 |
 |
- Search
| Asian Spine J > Volume 17(6); 2023 > Article |
|
Abstract
Purpose
This study aims to demonstrate the proper resection trajectory of a partial posterior uncinate process resection combined with anterior cervical discectomy and fusion (ACDF) and evaluate whether foraminal stenosis or uncinate process degeneration increases the risk of vertebral artery (VA) injury.
Overview of Literature
Appropriate resection trajectory that could result in sufficient decompression and avoid vertebral artery injury is yet unknown.
Methods
We retrospectively reviewed patients who underwent cervical magnetic resonance imaging and computed tomography angiography for preoperative ACDF evaluation. The segments were classified according to the presence of foraminal stenosis. The height, thickness, anteroposterior length, horizontal distance from the uncinate process to the VA, and vertical distance from the uncinate process baseline to the VA of the uncinate process were measured. The distance between the uncinate anterior margin and the resection trajectory (UAM-to-RT) was measured.
Results
There were no VA injuries or root injuries among the 101 patients who underwent ACDF (163 segments, mean age of 56.3±12.2). Uncinate anteroposterior length was considerably longer in foramens with foraminal stenosis, whereas uncinate process height, thickness, and distance between the uncinate process and VA were not significantly associated with foraminal stenosis. There were no significant differences in radiographic parameters based on uncinate degeneration. The UAM-to-RT distances for adequate decompression were 1.6±1.4 mm (range, 0–4.8 mm), 3.4±1.7 mm (range, 0–7.1 mm), 4.0±1.7 mm (range, 0–9.0 mm), and 4.5±1.2 mm (range, 2.5–7.5 mm) for C3–C4, C4–C5, C5–C6, and C6–C7, respectively.
Anterior cervical discectomy and fusion (ACDF) is a commonly performed surgical procedure for managing cervical radiculopathy with posterior cervical foraminotomy [1–3]. While indirect decompression to restore disk height and segmental fixation could result in favorable clinical outcomes [3–5], patients may experience inadequate symptom relief or recurrence after temporary postoperative improvement in cases where direct nerve root decompression involving removal of uncinate osteophytes is not performed [6–8]. Although foraminal decompression with uncinate process resection (UPR) during ACDF is associated with increased operation time and blood loss, it can achieve significantly greater improvement in arm pain in the early postoperative period than ACDF without UPR [9]. Therefore, ACDF with UPR is an effective and vital surgical method for treating cervical radiculopathy patients with severe foraminal stenosis [6–8,10].
Several surgical techniques have been reported for UPR have been reported. Some authors suggest complete resection of the exposed uncinate process while using a surgical device to protect the vertebral artery (VA) [6,8,10–12]. On the other hand, partial resection of only the posterior zone of the uncinate process, which causes nerve root compression, has been proposed [13,14]. Although both techniques are considered equally effective and have similar safety profiles, partial posterior UPR has the advantage of being less technically demanding and requiring less lateral dissection [14–16]. Furthermore, due to anatomical variations in the uncinate process and VA, complete UPR may not be achieve in some cases, increasing the risk of VA injury [17]. Therefore, surgeons should be familiar with partial UPR procedures for direct foraminal decompression during ACDF. However, partial posterior UPR may result in inadequate decompression and is not free from the risk of VA injury. A method for surgeons to determine the appropriate resection trajectory for partial UPR has yet to be developed. Furthermore, it is unknown whether the pathologies causing cervical root compression increase the risk of VA injury during UPR. Therefore, the present study aimed to identify the proper resection trajectory of a partial posterior UPR for direct decompression of the cervical nerve root and evaluate whether foraminal stenosis or uncinate process degeneration increased the risk of VA injury.
This retrospective radiographic study was conducted after obtaining approval from the review board of Dongguk University Ilsan Hospital (DUIH 2022-06-055). The requirement for informed consent was waived owing to the retrospective nature of the study. One-hundred-one patients who underwent ACDF between September 2012 and March 2020 and completed preoperative radiographic evaluations, including cervical computed tomography (CT) angiography and cervical magnetic resonance imaging (MRI) were studied.
Radiographic assessments were performed by two orthopedic surgeons. Surgeons agreed to assess foraminal stenosis and uncinate degeneration, and the analysis used the mean measurement value for each parameter. Foramens at each level were classified as either having foraminal stenosis or having uncinate process degeneration. Foraminal stenosis was evaluated using oblique sagittal T2 MRI findings, according to the classification suggested by Kim et al. [18], Park et al. [19], and Meacock et al. [20]. Foramens with >50% perineural fat obliteration around the nerve root circumferences were considered to have foraminal stenosis [19]. Uncovertebral joint degeneration was evaluated based on coronal CT findings according to the classification system proposed by Huang et al. [21]. This classification divides uncovertebral joint degeneration into five grades: (1) grade 0, normal without degeneration; (2) grade 1, mild narrowing of space or osteophyte formation; (3) grade 2, osteophyte formation with osteophytes not exceeding the intervertebral level; (4) grade 3, osteophyte formation with osteophytes exceeding the intervertebral level; and (5) grade 4, osteophyte articulation or uncinate joint fusion [21]. Uncovertebral joints with grade ≥2 were classified as “uncinate degeneration.” Coronal CT images were used to measure uncinate process height (distance from the line from the upper endplate of the vertebral body to the tip of the uncinate process) and uncinate process thickness (distance between the medial and lateral borders of the uncinate process at the plane of the upper endplate) (Fig. 1A) [22]. Furthermore, anteroposterior length, as the vertical distance between the anterior and posterior borders of the uncinate process, vertical distance from the baseline plane of the uncinate process to the VA, horizontal distance from the lateral border of the uncinate process to the VA, and horizontal distance between the right and left tips of the uncinate process, were measured based on axial CT images (Fig. 1B). All measurements were performed for the C3–C4, C4–C5, C5–C6, and C6–C7 levels.
Radiographic simulation of the proper resection trajectory of the partial UPR for adequate decompression and prevention of VA injury was performed on axial CT images with angiography. The resection trajectory was determined using the uncinate process anterior margin-to-resection trajectory (UAM-to-RT) distance because it is easier to recognize intraoperatively than the distance from uncinate base-to-burr or angulation (Fig. 2). For the radiographic simulation, the following three assumptions were made: (1) 4-cm self-retractors were placed at the uncinate process tip; (2) a high-speed burr with a 3-mm burr tip and a 5-mm-thick handpiece (Midas; Medtronic, Minneapolis, MN, USA) was used for the UPR; and (3) leaving a 3-mm gap from the VA to the resection trajectory could prevent VA injury risk.
Determining which resection trajectory would provide adequate decompression was conducted as follows: First, two self-retractors were drawn vertically at the uncinate process tip. Second, the point of the uncinate process lateral margin reaching the upper border of the caudal vertebra pedicle was identified. Because the pedicle includes the superior and inferior foramen borders, the UPR reaching the pedicle was considered to provide adequate decompression. Then, a diagonal line was drawn such that the distance from the line to the superior end of the contralateral self-retractor was 4-mm. The angle of the burr was limited by the self-retractor so that the maximum angulation was the same as the angle when the handpiece of the burr touched the self-retractor. A 4-mm margin (2.5+1.5 mm) was selected, as this was half the sum of the 5-mm radius of the burr handpiece and the 3-mm radius of the burr tip. The UAM-to-RT distance was measured as the distance from the uncinate process to the drawn resection trajectory along the medial margin of the uncinate process. The resection trajectory to VA distance was also measured as the shortest distance from the line to the VA (Fig. 2).
A suitable resection trajectory leaving a 3-mm distance from the VA and a resection trajectory for safe decompression were also assessed. A circle with a 3-mm radius was drawn, with the VA in the center. A diagonal resection trajectory was drawn from the point where the circle meets the lateral margin of the uncinate process. The UAM-to-RT distance was measured using this trajectory, as described in the previous paragraph (Fig. 2).
Self-retractors are placed at the uncinate process tip according to the standard Smith-Robinson index level approach. A complete discectomy and endplate preparation were performed before UPR. The uncinate tip-to-burr distance was measured preoperatively using the abovementioned method to assess the proper resection trajectory. A 3-mm match head burr was used to thin down the uncinate process below the preoperatively determined distance from the uncinate process. A Kerrison punch was used to remove the paper-thin uncinate process to prevent nerve root injury. The pedicle borders were palpated with an angled probe to ensure adequate decompression. Interbody spacers were inserted after decompression completion, followed by anterior cervical plate application (Fig. 3).
All variables were tested for normality using the Shapiro-Wilk test. The Student t-test was used to compare two groups according to the presence of foraminal stenosis or uncinate degeneration. All statistical analyses were performed using IBM SPSS ver. 22.0 (IBM Corp., Armonk, NY, USA), with the significance level set at p<0.05.
ACDF was performed on 163 segments of 101 patients (65 men [64.4%]; age, 56.3±12.2 years). Partial UPR was performed bilaterally in 87 segments (53.4%) and unilaterally in 43 segments (26.4%). There were no VA or nerve root injuries observed as a result of the UPR. Arm pain Visual Analog Scale (preoperative, 8.0±1.6; 1 year postoperative, 1.2±2.6; p<0.001) improved significantly during the 1 year postoperative period. Furthermore, the Neck Disability Index at 1-year follow-up demonstrated significant improvement compared with the preoperative score (preoperative, 21.1±6.3; 1 year postoperative, 6.7±5.3; p<0.001).
When foraminal stenosis was present, the uncinate process anteroposterior length was significantly higher at all levels than in segments without foraminal stenosis. Other radiographic parameters, such as uncinate process height, thickness, vertical distance from the uncinate process base to VA, and horizontal distance from the uncinate process to VA, did not demonstrate a significant trend when foraminal stenosis was present (Tables 1, 2). Furthermore, there were no significant differences in uncinate process height, length, anteroposterior length, or horizontal/vertical distance from the uncinate process to the VA based on uncinate degeneration (Table 3).
The distances between the right and left uncinate process tips were 19.4±2.6 mm, 20.3±2.2 mm, 23.0±2.6 mm, and 26.3±2.1 mm for C3–C4, C4–C5, C5–C6, and C6–C7 levels, respectively, with an increasing trend from the proximal to distal level. The horizontal distances from the uncinate process to the VA were significantly higher at the C6–C7 levels than at the proximal levels (right, p<0.001; left, p<0.001).
The UAM-to-RT distances for adequate decompression to reach the pedicle were 1.6±1.4 mm (range, 0–4.8 mm), 3.4±1.7 mm (range, 0–7.1 mm), 4.0±1.7 mm (range, 0–9.0 mm), and 4.5±1.2 mm (range, 2.5–7.5 mm) for the C3–C4, C4–C5, C5–C6, and C6–C7 levels, respectively, with an increasing trend at the distal levels. This indicates that when considering the anteroposterior length of the uncinate process at each level, 87.0%, 71.5%, 67.3%, and 53.7% of the uncinate from the posterior margin should be removed for adequate decompression. The distances from the resection trajectory to the VA ranged from 3–4 mm at the C3–C6 levels but were significantly higher at the C6–C7 levels (7.4±1.5 mm, p<0.001). The UAM-to-RT for adequate decompression did not differ significantly due to foraminal stenosis or uncinate degeneration (Tables 4, 5).
The UAM-to-RT distances for leaving a 3-mm margin from the resection trajectory to the VA were 1.5±1.4 mm (range, 0–4.8 mm), 2.0±1.5 mm (range, 0–4.6 mm), and 2.5±1.7 mm (range, 0–6.6 mm) for the C3–C4, C4–C5, and C5–C6 levels, respectively. The UAM-to-RT distance at the C6–C7 level was not measured because the 3-mm-radius circle often did not meet the uncinate process due to the increased distance from the uncinate process to VA at this level. The UAM-to-RT for preventing VA injury risk did not differ significantly according the presence of foraminal stenosis or uncinate degeneration (Tables 4, 5). Because the UAM-to-RT distance in the C3–C5 levels ranged from 0–4.8 mm and 0–6.6 mm in the C6–C7 levels, a cutoff value of 5-mm was assumed. Eleven segments (5.4%) at the C5–C6 levels exceeded the boundary of 3-mm from the VA when leaving a 5-mm distance from the uncinate tip to the resection trajectory; however, no violation occurred at the C3–C4 and C4–C5 levels.
The present study demonstrated that foraminal stenosis or uncinate degeneration had no effect on the relative anatomy of the uncinate process and VA, indicating that there is no change in the risk of VA injury. Furthermore, resection of the anterior portion of the uncinate process was required for adequate foraminal decompression at the proximal level. The necessary UAM-to-RT distances to leave a 3-mm distance from the VA were 1.5, 2.0, and 2.5 mm at the C3–C4, C4–C5, and C5–C6 levels, respectively, and these increased in the distal levels. Maintaining the resection trajectory 5-mm from the uncinate tip was generally safe, resulting in no violation of the 3-mm boundary from the VA at the C3–C4 and C4–C5 levels and a 5.4% violation at the C5–C6 level. The UPR at the C6–C7 level was anatomically safer because of the increased distance of the VA from the uncinate process at this level.
Anterior cervical discectomy and fusion is traditionally considered to provide both direct and indirect decompression [2,3]. Foraminal stenosis by uncinate hypertrophy can be treated with indirect decompression to restore the disk height [3]. Shen et al. [3] reported that a 2-mm distraction of the disk space resulting in indirect decompression was associated with clinical outcomes comparable with direct decompression. Abudouaini et al. [14] found that additional direct decompression by UPR did not result in greater clinical benefit than that of ACDF alone. However, recent studies have shown that indirect decompression without UPR during ACDF has limitations. Lee et al. [6] reported that although the late clinical results of ACDF alone and ACDF with UPR were identical, the ACDF with UPR group demonstrated faster clinical improvement and significantly better early postoperative arm pain. A meta-analysis also concluded that while ACDF with UPR requires longer operation time and is associated with increased blood loss, it has the additional benefit of improving early postoperative arm pain [9]. Furthermore, the decrease of segmental height commonly occurring after indirect decompression with ACDF may result in late deterioration [23]. Therefore, while ACDF alone could still provide clinical improvement for cervical radiculopathy, additional UPR appears to provide the benefits of faster and more significant pain relief [8,9]. This is especially true when uncinate hypertrophy, rather than soft disk herniation, is the main pathology and the degree of severe foraminal stenosis [9]. Sun et al. [4,24] showed that when the preoperative intervertebral foraminal width was <3 mm, additional UPR provided significantly greater improvement in clinical symptoms. Nevertheless, although the safety of UPR has been demonstrated by its low rate of complications, it still increases the risk of VA injury and is technically demanding compared with ACDF alone; therefore, this technique warrants special care and thorough preoperative planning [9].
Although previous studies have demonstrated the efficacy of UPR, several questions remain regarding UPR. First, it is unclear which surgical technique, such as total uncinate removal or partial posterior UPR, is the optimal decompression method [16]. Because the anterior border of the foramen is completely removed, total uncinate removal must result in complete foraminal decompression [8,10,25,26]. However, more extensive lateral dissection is required, and the risk of VA injury increases as the lateral cortex of the uncinate process is removed. Partial posterior UPR is less technically challenging because it does not require access lateral to the uncinate process, but it does carry the possibility of incomplete decompression [14,15]. Second, the amount of resection required for adequate decompression while preventing VA injury during partial posterior UPR is unknown. Moreover, the amount of decompression required cannot be easily determined intraoperatively. Because excessive resection involving the anterior and lateral portions of the uncinate process can damage the VA, partial UPR is not free from the risk of VA injury. The main goal of the present study was to determine how surgeons should plan an adequate resection trajectory while performing partial posterior UPR.
In the present study, we used the UAM-to-RT distance to guide the amount of uncinate resection. We believe that this is more easily identified intraoperatively than other indicators, such as instrument angulation or distance from the uncinate base. Surgeons may use the diameters of surgical instruments, such as the burr tip, as reliable references to measure the distance from the resection trajectory to the uncinate process tip. The UAM-to-RT distance required for adequate decompression was 1.6-mm at C3–C4 and gradually increased at each distal level. This increasing trend could be attributed to the increased horizontal distance between uncinate processes at more distal levels [22]. We assumed that self-retractors are placed at the uncinate process, limiting the angulation of the surgical instruments; therefore, fewer angulations would be possible at proximal levels, and greater anterior bone removal would be required for sufficient bone resection at the posterior uncinate. Furthermore, considering that the anteroposterior length of the uncinate process is approximately 10-mm, a significant portion of the anterior part of the uncinate process should be resected to provide adequate decompression to reach the margin of the pedicle. While several previous studies have described surgical techniques that involve resecting only the posterior portion of the uncinate, the present study suggests that such techniques have a high risk of resulting in incomplete decompression because the extent of uncinate resection could not reach the foramen exit zone due to the limited angulation of surgical instruments [14,15].
VA injury is one of the most feared complications during UPR [17,25]. The present study demonstrated that maintaining the UAM-to-RT distance above 5-mm could maintain the distance between the VA and resection trajectory above 3-mm in most cases. Furthermore, because the UAM-to-RT for adequate decompression was similar to or greater than the UAM-to-RT for avoiding VA injury at all levels, adequate decompression with partial posterior UPR could be considered generally safe. However, individual preoperative assessment is required because more anterior resection of the uncinate may be required for adequate decompression in some cases and because the course of VA is highly varied. For example, radiographic simulations using axial CT angiography, as demonstrated in the present study, would be beneficial (Figs. 2, 3). Caution is particularly needed at the C5–C6 level because the distance between uncinate and VA is smaller than that at the C6–C7 level. Moreover, the resection trajectory with a UAM-to-RT of 5-mm violated the boundary of 3-mm from the VA in 5.4% of cases.
The anteroposterior length of the uncinate process was significantly longer when foraminal stenosis was present. However, this difference is inherent in the definition of foraminal stenosis because posterior growth of the uncinate process causes foramen narrowing [24]. Other than anteroposterior length, no other radiographic parameters of the uncinate process and VA showed any significant differences according to the presence of foraminal stenosis. This demonstrates that foraminal stenosis does not alter the relative anatomy of the uncinate process and VA; thus, the risk of VA injury is not increased with foraminal stenosis. Furthermore, due to uncinate degeneration, the uncinate process height, thickness, and relative anatomy with VA were not significantly different. This finding was unexpected, as we had assumed that uncinate degeneration increased the risk of uncinate hypertrophy, which would increase the thickness or decrease the distance between the uncinate process and VA [24]. This lack of intergroup difference could be attributed to the specifics of the classification system used for uncinate degeneration [21]. The uncinate degeneration classification system is typically divided by osteophyte formation at the uncovertebral joint and mimics the Lawrence-Kellgren classification commonly used for knee osteoarthritis [21]. However, osteophytes are most commonly developed at the superior portion of the uncinate process, which articulates with the cranial vertebra, and the specifics of the anatomy at the base of the uncinate process, where foraminal decompression is performed, may not be reflected in this system [21]. Nevertheless, we were unable to identify a proper classification system for uncinate process degeneration that represented the characteristics of uncinate process anatomy; therefore, this warrants further evaluation.
The present study has some limitations. First, the radiographic simulation was based on multiple self-retractor positions and burr size assumptions. While these assumptions are not distinct from typical operative situations, they may not be applicable in all cases. However, our results can be used as a general guideline and to assist in preoperative planning. Second, because we focused on the technical aspects and anatomy of partial UPR, the efficacy of partial UPR for foraminal decompression was not evaluated. In the present cohort, this was impossible because we routinely performed partial UPR on segments with foraminal stenosis. Nevertheless, the potential benefit of direct foraminal decompression has been well described in previous studies [6,7,9,13,27]. Finally, this study was conducted in a nation dominated with a single race. Therefore, these measurements may differ in other countries with diverse ethnic populations.
In conclusion, the UAM-to-RT distance could be used in preoperative planning and during surgery to determine the degree of partial UPR. Maintaining a UAM-to-RT distance of >5 mm should generally provide safe decompression without the risk of VA injury. Foraminal stenosis or uncinate degeneration did not distort the relative anatomy of the uncinate process and the VA and did not change the risk of VA injury. While the results of the present study could be used as a general guide, individual assessment and preoperative planning are still important because of the highly variable course of VA.
Fig. 1
Radiographic assessment. (A) Radiographic assessment on coronal computed tomography (CT). a)Uncinate process height was measured as distance from the line drawn along the upper endplate of the vertebral body and tip of the uncinate process. b)Uncinate process thickness was measured as the distance between the medial and lateral borders of uncinate process at the plane of upper endplate. (B) Radiographic assessment on axial CT. c)Anteroposterior length of uncinate process was measured as vertical distance between anterior and posterior borders of uncinate process. d)Horizontal distance from lateral border of uncinate process to vertebral artery. e)Vertical distance from baseline plane of uncinate process to VA. f)Horizontal distance between the right and left tips of the uncinate process.

Fig. 2
Radiographic simulation of resection trajectory (RT). (A) To simulate decompression sufficient to reach pedicle laterally, a point that corresponds to the superior border of pedicle was found (black spot). (B) Axial image was changed to the one visualizing the uncinate process. Referencing the point previously found, as described in (A), a point of uncinate process lateral margin that reaches the upper border of pedicle was again marked (black spot). A line simulating the 40-mm self-retractors were also drawn (blue lines). Next, a line was drawn diagonally (white dashed line) to a point where distance from the line and superior end of contralateral self-retractor was 4 mm (green line). A margin of 4 mm (2.5 mm+1.5 mm) was selected, as this was half the sum of the 5-mm radius of the burr handpiece (yellow line) and the 3-mm burr tip radius (red line). Uncinate anterior margin-to-resection trajectory (UAM-to-RT) was measured as the length from the uncinate process to the drawn RT along the medial margin of uncinate process (orange line). Resection trajectory-to-vertebral artery (RT-to-VA) distance was measured as the shortest distance from the line to the VA. (C) To simulate safe decompression keeping a 3-mm distance between the RT and VA, a 3-mm circle with the center being the VA was drawn. A point where lateral margin of uncinate process meets the 3-mm-radius circle was marked (black spot). With this reference point, UAM-to-RT distance was again assessed with the same method described in the legend of (B).
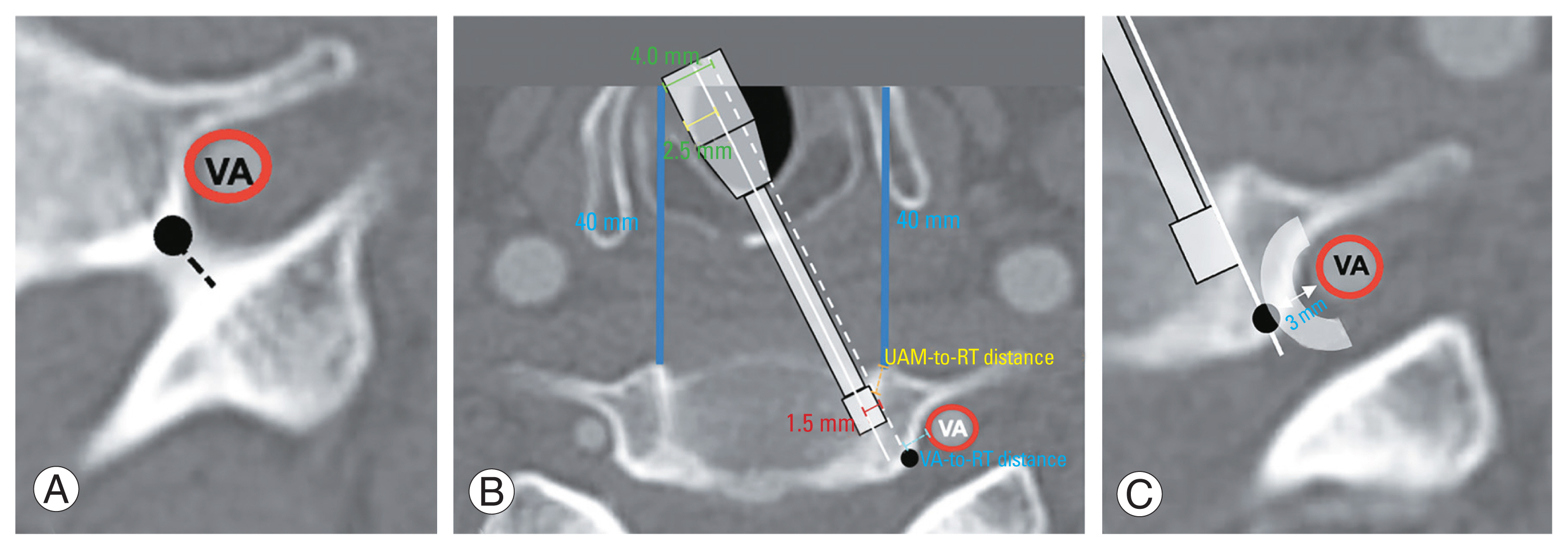
Fig. 3
Illustrative case. A 56-year-old female presented with bilateral arm pain that did not respond to conservative management for 4 months. (A) Axial magnetic resonance imaging of C5–6 demonstrated bilateral foraminal stenosis (arrows). Left side foraminal stenosis of C6–7 was also noted. After the diagnosis of cervical radiculopathy, anterior cervical discectomy and fusion combined with uncinate process partial resection was planned. (B) After drawing the location of vertebral artery (red circle), pedicle (black circle), and self-retractors (blue lines), resection trajectories (white dashed lines) were planned with simulation method demonstrated in Fig. 2. Uncinate anterior margin-to-resection trajectory distances (black lines) were preoperative measured. (C) Anterior cervical discectomy and fusion of C5–7 were performed. (D) Axial computed tomography image demonstrates that resection was performed as planned (white lines), and that successful bilateral foraminal decompression was achieved (arrows).
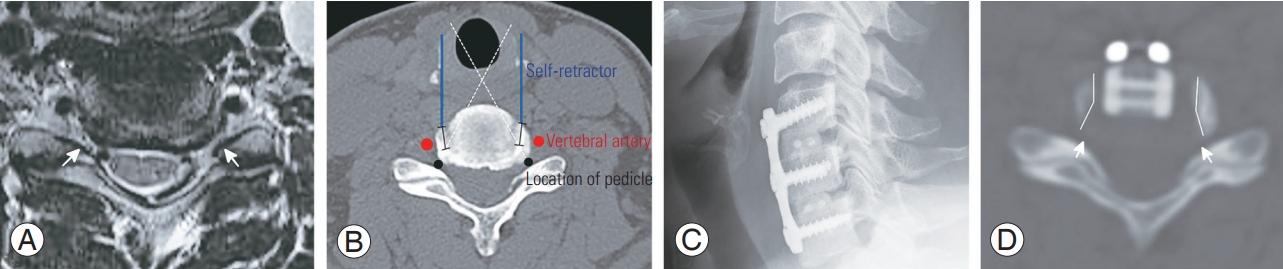
Table 1
Assessment of foraminal stenosis and uncinate degeneration at each level
Table 2
Radiographic measurement of uncinate process and vertebral artery according to foraminal stenosis
| Variable | Category | Right | Left | ||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| No foraminal stenosis | Foraminal stenosis | p-value | No foraminal stenosis | Foraminal stenosis | p-value | ||
| C3–4 | Uncinate height | 5.3±0.9 | 5.9±1.0 | 0.013* | 5.5±1.0 | 6.0±1.0 | 0.044* |
|
|
|||||||
| Uncinate thickness | 5.1±1.0 | 5.3±1.2 | 0.614 | 5.0±1.1 | 5.4±1.1 | 0.221 | |
|
|
|||||||
| Anteroposterior length | 11.6±1.6 | 12.8±2.0 | 0.008* | 11.6±1.6 | 12.5±1.8 | 0.049* | |
|
|
|||||||
| Uncinate base to vertebral artery | 3.8±1.6 | 5.0±1.6 | 0.007* | 3.4±1.3 | 4.4±1.5 | 0.012* | |
|
|
|||||||
| Uncinate to vertebral artery | 1.6±0.5 | 1.5±0.3 | 0.292 | 1.6±0.5 | 1.3±0.5 | 0.041* | |
|
|
|||||||
| C4–5 | Uncinate height | 5.5±0.9 | 5.9±1.3 | 0.084 | 5.6±1.1 | 6.2±1.3 | 0.083 |
|
|
|||||||
| Uncinate thickness | 5.2±1.0 | 5.3±1.4 | 0.918 | 5.1±1.2 | 5.2±0.9 | 0.759 | |
|
|
|||||||
| Anteroposterior length | 11.3±1.7 | 13.2±2.2 | <0.001* | 11.3±1.6 | 13.6±2.3 | <0.001* | |
|
|
|||||||
| Uncinate base to vertebral artery | 3.7±2.0 | 4.4±1.0 | 0.142 | 3.3±1.4 | 4.3±1.2 | 0.012* | |
|
|
|||||||
| Uncinate to vertebral artery | 1.5±0.6 | 1.3±0.4 | 0.778 | 1.4±0.5 | 1.5±0.8 | 0.663 | |
|
|
|||||||
| C5–6 | Uncinate height | 5.8±1.1 | 5.7±1.3 | 0.824 | 5.6±1.0 | 5.8±1.0 | 0.373 |
|
|
|||||||
| Uncinate thickness | 5.3±0.9 | 5.4±1.4 | 0.752 | 5.0±1.1 | 5.3±1.2 | 0.275 | |
|
|
|||||||
| Anteroposterior length | 11.4±1.9 | 13.0±2.7 | 0.013* | 10.9±1.7 | 12.9±2.7 | 0.001* | |
|
|
|||||||
| Uncinate base to vertebral artery | 4.5±3.0 | 4.7±2.0 | 0.768 | 4.1±3.2 | 4.6±1.8 | 0.404 | |
|
|
|||||||
| Uncinate to vertebral artery | 1.5±0.5 | 1.5±0.5 | 0.895 | 1.6±1.3 | 1.4±0.6 | 0.506 | |
|
|
|||||||
| C6–7 | Uncinate height | 5.4±1.0 | 5.8±1.2 | 0.134 | 5.8±1.2 | 5.5±1.2 | 0.398 |
|
|
|||||||
| Uncinate thickness | 5.4±1.3 | 5.6±1.2 | 0.490 | 5.4±1.2 | 5.9±1.3 | 0.110 | |
|
|
|||||||
| Anteroposterior length | 8.9±1.9 | 11.0±2.1 | <0.001* | 9.0±1.7 | 10.9±2.1 | <0.001* | |
|
|
|||||||
| Uncinate base to vertebral artery | 6.6±3.3 | 7.2±1.8 | 0.432 | 5.8±2.7 | 6.3±2.1 | 0.472 | |
|
|
|||||||
| Uncinate to vertebral artery | 3.0±1.3 | 3.0±2.0 | 0.984 | 2.8±1.4 | 2.2±1.1 | 0.079 | |
Table 3
Radiographic measurement of uncinate process and vertebral artery according to uncinate degeneration
| Variable | Category | Right | Left | ||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| No uncinate degeneration | Uncinate degeneration | p-value | No uncinate degeneration | Uncinate degeneration | p-value | ||
| C3–4 | Uncinate height | 5.4±0.9 | 6.5±0.8 | 0.013* | 5.6±1.0 | 6.2±1.5 | 0.327 |
|
|
|||||||
| Uncinate thickness | 5.2±1.1 | 5.5±0.6 | 0.552 | 5.1±1.1 | 4.9±0.4 | 0.758 | |
|
|
|||||||
| Anteroposterior length | 12.0±1.7 | 12.1±2.8 | 0.929 | 11.9±1.7 | 11.9±2.2 | 0.969 | |
|
|
|||||||
| Uncinate base to vertebral artery | 4.5±1.5 | 5.1±1.5 | 0.210 | 4.6±1.3 | 4.8±1.5 | 0.854 | |
|
|
|||||||
| Uncinate to vertebral artery | 1.5±0.5 | 1.7±0.3 | 0.623 | 1.5±0.5 | 1.8±0.8 | 0.175 | |
|
|
|||||||
| C4–5 | Uncinate height | 5.6±0.9 | 5.9±1.8 | 0.332 | 5.7±1.0 | 6.4±2.0 | 0.138 |
|
|
|||||||
| Uncinate thickness | 5.2±1.2 | 5.2±1.1 | 0.875 | 5.1±1.2 | 4.9±0.6 | 0.653 | |
|
|
|||||||
| Anteroposterior length | 11.9±2.1 | 12.8±2.1 | 0.191 | 11.8±2.1 | 13.0±1.4 | 0.171 | |
|
|
|||||||
| Uncinate base to vertebral artery | 3.8±1.8 | 4.8±0.9 | 0.075 | 3.4±1.4 | 4.7±1.4 | 0.029* | |
|
|
|||||||
| Uncinate to vertebral artery | 1.5±0.5 | 1.9±0.7 | 0.083 | 1.4±0.6 | 1.3±0.2 | 0.541 | |
|
|
|||||||
| C5–6 | Uncinate height | 5.7±1.1 | 6.0±1.5 | 0.290 | 5.6±1.0 | 6.0±1.1 | 0.150 |
|
|
|||||||
| Uncinate thickness | 5.4±1.0 | 5.3±1.7 | 0.697 | 5.2±1.2 | 5.1±1.1 | 0.513 | |
|
|
|||||||
| Anteroposterior length | 12.2±2.7 | 12.7±2.1 | 0.472 | 11.7±2.6 | 12.8±2.1 | 0.121 | |
|
|
|||||||
| Uncinate base to vertebral artery | 4.6±2.5 | 4.6±2.3 | 0.941 | 4.4±2.7 | 4.3±2.1 | 0.949 | |
|
|
|||||||
| Uncinate to vertebral artery | 1.4±0.4 | 1.6±0.5 | 0.120 | 1.5±1.1 | 1.5±0.6 | 0.798 | |
|
|
|||||||
| C6–7 | Uncinate height | 5.5±0.8 | 6.1±1.6 | 0.073 | 5.7±1.1 | 5.4±1.5 | 0.320 |
|
|
|||||||
| Uncinate thickness | 5.4±1.2 | 5.8±1.4 | 0.269 | 5.7±1.3 | 5.6±1.3 | 0.874 | |
|
|
|||||||
| Anteroposterior length | 9.7±2.2 | 11.4±1.8 | 0.010* | 9.8±2.2 | 10.9±1.7 | 0.127 | |
|
|
|||||||
| Uncinate base to vertebral artery | 7.0±2.7 | 6.8±2.2 | 0.785 | 5.8±2.5 | 7.2±2.3 | 0.104 | |
|
|
|||||||
| Uncinate to vertebral artery | 3.2±1.7 | 2.5±0.9 | 0.149 | 2.5±1.3 | 2.4±0.9 | 0.849 | |
Table 4
Radiographic simulation of uncinate process resection according to foraminal stenosis
Table 5
Radiographic simulation of uncinate process resection according to uncinate degeneration
| Variable | Category | Right | Left | ||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| No uncinate degeneration | Uncinate degeneration | p-value | No uncinate degeneration | Uncinate degeneration | p-value | ||
| C3–4 | UAM-to-RT distance (for enough decompression) | 1.6±1.3 | 1.9±2.1 | 0.772 | 1.5±0.7 | 1.6±0.8 | 0.701 |
|
|
|||||||
| Resection trajectory to vertebral artery | 3.2±0.8 | 3.3±0.7 | 0.913 | 3.3±0.7 | 3.1±0.9 | 0.427 | |
|
|
|||||||
| UAM-to-RT distance (for avoiding vertebral artery) | 1.7±1.3 | 1.6±1.0 | 0.552 | 1.3±1.3 | 1.3±0.8 | 0.902 | |
|
|
|||||||
| C4–5 | UAM-to-RT distance (for enough decompression) | 3.5±1.7 | 3.6±0.8 | 0.237 | 3.2±1.1 | 3.5±1.4 | 0.507 |
|
|
|||||||
| Resection trajectory to vertebral artery | 3.5±0.9 | 3.9±1.3 | 0.183 | 3.2±1.0 | 3.5±2.1 | 0.371 | |
|
|
|||||||
| UAM-to-RT distance (for avoiding vertebral artery) | 1.9±1.5 | 1.8±1.6 | 0.892 | 2.1±1.2 | 2.1±0.8 | 0.879 | |
|
|
|||||||
| C5–6 | UAM-to-RT distance (for enough decompression) | 3.9±1.0 | 4.3±1.8 | 0.304 | 3.9±1.6 | 4.2±1.4 | 0.412 |
|
|
|||||||
| Resection trajectory to vertebral artery | 3.8±1.2 | 4.2±2.2 | 0.408 | 3.8±1.1 | 3.5±0.4 | 0.165 | |
|
|
|||||||
| UAM-to-RT distance (for avoiding vertebral artery) | 2.6±.8 | 2.4±1.5 | 0.435 | 2.4±1.7 | 2.6±0.6 | 0.770 | |
|
|
|||||||
| C6–7 | UAM-to-RT distance (for enough decompression) | 4.2±0.9 | 4.9±1.2 | 0.019* | 4.6±1.2 | 4.4±0.9 | 0.137 |
|
|
|||||||
| Resection trajectory to vertebral artery | 7.7±1.9 | 7.1±1.4 | 0.494 | 7.4±1.7 | 7.2±1.6 | 0.592 | |
|
|
|||||||
| UAM-to-RT distance (for avoiding vertebral artery) | NA | NA | NA | NA | NA | NA | |
References
1. Kang KC, Jang TS, Jung CH. Cervical radiculopathy: focus on factors for better surgical outcomes and operative techniques. Asian Spine J 2022;16:995–1012.




2. Sharma JK, Varma KK, Mallepally AR, et al. Two-level anterior cervical discectomy and fusion versus hybrid total disc replacement for bilevel pathology with cervical radiculopathy/myelopathy: a comparative study with a minimum 2-year follow-up in an Indian population. Asian Spine J 2022;16:493–501.




3. Shen FH, Samartzis D, Khanna N, Goldberg EJ, An HS. Comparison of clinical and radiographic outcome in instrumented anterior cervical discectomy and fusion with or without direct uncovertebral joint decompression. Spine J 2004;4:629–35.


4. Sun B, Xu C, Zhang Y, et al. Intervertebral foramen width is an important factor in deciding additional uncinate process resection in ACDF: a retrospective study. Front Surg 2021;8:626344.



5. Lawless MH, Yoon EJ, Jasinski JM, et al. Impact of interspace distraction on fusion and clinical outcomes in anterior cervical discectomy and fusion: a longitudinal cohort study. Asian Spine J 2022;16:369–74.




6. Lee DH, Cho JH, Baik JM, et al. Does additional uncinate resection increase pseudarthrosis following anterior cervical discectomy and fusion? Spine (Phila Pa 1976) 2018;43:97–104.


7. Safaee MM, Nichols NM, Yerneni K, Zhang Y, Riew KD, Tan LA. Safety and efficacy of direct nerve root decompression via anterior cervical discectomy and fusion with uncinectomy for cervical radiculopathy. J Spine Surg 2020;6:205–9.



8. Mella P, Suk KS, Kim HS, et al. ACDF with total en bloc resection of uncinate in foraminal stenosis of the cervical spine: comparison with conventional ACDF. Clin Spine Surg 2021;34:E237–42.

9. Yin M, Ding X, Zhu Y, et al. Safety and efficacy of anterior cervical discectomy and fusion with uncinate process resection: a systematic review and meta-analysis. Global Spine J 2022;12:1956–67.




10. Tan LA, Riew KD. Anterior cervical foraminotomy: 2-dimensional operative video. Oper Neurosurg (Hagerstown) 2018;15:E66.


11. Clifton W, Williams D, Pichelmann M. How I do it: total uncinatectomy during anterior diskectomy and fusion for cervical radiculopathy caused by uncovertebral joint hypertrophy. Acta Neurochir (Wien) 2019;161:2229–32.



12. Pakzaban P. Ultrasonic total uncinectomy: a novel technique for complete anterior decompression of cervical nerve roots. Neurosurgery 2014;10(Suppl 4): 535–41.

13. Lee BH, Park JH, Lee JY, Jeon HJ, Park SW. Efficiency of minimal oblique resection of the uncinate process during an anterior cervical discectomy and fusion. Medicine (Baltimore) 2021;100:e26790.



14. Abudouaini H, Wu T, Liu H, et al. Partial uncinatectomy combined with anterior cervical discectomy and fusion for the treatment of one-level cervical radiculopathy: analysis of clinical efficacy and sagittal alignment. BMC Musculoskelet Disord 2021;22:777.




15. Guo Q, Wang L, Zhang B, et al. Standalone anterior cervical discectomy and fusion versus combination with foraminotomy for the treatment of cervical spondylotic radiculopathy secondary to bony foraminal stenosis. World Neurosurg 2016;95:134–42.


16. Guo W, Jiang Y, Zhu Y, Huang J. Effect of ACDF combined with different degrees of partial resection of uncovertebral joints on cervical stability and degeneration: a three-dimensional finite element analysis. J Orthop Surg Res 2022;17:551.




17. Gitkind AI, Olson TR, Downie SA. Vertebral artery anatomical variations as they relate to cervical transforaminal epidural steroid injections. Pain Med 2014;15:1109–14.


18. Kim GU, Park WT, Chang MC, Lee GW. Diagnostic technology for spine pathology. Asian Spine J 2022;16:764–75.




19. Park HJ, Kim SS, Han CH, et al. The clinical correlation of a new practical MRI method for grading cervical neural foraminal stenosis based on oblique sagittal images. AJR Am J Roentgenol 2014;203:412–7.


20. Meacock J, Schramm M, Selvanathan S, et al. Systematic review of radiological cervical foraminal grading systems. Neuroradiology 2021;63:305–16.



21. Huang T, Qin J, Zhong W, Tang K, Quan Z. The CT assessment of uncovertebral joints degeneration in a healthy population. Eur J Med Res 2021;26:145.




22. Cui S, Nasser AE, Ma L, Su P, Su D, Liao Z. Analysis of the morphometric change in the uncinate process of the cervical spondylosis patients: a study of radiological anatomy. J Orthop Translat 2020;24:32–8.



23. Yang JJ, Park S, Kim HJ, Yoon JY. Segmental height decrease adversely affects foraminal height and cervical lordosis, but not clinical outcome after anterior cervical discectomy and fusion using allografts. World Neurosurg 2021;154:e555–65.


24. Sun B, Xu C, Qi M, et al. Predictive effect of intervertebral foramen width on pain relief after ACDF for the treatment of cervical radiculopathy. Global Spine J 2023;13:133–9.




25. Valero-Moreno F, Clifton W, Damon A, Pichelmann M. Total anterior uncinatectomy during anterior discectomy and fusion for recurrent cervical radiculopathy: a two-dimensional operative video and technical report. Cureus 2020;12:e7466.



- TOOLS







