 |
 |
- Search
| Asian Spine J > Volume 17(6); 2023 > Article |
|
Abstract
Purpose
To analyze the results and effectiveness of percutaneous screws (PS) with midline microscopic transforaminal decompression (MTFD) technique in reducing adult stiff lytic high-grade spondylolisthesis (HGSL) and compare it with the conventional technique.
Overview of Literature
Pedicle screw cannulation and segmental kyphosis negotiation are surgical challenges in HGSL. Open reduction is the preferred approach. PS have the advantage of optimized trajectory and minimized soft tissue exposure. The role of minimally invasive surgery in HGSL remains unknown. We propose a hybrid technique combining PS with MTFD for lytic HGSL.
Methods
This study included 25 patients with adult lytic HGSL (Meyerding grade III and IV) operated using a hybrid technique from 2012 to 2015. Data were compared with retrospective data on conventional open reduction (n=23) operated from 2000 to 2015. The minimum follow-up was 5 years. Clinical outcomes were assessed using the Visual Analog Scale (VAS) score and modified Oswestry Disability Index (m-ODI). The spinopelvic and perioperative parameters were recorded. The inter-body fusion and adjacent segment degeneration (ASD) were assessed on radiographs at the final follow-up.
Results
The average age in the MTFD and open groups was 45.84┬▒12.70 years (nine males and 16 females) and 49.26┬▒13.33 years (eight males and 15 females), respectively. Further, 22 and three patients in the MTFD group and 19 and four in the open group had grade III and IV listhesis, respectively. The MTFD group demonstrated less operative time, blood loss, and hospital stays than the open group. Significant improvements were observed in VAS and m-ODI in subsequent follow-ups in both groups. The MTFD group fared better at 3 months but outcomes were comparable at the final follow-up. Both techniques were equally effective in restoring spinopelvic parameters. The incidence of ASD is comparable.
High-grade spondylolisthesis (HGSL) with a Meyerding grade of >II is a surgical predicament. Reduced contact surface for fusion, segmental kyphosis, and abnormal spinopelvic parameters are surgical concerns [1ŌĆō3]. A controlled slip reduction and kyphosis correction that restores spinopelvic anatomy is the standard surgical approach [4,5]. An open reduction and inter-body fusion remain the preferred treatment [6,7]. Advent percutaneous screws (PS) and micro-surgical approaches have helped minimize soft tissue injury, but their role in HGSL remains sparsely described in the literature [8,9]. The Authors describe a hybrid technique that combines PS insertion with the midline microscopic transforaminal decompression (MTFD) approach for controlled adult lytic HGSL reduction. This study aims to investigate the effectiveness of this technique in reducing listhesis and its clinic-radiological outcomes. Authors have used ŌĆ£MTFDŌĆØ as a hybrid technique for convenience of description.
This retrospective analysis included 25 adult patients with lytic HGSL (Meyerding grade III and IV) operated using a hybrid technique from 2012 to 2015. All clinical and radiological data were collected from the hospitalŌĆÖs medical record department. All patients presented with axial and leg pain (unilateral in 18 and bilateral in seven). Data were compared with available retrospective (unpublished) data on conventional open reduction (control group n=23) operated from 2000 to 2015. The minimum follow-up was 5 years. Mono-segment fixation was performed in all patients. A stiff lytic listhesis was included. This study excluded patients who had grade I or more reduction in listhesis on dynamic and supine radiographs, as well as a low-grade spondylolisthesis (I and II), congenital adolescent HGSL, and spondyloptosis. The Institutional Review Board approval was waived due to the retrospective design of the study. Written informed consent was obtained from the patients.
All patients of both groups underwent antero-posterior (AP), lateral (L), and dynamic flexion-extension lumbosacral spine radiographs preoperatively. Postoperative radiographs (AP and L) were followed at 3, 12, 24, and 60 months. The radiographs were evaluated by an independent radiologist blinded to the purpose of the study. Slip percentage, slip angle (SA), sacral slope (SS), pelvic tilt (PT), lumbar lordosis (LL), pelvic incidence, MeyerdingŌĆÖs grade change, implant mal-positioning, implant loosening, and loss of reduction/slip progression were recorded. The clinical outcomes were recorded using the Visual Analog Scale (VAS) score and modified Oswestry Disability Index (m-ODI). The preoperative VAS for leg and back pain was compared with 3, 12, 24, and 60 months postoperative. The m-ODI was measured pre- and postoperative at 3, 24, and 60 months. The inter-body fusion was assessed using Bridwell fusion criteria at the final follow-up [10]. Grades 1 and 2 fusion was considered acceptable. Operative parameters, such as surgical time (ST), blood loss (BL), radiation time (RT), and hospital stay, were documented. The adjacent segment degeneration (ASD) was assessed on standing radiographs at the final follow-up by an independent radiologist in both groups. A significant radiological ASD has been considered if the patient had any of the following signs: (1) Ōēź50% disk height reduction; (2) >3-mm anterior translation; and (3) >10┬░ angulation on sagittal and/or coronal plane [11].
The surgical technique combined PS insertion with midline MTFD. The patient was positioned prone under general anesthesia on a spinal frame with the abdomen free and partial extension of hips to improve reduction (sacral ante-version).
The entry point on the skin was selected as per the trajectory and morphology of the pedicle under the C-arm. The C-arm was angled cranio-caudally as per the kyphosis and vertebral rotation. A Jamshidi needle was used to cannulate each pedicle. The needle position was confirmed with AP and lateral images on C-arm. Guide wires for PS were inserted in the lytic and subjacent pedicles and anchored to the drapes. Neuro-navigation was used in the last five cases.
A 2ŌĆō2.5 cm midline incision was centered over the spinous processes. Multifidus was erased to expose the lower 1/3 of the cranial lamina to the upper edge of the inferior facet to expose the lytic defect. Caudally, the upper edge of the inferior lamina was defined. A micro-discectomy retractor was used. The medial blade was anchored on the spinous process of the lytic vertebra. The lateral blade exposed the facet and lytic defect. The spinous process with interspinous ligament was preserved. The inferior facet of the cranial vertebra was excised (Fig. 1). The medial and superior overhang of the superior facet of the caudal vertebra was recessed. The pars interarticularis has resected at the pars defect level, and the remaining part of the proximal pars is trimmed to the inferior border of the pedicle to visualize an exit root. The exiting and traversing roots were decompressed by ŌĆ£looking outŌĆØ through the foramen. The surgeon stood on the contra-lateral side during decompression, and the retractor was tilted laterally. This step allowed optimal exiting root decompression. The surgeon then stood on the ipsilateral side with the retractor tilted medially ŌĆ£looking intoŌĆØ the central canal. The disk was visualized across the midline after retracting the dura and traversing roots. The overhanging posterior margin of the caudal vertebra was recessed to define the margins of the disk. This allowed the disk shavers to negotiate the inferior angulation and avoid end-plate lytic vertebra perforation. A partial reduction was achieved after disk release and distraction using sequential shavers. The midline distractor was loosened to reduce skin tension. Only unilateral transforaminal decompression (UTFD) was preferred for patients in whom the listhesis was partially reduced after disk and soft tissue release. A bilateral transforaminal decompression (BTFD) was done when the listhesis remained unreduced even after disk release.
The disk space was packed with autologous local morselized bone graft (a part of the lamina, resected inferior facets, trimmed superior facet, and base of the spinous process). The morselized graft was measured in the syringe in each patient (Figs. 1, 2). A 4-degree lordotic inter-body cage was inserted. The exiting root decompression was re-inspected.
Certain degree of listhesis was reduced by facetectomy and disk space preparation. The screws were inserted over the guide wires for further reduction. The caudal screws were put in the reduction mode. An appropriate-sized stabilizing rod was fixed at the caudal screw and then rod reduction was achieved using a reduction device (Figs. 3, 4).
The author preferred the complete removal of the rattler for wide decompression of the exiting and traversing roots in the conventional group.
Quantitative data were analyzed using mean and standard deviation. Pre- and postoperative clinical and radiological outcomes were analyzed in each group using the Student paired t-test. An unpaired t-test was used to compare between groups. A p-value of <0.05 signifies statistical significance.
The average follow-ups were 5.76┬▒0.57 years and 5.77┬▒0.51 years and the average age was 45.84┬▒12.70 years (nine males and 16 females) and 49.26┬▒13.33 years (eight males and 15 females) in the MTFD and open groups, respectively. Further, 22 and three patients in the MTFD group and 19 and four patients in the open group had grades III and IV listhesis, respectively. Unilateral leg pain (ULP) and bilateral leg pain (BLP) were observed in 18 (17 with grade III and one with grade IV) and seven (five with grade III and two with grade IV) patients in the MTFD group and 14 (13 with grade III and one with grade IV) and nine (six with grade III and three with grade IV) patients in the open group, respectively. Moreover, 18 patients in the MTFD group required UTFD, of which 15 (14 with grade III and one with grade IV) had ULP and three (with grade III) had BLP. The remaining seven patients underwent BTFD, of which three (with grade III) had ULP and four (two with grade III and two with grade IV) had BLP. A demographic detail is listed in Table 1.
The mean ST and BL were 188.12┬▒15.78 minutes and 108.4┬▒23.61 mL in the MTFD group. This was significantly (p<0.05) higher in the open group (198.91┬▒18.33 minutes and 363.47┬▒72.65 mL). None of the patients in the MTFD group required blood transfusion perioperatively while six patients (26%) in the open group required transfusion. The mean RT was 84.72┬▒22.01 seconds in the MTFD group, which was significantly higher than in the open group (45.17┬▒5.93 seconds). RT was reduced in the last five patients in the MTFD group because of navigation (average 43 seconds). The ST (mean 211 minutes) increased in five patients in whom navigation was used.
Patients in both groups were mobilized on the next day of surgery. The Foley catheter was removed on postoperative day 2, and the patient was advised to self-void. The patient was discharged once comfortable. The hospital stay was lesser in the MTFD (3.36┬▒0.74 days) in the open groups (5.43┬▒1.47 days, p<0.05).
Postoperative VAS was significantly improved at 3 months in both groups (p<0.05). A significant difference was found in VAS for back pain between groups. An MTFD fared better. This significance was maintained for up to 1 year (p<0.05). The difference between groups became statistically insignificant at 2 and 5 years of follow-up (Table 2).
VAS for the leg was significantly improved in both groups at 3 months of follow-up. The improvement persisted till the final follow-up. No statistical difference was found between groups at each follow-up (Table 2).
The m-ODI significantly improved for both groups at 3 months. Disability was significantly lower in the MTFD than in the open group (p<0.05). This difference became insignificant at 2 and 5 years, but the MTFD group appeared better (Table 2).
Slip percentage (MTFD: 63.88%┬▒8.32% to 8.36%┬▒9.59%; open group: 65.16%┬▒9.16% to 8.25%┬▒9.96%, p<0.05) and SA (MTFD: 9.35┬░┬▒3.96┬░ kyphosis to 9.43┬░┬▒3.10┬░ lordosis; open group: 9.39┬░┬▒3.05┬░ kyphosis to 8.21┬░┬▒1.85┬░ lordosis, p<0.05) were significantly improved in both groups. In the MTFD group, a complete reduction was achieved in 15 patients with grade III and one with grade IV listhesis. The remaining nine (seven with grade III and two with grade IV) were reduced to grade I. A complete reduction was achieved in 13 of 23 patients (12 with grade III and one with grade IV) in the open group. An up-to-grade-I reduction was achieved in nine patients (seven with grade III and two with grade IV) and the remaining one with grade IV listhesis was reduced to grade II. A significant reduction of LL was reported in both groups after correction. No significant change was found in PT and SS even after the reduction (Table 3). The achieved reduction was maintained in both groups till the final follow-up except for one patient in the open group who had a loss of reduction at the 5-month follow-up due to pseudoarthrosis.
One patient in the MTFD group developed postoperative left extensor halluces longus weakness (Medical Research Council grade 3/5) that recovered to normal at the end of 3 months. One patient had center wound superficial necrosis which was cured with secondary healing. One patient in the open group had a dural leak which remained uneventful in follow-up. One had L5 root neuropraxia that partially recovered in follow-up (Table 4).
In the MTFD group, 19 patients (76%) had grade 1 (complete fusion) while six had grade 2 fusions and with no non-union or pseudo-arthrosis. In open group, 20 patients (86%) had complete fusion and two had grade 2. One patient had pseudoarthrosis with rod breakage and loss of reduction, which was revised at 5 months of follow-up (Table 4).
One patient in the MTFD and two in the open groups had significant ASD. One from the open group was asymptomatic, and the remaining two were symptomatic (Table 4).
High-grade slips (grades III/IV) pose a different set of clinical and radiological challenges as compared to low-grade slips. Open reduction is preferred for reduction. The technical challenges of cannulation of dysmorphic lytic pedicles, optimum disk preparation, and controlled reduction have been highlighted [12,13]. The screw trajectory is of paramount importance for maximum purchase which allows a mono-segmental reduction. Far lateral and proximal dissection would require negotiating kyphosis and medial angulation of lytic pedicles in the conventional approach. The advent of PS allows the selection of precise trajectory while avoiding excessive soft tissue dissection. Deep-seated lytic pedicles and segmental kyphosis make the delineation of pedicles difficult. Positioning the C-arm requires experience, and radiation was a concern. The use of neuro-navigation reduced radiation exposure in the present series (n=5), as shown by Tian et al. [14]. The mobility of the rattler helps to maneuver instruments during disk preparation. Overhang of the caudal vertebra and segmental kyphosis needs to be negotiated to introduce disk shavers in the index disk space. End-plate perforation is of concern, which reduces effective distraction and results in cage migration. This was not observed in our series. Optimal disk release across the midline improves segment mobility. This reduces the stress on screws. The disk release could be performed across the midline by ŌĆ£looking into the canalŌĆØ in MTFD. Out of 22 grade III slip, 17 improved to grade II after disk preparation, while one with grade IV slip was reduced to grade II. A restoration of foraminal height through a unilateral approach indirectly decompressed the contra-lateral exiting root [15ŌĆō17]. We also preferred UTFD (n=18) in MTFD. Of the 18 patients, three had BLP. UTFD approach reduced listhesis, restored foraminal height, and alleviated bilateral symptoms. A listhesis was stiff even after unilateral disk release in seven patients, in which BTFD was done to achieve reduction and reduce the stress on implants.
HGSL reduction improves spinopelvic alignment and correlates with better clinical outcomes [4,5,18]. A correction of slip percentage in this series (preoperative slipŌĆōpostoperative slip divided by preoperative slip├Ś100) is 87% in MTFD group and 85% in open group with mono-segment fixation. This is comparable to the reported literature [6,15,19]. It proves the effectiveness of the hybrid technique in reducing a high-grade slip.
Harvesting bone graft in the present technique was identical to the open surgery although through a micro-fenestration. En-mass resection of a portion of the lamina and the inferior facet provided adequate bone graft. The average bone graft harvested in UTFD was 3.27┬▒0.73 mL and in BTFD was 7.57┬▒0.90 mL. We have not used bone substitutes. The fusion rate is comparable to open techniques reported in the literature [4,20,21]. Microscopic decompression is advantageous in minimizing BL, infection, and exposure-related morbidity. MTFD group had lesser BL, OT, and hospital stays compared to open group in this series. The VAS and ODI favorably improved in both groups. The MTFD technique equally proved as effective in relieving radicular symptoms as the conventional technique.
The reported complication rate in literature after the conventional surgery was 10%ŌĆō29%, including deep wound infection, nerve root deficit, dural injury, pseudoarthrosis, and implant failure/malposition [3,4,22ŌĆō24]. Our series revealed similar incidences of early perioperative complications in both groups. The most concerning complication is L5 neuropraxia as described by Petraco et al. [25]. A wide and far lateral decompression of the nerve root before reduction would require to prevent stretch to the exiting root [2,3,12,26]. We could achieve a far lateral decompression of the exiting root (similar to open reduction) on the ipsilateral through TFD. Our series revealed that two patients had L5 root neuropraxia, one in each group. It happened on the ipsilateral side of the surgical decompression in MTFD. We have not reported a contra-lateral neurological deficit. Moreover, the portion of the skin between the screws and midline retractor needs careful attention in MTFD. One patient had central wound maceration in early experience. It was further prevented by lateralizing the skin incisions for screws and relaxing a midline retractor intermittently during surgery.
This series revealed that the incidence rate of significant ASD is comparable in both groups (MTFD group: 4%, open group: 8.69%). The benefit of minimally invasive surgery to reduce ASD remains unclear in the literature [27,28]. The midline dissection remained at the edges of laminotomy, without violating the adjacent segment during decompression in the hybrid technique; henceforth, authors preferred the term ŌĆ£contained midline decompression.ŌĆØ At present, concluding the role of the current technique to reduce ASD was difficult for authors. A larger study would be required.
This study had a few limitations. All surgeries were performed by a single senior surgeon. This creates a bias about the learning curve. The learning curve may get shortened for the surgeons familiar with the midline approach. The authors have not experienced other minimally invasive techniques. Rajakumar et al. [15] and Quraishi et al. [29] have described the feasibility and effectiveness of the tubular system for HGSL reduction. All patients involved in this series had stiff lytic HGSL with a less severe lumbopelvic deformity, vertebral remodeling, and rigidity compared to dysplastic listhesis. However, the author has started using this technique in dysplastic listhesis which is not a part of this study.
A hybrid technique is effective to reduce HGSL, with outcomes similar to the conventional approach. It combines the benefits of limiting soft tissue dissection by microscopic decompression and optimal screw trajectory using PS. It has lesser OT, BL, and hospital stay than the conventional approach. Long-term clinical and radiological outcomes are favorable.
Notes
AuthorsŌĆÖ Contributions
Conception and design: BKP, MRB, AG; data acquisition and analysis of data: BKP; drafting a manuscript: BKP, MRB; manuscript review & editing: BKP, MRB, AG; critical revision: BKP; administrative support: MRB; supervision: MRB, AG; and final approval of the manuscript: all authors.
Fig.┬Ā1
(A, B) Images showed complete reduction of grade-IV listhesis. (C) Computed tomography scan showed complete inter-body fusion. (D) Images showed resected en-mass inferior facet (black arrow), measured bone graft in syringe, and cage filled with bone paste (white arrow). SS, sacral slope; PT, pelvic tilt; LL, lumbar lordosis; SA, slip angle; K, kyphosis; L, lordosis.

Fig.┬Ā2
Grade-III spondylolisthesis (A, B) was reduced up-to grade-I (C). (D) Image showed measured bone graft volume in bilateral transforaminal decompression. SS, sacral slope; PT, pelvic tilt; LL, lumbar lordosis; SA, slip angle; K, kyphosis; L, lordosis; Erect LAT, erect lateral view.
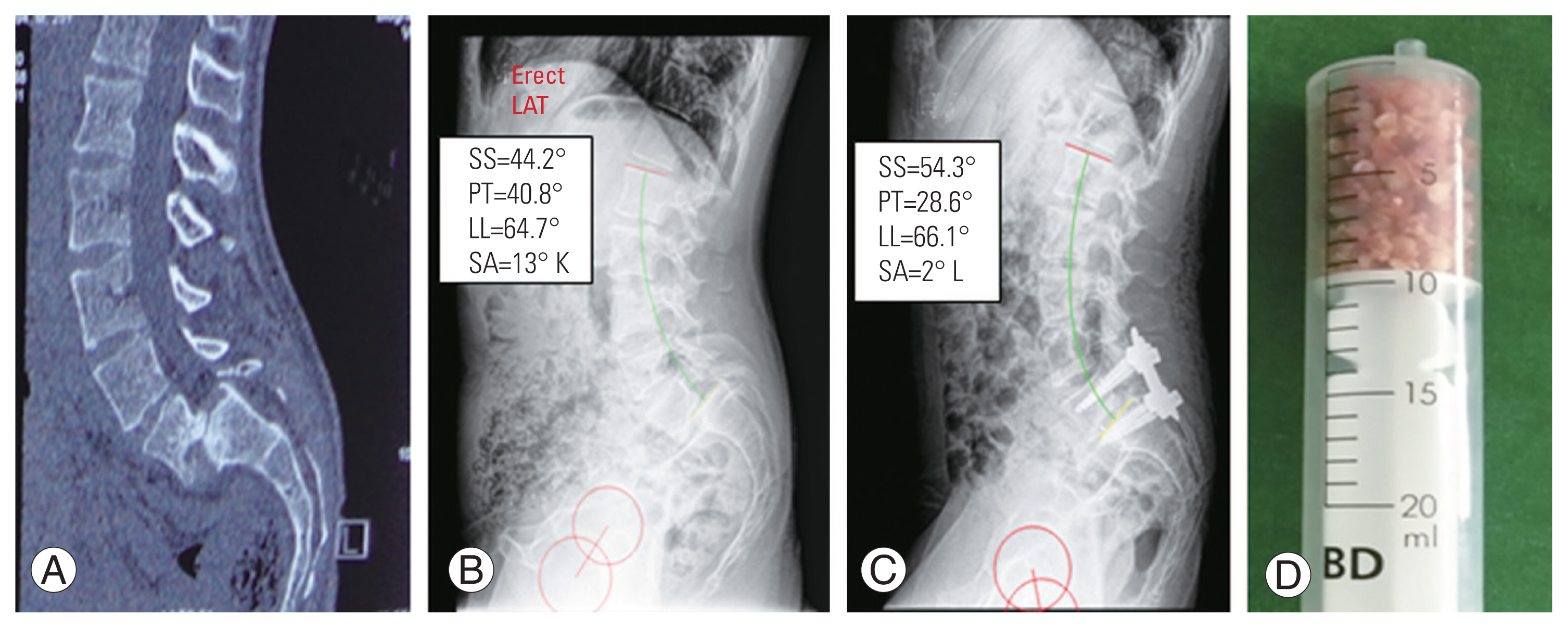
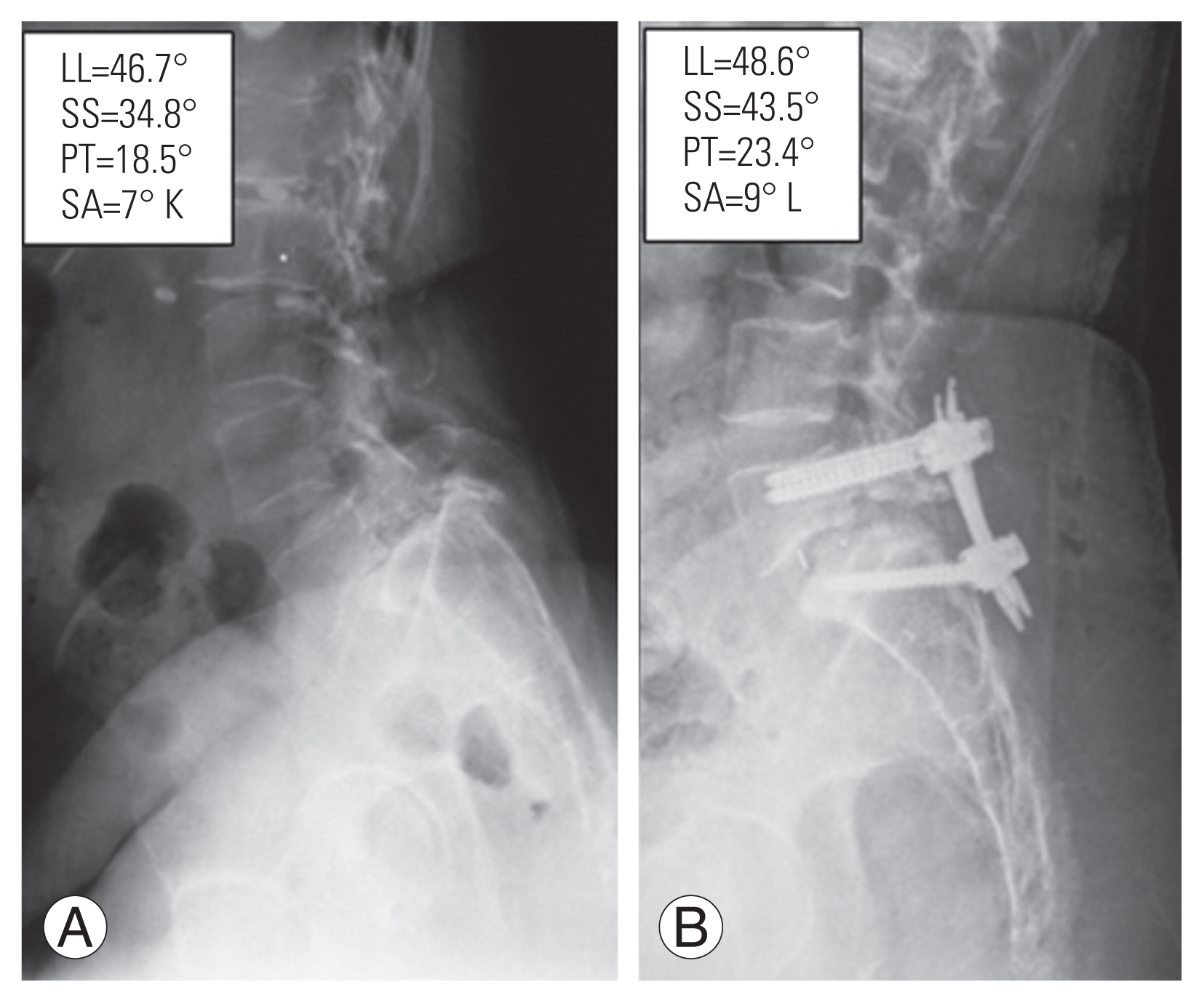
Fig.┬Ā3
Grade-IV spondylolisthesis (A) was reduced up-to grade-I (B). SS, sacral slope; PT, pelvic tilt; LL, lumbar lordosis; SA, slip angle; K, kyphosis; L, lordosis.
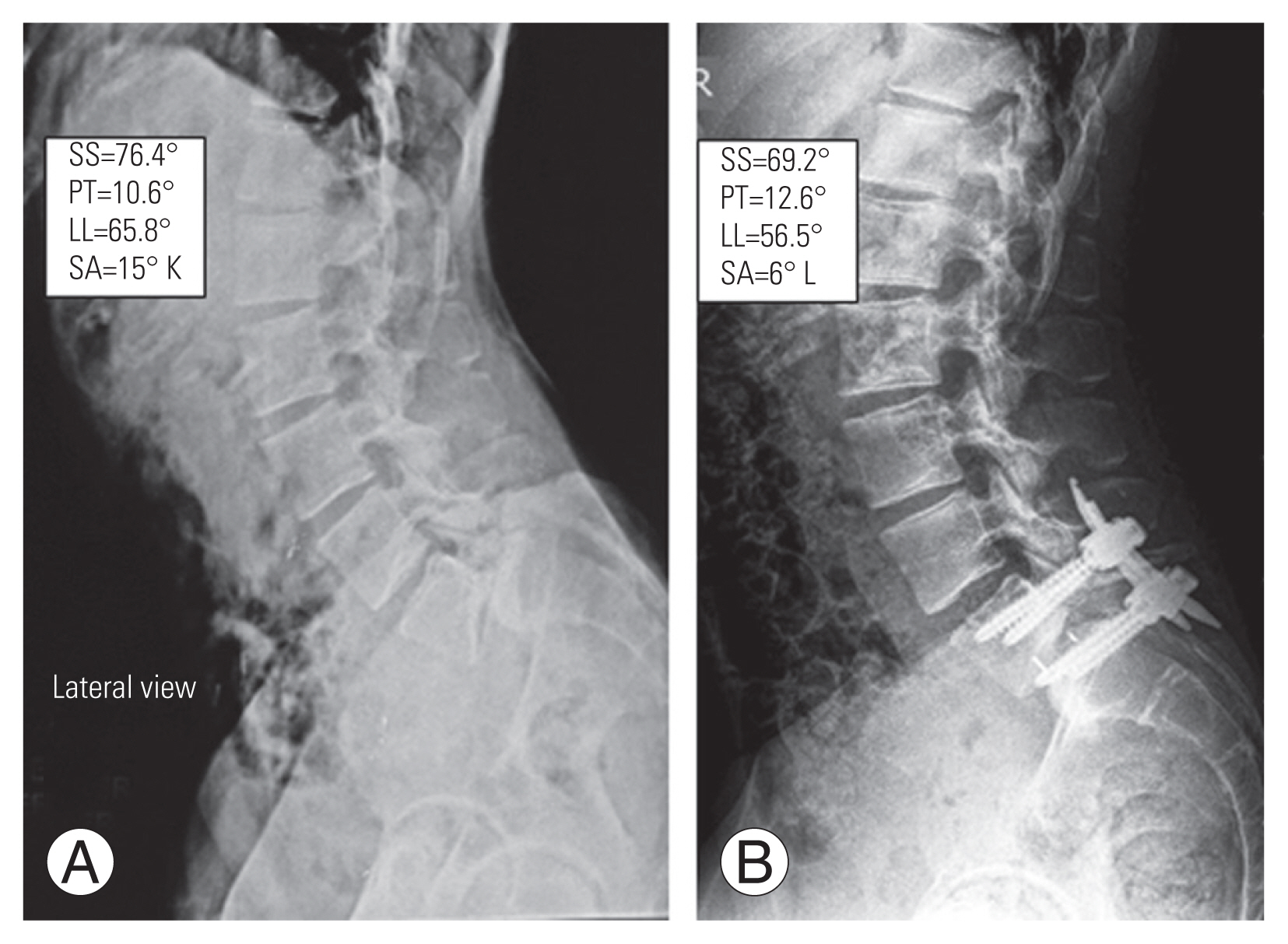
Fig.┬Ā4
(A, B) Grade-III spondylolisthesis was reduced up-to grade-I. SS, sacral slope; PT, pelvic tilt; LL, lumbar lordosis; SA, slip angle; K, kyphosis; L, lordosis.
Table┬Ā1
Comparisons of demographics and perioperative parameters between MTFD and open group
| Characteristic | MTFD | Open | p-valuea) |
|---|---|---|---|
| No. of patients | 25 | 23 | |
| Sex | |||
| ŌĆāMale | 9 | 8 | |
| ŌĆāFemale | 16 | 15 | |
| Average age (yr) | 45.84┬▒12.70 | 49.26┬▒13.33 | |
| Average follow-up (yr) | 5.76┬▒0.57 | 5.77┬▒0.51 | |
| Disc level | |||
| ŌĆāL5ŌĆōS1 | 22 | 22 | |
| ŌĆāL4ŌĆō5 (sacralise) | 3 | 1 | |
| Preoperative Meyerding grade | |||
| ŌĆāIII | 22 | 19 | |
| ŌĆāIV | 3 | 4 | |
| Postoperative Meyerding grade | |||
| ŌĆāCR | 16 (III: 15, IV: 1) | 13 (III: 12, IV: 1) | |
| ŌĆāGrade I | 9 (III: 7, IV: 2) | 9 (III: 7, IV: 2) | |
| ŌĆāGrade II | - | 1 (IV) | |
| Complaint | |||
| ŌĆāULP | 18 (III: 17, IV: 1) | 14 (III: 13, IV: 1) | |
| ŌĆāBLP | 7 (III: 5, IV: 2) | 9 (III: 6, IV: 3) | |
| Surgery | |||
| ŌĆāUTFD | 18 | - | |
| ŌĆāŌĆāULP | 15 (III: 14, IV: 1) | ||
| ŌĆāŌĆāBLP | 3 (III) | ||
| BTFD | 7 | - | |
| ŌĆāŌĆāULP | 3 (III) | ||
| ŌĆāŌĆāBLP | 4 (III: 2, IV: 2) | ||
| ŌĆāLa_minectomy + B/L root decompression | - | 23 | |
| Mean surgical time (min) | 188.12┬▒15.78 | 198.91┬▒18.33 | <0.05 |
| Estimated blood loss (mL) | 108.4┬▒23.61 | 363.47┬▒72.65 | <0.05 |
| Average Radiation exposure (sec) | 84.72┬▒22.01 | 45.17┬▒5.93 | <0.05 |
| Average hospital stay (day) | 3.36┬▒0.74 | 5.43┬▒1.47 | <0.05 |
Table┬Ā2
Comparison of clinical outcomes between MTFD and open groups
| Variable | MTFD | Open | p-valuea) |
|---|---|---|---|
| VAS for back pain | |||
| ŌĆāPreoperative | 7.24┬▒0.58 | 7.43┬▒0.66 | |
| ŌĆāPostoperative | |||
| ŌĆā3 mo | 3.56┬▒0.75 | 4.60┬▒1.19 | <0.05 (0.0007) |
| ŌĆā1 yr | 2.44┬▒0.80 | 3.08┬▒0.99 | <0.05 (0.017) |
| ŌĆā2 yr | 1.96┬▒0.66 | 2.13┬▒0.69 | >0.05 (0.393) |
| ŌĆā5 yr | 2.32┬▒1.01 | 2.17┬▒0.81 | >0.05 (0.593) |
| ŌĆāp-valueb) | <0.05 | <0.05 | |
| VAS for leg pain | |||
| ŌĆāPreoperative | 7.2┬▒0.93 | 7.17┬▒0.98 | |
| ŌĆāPostoperative | |||
| ŌĆā3 mo | 2.2┬▒0.93 | 2.08┬▒0.79 | >0.05 (0.65) |
| ŌĆā1 yr | 1.44┬▒0.63 | 1.30┬▒0.63 | >0.05 (0.46) |
| ŌĆā2 yr | 1.12┬▒0.71 | 1.08┬▒0.82 | >0.05 (0.88) |
| ŌĆā5 yr | 1.4┬▒0.63 | 1.17┬▒0.71 | >0.05 (0.25) |
| ŌĆāp-valueb) | <0.05 | <0.05 | |
| Modified ODI | |||
| ŌĆāPreoperative | 65.04┬▒6.09 | 69.39┬▒4.40 | |
| ŌĆāPostoperative | |||
| ŌĆā3 mo | 21.92┬▒4.28 | 30.78┬▒5.86 | <0.05 |
| ŌĆā2 yr | 13.28┬▒3.74 | 15.21┬▒4.81 | >0.05 (0.13) |
| ŌĆā5 yr | 15.84┬▒5.84 | 17.65┬▒5.83 | >0.05 (0.29) |
| ŌĆāp-valueb) | <0.05 | <0.05 | |
Table┬Ā3
Comparison of changes in spino-pelvic parameters after reduction between MTFD and open groups
| Variable | MTFD | Open | p-valuea) |
|---|---|---|---|
| Slip percentage | |||
| ŌĆāPreoperative | 63.88┬▒8.32 | 65.16┬▒9.16 | >0.05 |
| ŌĆāPostoperative | 8.36┬▒9.59 | 8.25┬▒9.96 | >0.05 |
| ŌĆāp-valueb) | <0.05 | <0.05 | |
| Slip angle (┬░) | |||
| ŌĆāPreoperative | 9.35┬▒3.96 (K) | 9.39┬▒3.05 (K) | >0.05 |
| ŌĆāPostoperative | ŌłÆ9.43┬▒3.10 (L) | ŌłÆ8.21┬▒1.85 (L) | >0.05 |
| ŌĆāp-valueb) | <0.05 | <0.05 | |
| Sacral slop (┬░) | |||
| ŌĆāPreoperative | 51.59┬▒9.91 | 47.95┬▒6.96 | >0.05 |
| ŌĆāPostoperative | 52.81┬▒5.85 | 48.04┬▒5.88 | <0.05 (0.004) |
| ŌĆāp-valueb) | >0.05 | >0.05 | |
| Lumbar lordosis (┬░) | |||
| ŌĆāPreoperative | 59.86┬▒6.49 | 57.52┬▒6.78 | >0.05 |
| ŌĆāPostoperative | 53.73┬▒4.97 | 51.04┬▒5.40 | >0.05 |
| ŌĆāp-valueb) | <0.05 | <0.05 | |
| Pelvic tilt (┬░) | |||
| ŌĆāPreoperative | 22.02┬▒7.18 | 20.15┬▒3.57 | >0.05 |
| ŌĆāPostoperative | 21.15┬▒3.57 | 20.13┬▒3.20 | >0.05 |
| ŌĆāp-valueb) | >0.05 | >0.05 | |
Table┬Ā4
Perioperative complications and long-term radiological outcomes
References
1. DeWald CJ, Vartabedian JE, Rodts MF, Hammerberg KW. Evaluation and management of high-grade spondylolisthesis in adults. Spine (Phila Pa 1976) 2005;30(6 Suppl): S49ŌĆō59.


2. Bridwell KH. Surgical treatment of high-grade spondylolisthesis. Neurosurg Clin N Am 2006;17:331ŌĆō8.


3. Kasliwal MK, Smith JS, Kanter A, et al. Management of high-grade spondylolisthesis. Neurosurg Clin N Am 2013;24:275ŌĆō91.


4. Lak AM, Abunimer AM, Devi S, et al. Reduction versus in situ fusion for adult high-grade spondylolisthesis: a systematic review and meta-analysis. World Neurosurg 2020;138:512ŌĆō20.


5. Passias PG, Poorman CE, Yang S, et al. Surgical treatment strategies for high-grade spondylolisthesis: a systematic review. Int J Spine Surg 2015;9:50.



6. Moreau S, Lonjon G, Guigui P, Lenoir T, Garreau de Loubresse C, Chopin D. Reduction and fusion in high-grade L5-S1 spondylolisthesis by a single posterior approach: results in 50 patients. Orthop Traumatol Surg Res 2016;102:233ŌĆō7.


7. Lengert R, Charles YP, Walter A, Schuller S, Godet J, Steib JP. Posterior surgery in high-grade spondylolisthesis. Orthop Traumatol Surg Res 2014;100:481ŌĆō4.


8. Kim DY, Lee SH, Chung SK, Lee HY. Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine (Phila Pa 1976) 2005;30:123ŌĆō9.

9. Lehmann W, Ushmaev A, Ruecker A, et al. Comparison of open versus percutaneous pedicle screw insertion in a sheep model. Eur Spine J 2008;17:857ŌĆō63.




10. Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine: do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976) 1995;20:1410ŌĆō8.

11. Moreau PE, Ferrero E, Riouallon G, Lenoir T, Guigui P. Radiologic adjacent segment degeneration 2 years after lumbar fusion for degenerative spondylolisthesis. Orthop Traumatol Surg Res 2016;102:759ŌĆō63.


12. Acosta FL Jr, Ames CP, Chou D. Operative management of adult high-grade lumbosacral spondylolisthesis. Neurosurg Clin N Am 2007;18:249ŌĆō54.


13. Kunze KN, Lilly DT, Khan JM, et al. High-grade spondylolisthesis in adults: current concepts in evaluation and management. Int J Spine Surg 2020;14:327ŌĆō40.



14. Tian W, Han XG, Liu B, et al. Posterior reduction and monosegmental fusion with intraoperative three-dimensional navigation system in the treatment of high-grade developmental spondylolisthesis. Chin Med J (Engl) 2015;128:865ŌĆō70.



15. Rajakumar DV, Hari A, Krishna M, Sharma A, Reddy M. Complete anatomic reduction and monosegmental fusion for lumbar spondylolisthesis of grade II and higher: use of the minimally invasive ŌĆ£rockingŌĆØ technique. Neurosurg Focus 2017;43:E12.

16. Min SH, Yoo JS, Lee JY. Usefulness of contralateral indirect decompression through minimally invasive unilateral transforaminal lumbar interbody fusion. Asian Spine J 2014;8:453ŌĆō61.



17. Sailhan F, Gollogly S, Roussouly P. The radiographic results and neurologic complications of instrumented reduction and fusion of high-grade spondylolisthesis without decompression of the neural elements: a retrospective review of 44 patients. Spine (Phila Pa 1976) 2006;31:161ŌĆō70.


18. Alzakri A, Labelle H, Hresko MT, et al. Restoration of normal pelvic balance from surgical reduction in high-grade spondylolisthesis. Eur Spine J 2019;28:2087ŌĆō94.



19. Sudarshan PK, Suthar HR, Varma VK, Krishnan A, Hegde SK. Long-term experience with reduction technique in high-grade spondylolisthesis in the young. Int J Spine Surg 2018;12:399ŌĆō407.



20. Poussa M, Remes V, Lamberg T, et al. Treatment of severe spondylolisthesis in adolescence with reduction or fusion in situ: long-term clinical, radiologic, and functional outcome. Spine (Phila Pa 1976) 2006;31:583ŌĆō92.


21. Transfeldt EE, Mehbod AA. Evidence-based medicine analysis of isthmic spondylolisthesis treatment including reduction versus fusion in situ for high-grade slips. Spine (Phila Pa 1976) 2007;32(19 Suppl): S126ŌĆō9.


22. Kasliwal MK, Smith JS, Shaffrey CI, et al. Short-term complications associated with surgery for high-grade spondylolisthesis in adults and pediatric patients: a report from the scoliosis research society morbidity and mortality database. Neurosurgery 2012;71:109ŌĆō16.

23. Sansur CA, Reames DL, Smith JS, et al. Morbidity and mortality in the surgical treatment of 10,242 adults with spondylolisthesis. J Neurosurg Spine 2010;13:589ŌĆō93.


24. Graham RB, Hashmi S, Maslak JP, Koski TR,Lumbar deformity spondylolisthesis (moderate-high grade) complication. Mummaneni PV, Park P, Crawford CH, Kanter AS, Glassman SD, editors. Spinal deformity: a case-based approach to managing and avoiding complications. Cham: Springer; 2017. p.291ŌĆō300.

25. Petraco DM, Spivak JM, Cappadona JG, Kummer FJ, Neuwirth MG. An anatomic evaluation of L5 nerve stretch in spondylolisthesis reduction. Spine (Phila Pa 1976) 1996;21:1133ŌĆō9.


26. Gandhoke GS, Kasliwal MK, Smith JS, et al. A multicenter evaluation of clinical and radiographic outcomes following high-grade spondylolisthesis reduction and fusion. Clin Spine Surg 2017;30:E363ŌĆō9.


27. Yee TJ, Terman SW, La Marca F, Park P. Comparison of adjacent segment disease after minimally invasive or open transforaminal lumbar interbody fusion. J Clin Neurosci 2014;21:1796ŌĆō801.


- TOOLS







