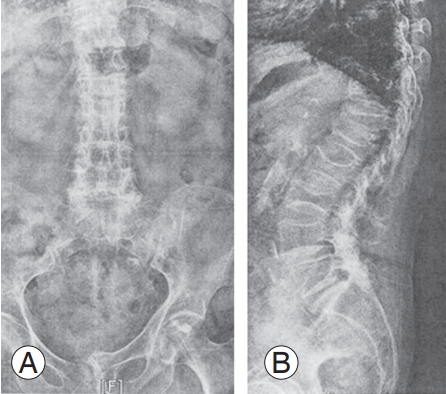
Fig.┬Ā3.
An example of a 40-year-old lady with degenerative kyphosis. Anteroposterior (A) and lateral (B) view.

Fig.┬Ā4.
An example of a 59-year-old male with wedge-fractures (T11 and T12) induced dorsolumbar kyphosis. Anteroposterior (A) and lateral (B) view.
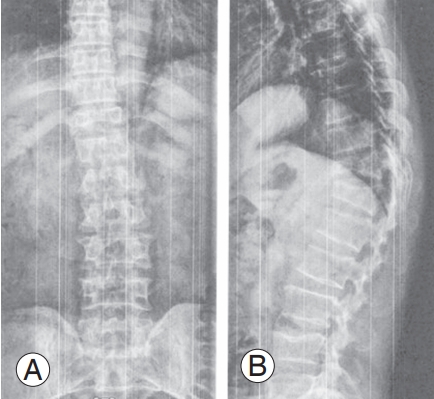
Fig.┬Ā5.
Radiograms show flattered lumbar spine with L2 anteriolisthesis with narrowed disc spaces (L2ŌĆō3, L3ŌĆō4, L4ŌĆō5, and L5ŌĆōS1) in a 60-year-old man. Anteroposterior (A) and lateral (B) view.
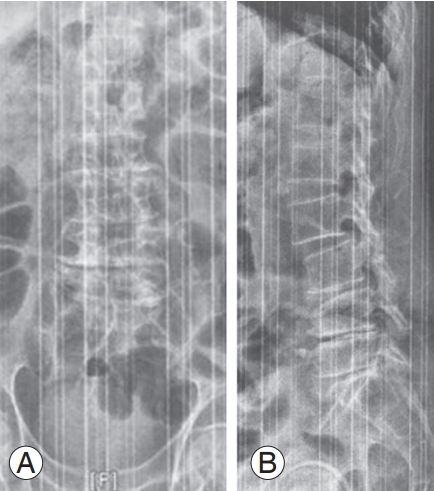
Fig.┬Ā6.
Lower type degenerative lumbar kyphosis in late stage 2 in a 75-yearold lady. KnuttsonŌĆÖs sign which indicates the instability. Anteroposterior (A) and lateral (B) view.

Fig.┬Ā7.
Radiograms show mid-sized claw spurs without disc space narrowing in a 47-year-old man. Anteroposterior (A) and lateral (B) view.

Fig.┬Ā8.
Radiograms show narrowed L2ŌĆō3 disc space with spur formation in a 23-year-old man. Anteroposterior (A) and lateral (B) view.
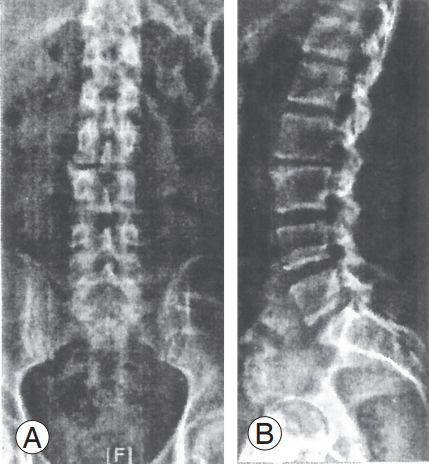
Fig.┬Ā9.
(A, B) Hyperostosis of multi-level lumbar spine with disc space narrowing in a 53-year-old lady. (C, D) Hyperostosis of entire lumbar spine with disc space narrowing in a 84-year-old man.

Fig.┬Ā10.
Radiograms show the large corporal spurs of the entire lumbar spine with well-maintained disc spaces which indicate the diffuse idiopathic spinal hyperostosis in a 60-year-old man. Anteroposterior (A) and lateral (B) view.
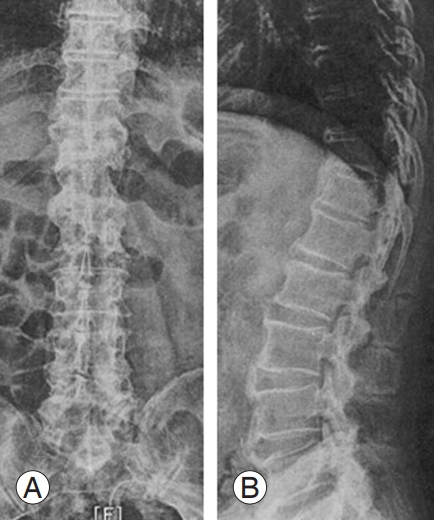
Fig.┬Ā11.
Radiograms show huge corporal spurs in entire lumbar spine with relative well-maintained disc spaces (diffuse idiopathic spinal hyperostosis) in a 96-year-old male. Anteroposterior (A) and lateral (B) view.
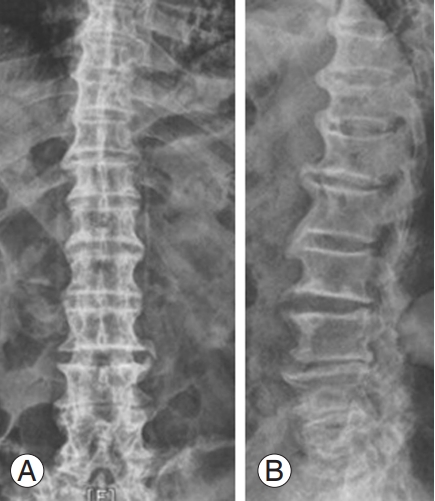
Fig.┬Ā12.
Anteroposterior and lateral radiograms showing idiopathic scoliosis in a 15-year-old girl (A, B) and a 52-year-old lay (C, D). Above shown radiograms are two out of three persons in the current series.
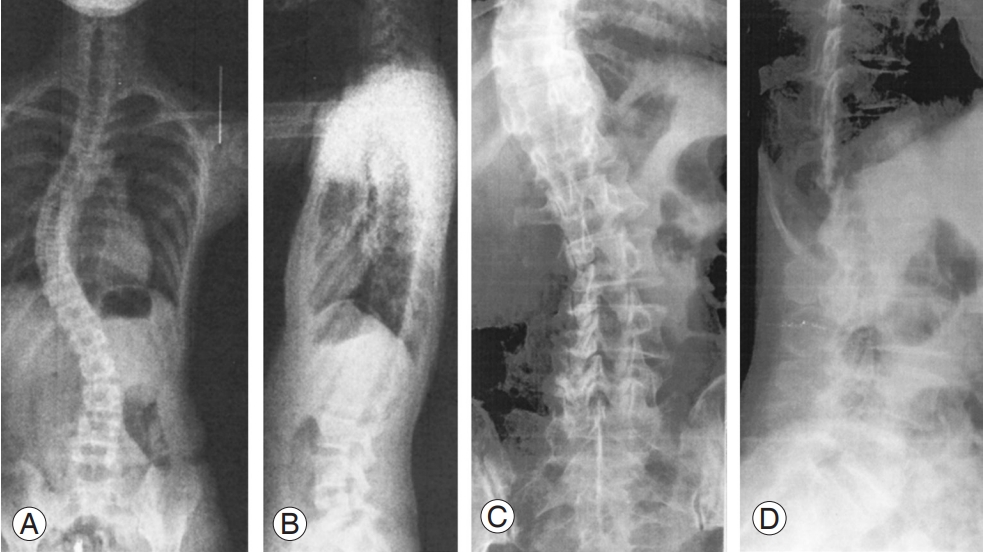
Fig.┬Ā13.
Lumbar radiograms of a 66-year-old lday with idiopatheic adult scoliosis and L4 anteriolisthesis. Anteroposterior (A) and lateral (B) view.
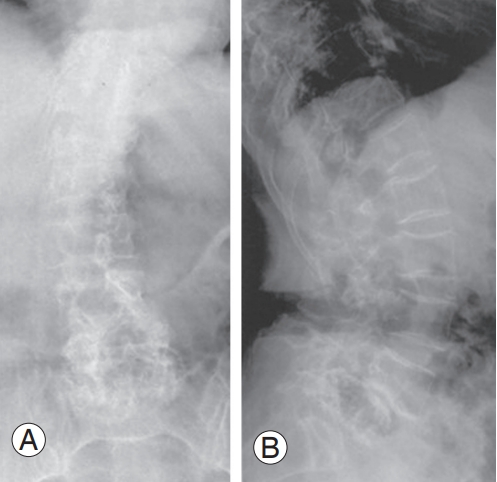
Fig.┬Ā14.
An example of a congenital osteopathic kyphoscoliosis case aged 48-year-old lady. Anteroposterior (A) and lateral (B) view.

Fig.┬Ā15.
(A, B) An example of osteopathic kyphoscoliosis (coronally wedged fused L3ŌĆō4 bodies in a 91-year-old lady.
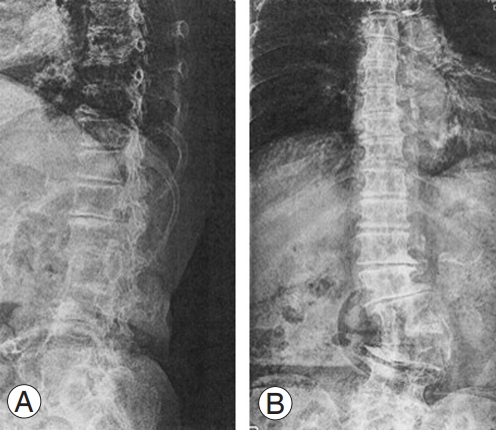
Fig.┬Ā16.
(A, B) Low-level origin degenerative lumbar scoliosis (DLS) in a 71-year-old lady. (C, D) Mid-level origin DLS. (E, F) Higher-level origin DLS.
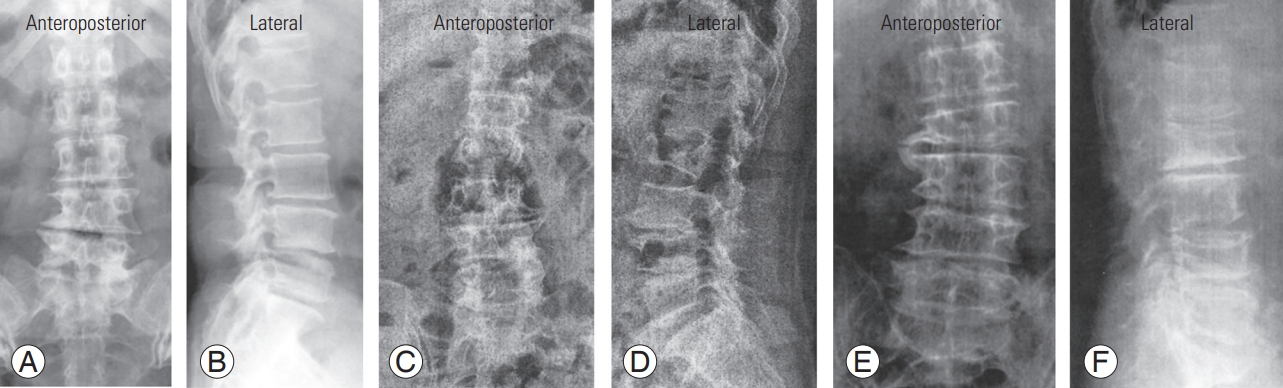
Fig.┬Ā17.
Low level type (double curve). High a level origin degenerative lumbar scoliosis (DLS): (A, B) 43-year-old lady, (C, D) 50-year-old lady, (E, F) 48-year-old lady, and (G, H) 66-year-old male. (I, J) Mid-level origin DLS: 71-year-old lady.
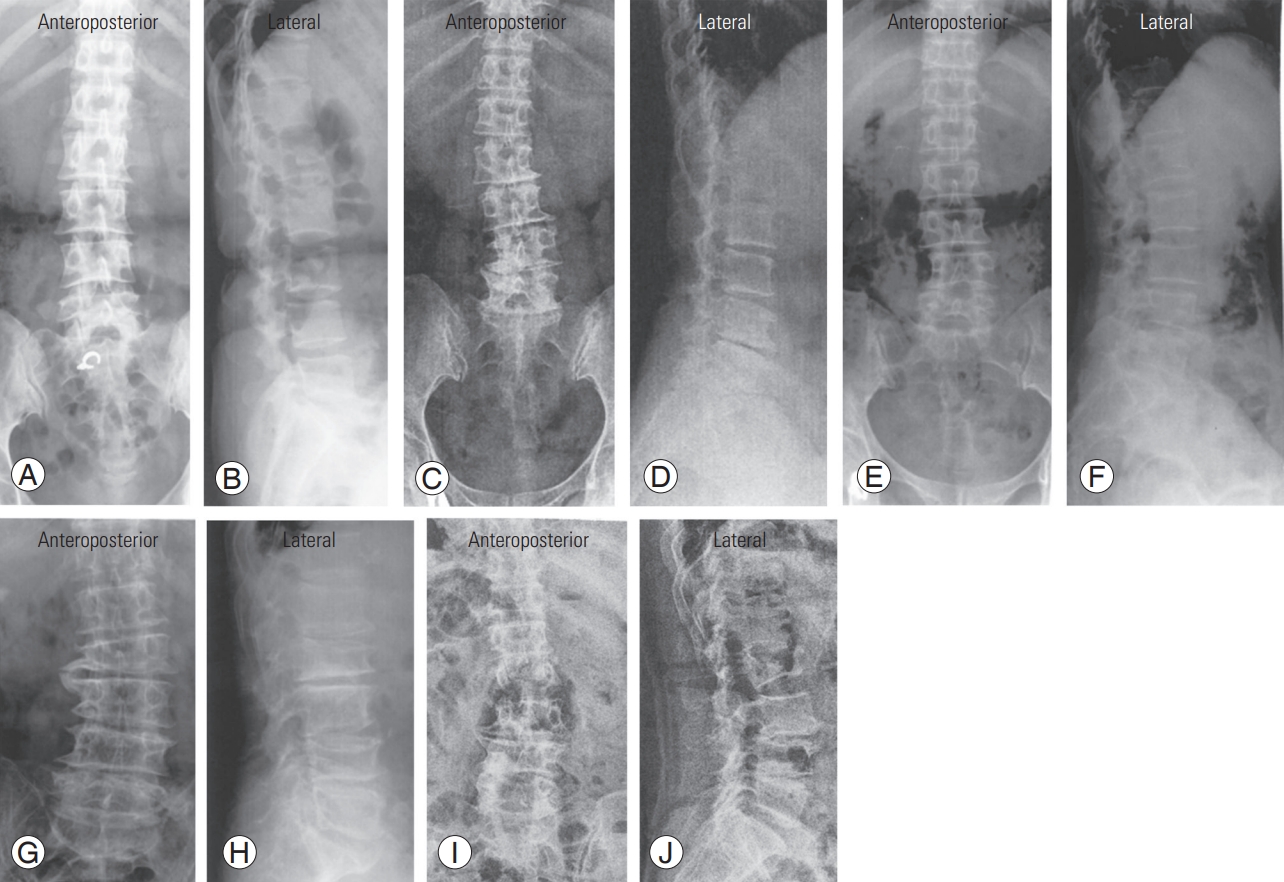
Fig.┬Ā18.
An example of low-level origin kyphoscoliosis in a 48-year-old lady. Anteroposterior (A) and lateral (B) view.

Fig.┬Ā19.
Radiograms show degenerative kyphoscoliotic spine in a 92-year-old lady. Anteroposterior (A) and lateral (B) view.

Fig.┬Ā20.
An example of degenerative lumbar scoliosis with large spurs at upper (L2ŌĆō3 disc) and small spurs at all adjacent segements in a 59-year-old lady. Anteroposterior (A) and lateral (B) view.
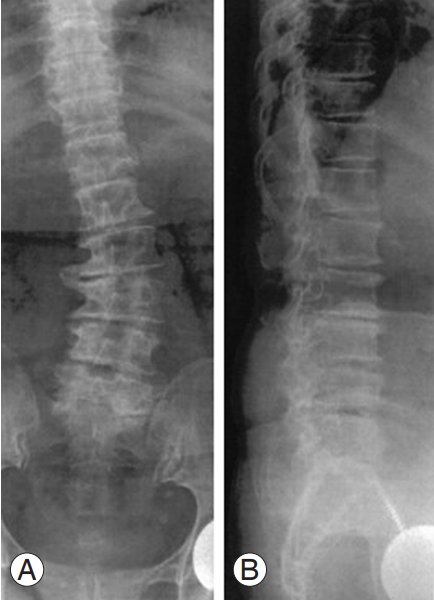
Fig.┬Ā21.
An example of multilevel disc space narrowing and small spur formation in an 83-year-old lady. Anteroposterior (A) and lateral (B) view.

Fig.┬Ā22.
An example of osteopathic angular scoliosis in a 56-year-old female (apex L1ŌĆō2 disc). Anteroposterior (A) and lateral (B) view.
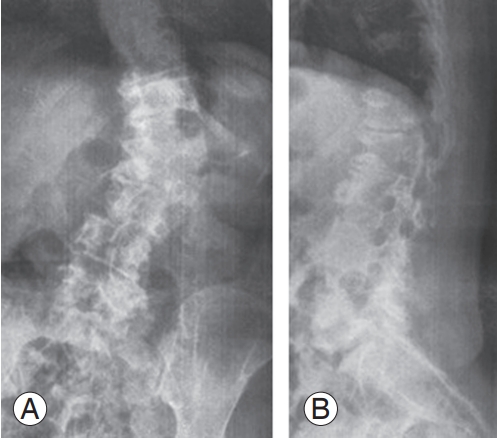
Fig.┬Ā23.
Radiograms show kyphotic lumbar spine with L2 anteriolisthesis with normal disc spaces (L2ŌĆō3, L3ŌĆō4, L4ŌĆō5, and L5ŌĆōS1) in a 60-year-old man. Anteroposterior (A) and lateral (B) view.
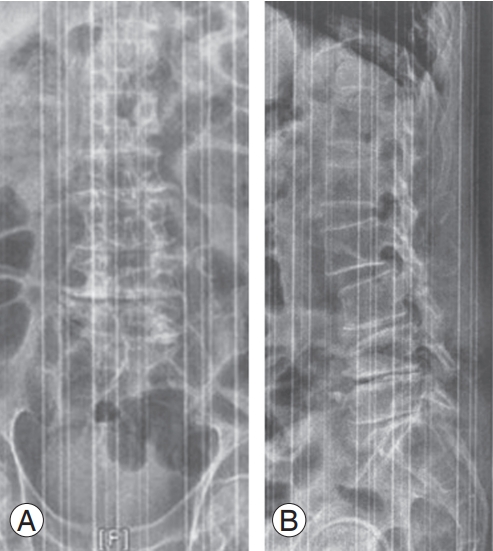
Fig.┬Ā24.
Radiograms of three different persons. (A, B) Biconcave vertebral bodies (L2, L3) and ballooned discs are shown. (C, D) Biconcave T12ŌĆōL3 bodies and ballooned discs and crushed (flat) L4 are shown. (E, F) Wedged L2, biconcave L3, and crushed L4 body shown.

Table┬Ā1.
Case numbers of each decade
|
Decade |
Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1st | 2nd | 3nd | 4th | 5th | 6th | 7th | 8th | 9th | ||
| Males | 10 | 19 | 46 | 67 | 104 | 113 | 108 | 44 | 44 | 555 |
| Females | 10 | 14 | 21 | 34 | 51 | 108 | 199 | 309 | 195 | 941 |
| Total | 20 | 33 | 67 | 101 | 155 | 221 | 307 | 383 | 239 | 1,496 |
Table┬Ā2.
Definition and ratio of sagittal lumbar curves of 1,548 patients: first to 9th decade
Table┬Ā3.
Degree of disc space narrowing at each lumbar spinal level in 67 third and 101 fourth decades
Table┬Ā4.
Degree of disc space narrowing at each lumbar spinal level in 104 5th decade and 113 6th decade
Table┬Ā5.
Degree of disc space narrowing at each lumbar spinal levels in 307 (108/199) 7th decade patients and 384 (75/309) 8th decade patients
Table┬Ā6.
Degree of disc space narrowing at each lumbar spinal level
Table┬Ā7.
Types of scoliosis by its causes
Table┬Ā8.
Incidences of DLK
Table┬Ā9.
Incidences of DLS in each decade patients
Table┬Ā10.
Incidences of corporal spur formation (claw and traction spurs) in IV, V, VI decade patients
Table┬Ā11.
Incidences of corporal spur formation (claw and traction spurs) in VII, VIII, IX decade patients
Table┬Ā12.
Incidences and slip direction of vertebra (spondylolisthesis) in the coronally straight and scoliotic spine in each decade patients
Table┬Ā13.
Incidences and slip direction of vertebra (spondylolisthesis) in the coronally straight and scoliotic spine in each decade patients
Table┬Ā14.
Incidences and slip direction of vertebra (spondylolisthesis) in the coronally straight and scoliotic spine in 307 (108/199) 7th decade patients
|
Segment decade |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
L1 |
L2 |
L3 |
L4 |
L5 |
||||||||||||
| 7th | 8th | 9th | 7th | 8th | 9th | 7th | 8th | 9th | 7th | 8th | 9th | 7th | 8th | 9th | ||
| No. of patients (M/F) | 307 (108/199) | 383 (44/309) | 239 (44/195) | 307 (108/199) | 383 (44/309) | 239 (44/195) | 307 (108/199) | 383 (44/309) | 239 (44/195) | 307 (108/199) | 383 (44/309) | 239 (44/195) | 307 (108/199) | 383 (44/309) | 239 (44/195) | |
| Coronally straight spine | 0 | 7 (2/5a)) | 26 (1/25) | 5 (1/4) | ||||||||||||
| Slipdinection | 26a) (1/25b)) | |||||||||||||||
| Anterlisthesis | 3 (2/1a)) | 5a) (1/4b)) | ||||||||||||||
| Retrolisthesis | 1 (1/0) | 4 (0/4) | 0 (0/0) | |||||||||||||
| Coronally straight spine | 0 | 0 | 5 (0/5) | 16 (3/13) | 1 (0/1) | |||||||||||
| Anterlisthesis | 1 (0/1) | 15 (2/13) | 1 (0/1) | |||||||||||||
| Retrolisthesis | 4 (0/4) | 0 (0/0) | 0 (0/0) | |||||||||||||
| Laterolisthesis | 0 (0/0) | 1 (1/0) | 0 (0/0) | |||||||||||||
| Total | ||||||||||||||||
Table┬Ā15.
Incidences of DISH in each decade
Table┬Ā16.
Balloned discs associated biconcave vertebra due to osteoporosis in aged lumbar spines
References
1. Moon MS, Kim BK. Radiological studies on lumbosacral joints in the healthy Korean adults. J Korean Orthop Assoc 1975;28:151ŌĆō9.
2. Moon MS, Lee KS, Lim CI, Kim YB, Lee HS. A clinical study of degenerative lumbar scoliosis. J Korean Orthop Assoc 1992;27:946ŌĆō55.


3. Moon MS, Lee BJ, Kim SS, Lin JF. Evaluation of management of spinal deformities: controversial issues and current concept review. J Spinal Surg 2010;2:295ŌĆō305.
4. Moon MS, Kim SS, Lee BJ, Lim JF. Degenerative lumbar scoliosis: an update: controversial issues and a new challenge. J Spinal Surg 2011;2:439ŌĆō50.
5. Truumees E. The role of fusion in degenerative lumbar disease. Semin Spine Surg 2003;15:430ŌĆō59.

6. Epstein E. The spine. 2nd ed. Philadelphia (PA): Lee and Febinger; 1969.
7. Macnab I. The traction spur: an indicator of segmental instability. J Bone Joint Surg Am 1971;53:663ŌĆō70.


8. Moon MS, Yoon MK, Kwon KT, Park MS, Park BK, Kim SS. Posterior element morphology and degenerative lumbar spondylolisthesis. J Musculoskelet Res 2015;18:1550001.

9. Kim BS, Moon MS, Yoon MG, et al. Prevalence of diffuse idiopathic skeletal hyperostosis diagnosed by whole spine computed tomography: a preliminary study. Clin Orthop Surg 2018;10:41ŌĆō6.




10. Moon MS. Unstable lumbar spine: diagnosis and assessment. Med Prog 2006;2006:386ŌĆō9.
11. Moon MS. Unstable lumbar spine: management. Med Prog 2006;2006:390ŌĆō4.
12. Moon MS, Yoon MG, Park BK, Park MS. Age-related incidence of cervical spondylosis in residents of Jeju Island. Asian Spine J 2016;10:857ŌĆō68.




13. Genant HK,Radiology of osteoporosis. Favus MJ, editors. Primer on the metabolic bone diseases and disorders of mineral metabolism. 2nd ed. Philadelphia (PA): Lippincot-Raven; 1993. p.229ŌĆō40.
- TOOLS







