 |
 |
- Search
| Asian Spine J > Volume 17(6); 2023 > Article |
|
Abstract
Hyperextension injuries of the ankylosed thoracolumbar spine, particularly those with preexisting kyphotic deformity, present significant therapeutic challenges. The authors viewed that such injuries without displacement or fractures of the posterior elements are reasonable candidates for standalone percutaneous vertebroplasty (PVP). In such cases, the posterior tension band is spared; thus, fractures are unstable not in the lateral direction, which would lead to the translation of the fracture, but in the vertical direction. Such vertical instability of the fracture can be stabilized if the open mouth-type vertebral cleft is adequately filled with a sufficiently large amount of polymethylmethacrylate (PMMA) cement. Our three patients receiving standalone PVP received injections of 12 mL, 16.5 mL, and 18 mL of PMMA cement. This minimally invasive surgical procedure achieved both short-term (immediate pain relief and mobilization) and long-term (fracture healing) goals.
Ankylosing spinal disorders, such as ankylosing spondylitis (AS) and diffuse idiopathic skeletal hyperostosis (DISH), present significant challenges in patients with spinal trauma [1–3]. The preexisting frailty of the patient population, typically older ones with medical morbidities, often outweighs the biomechanical benefit of surgical fixation using spinal instrumentation. To minimize surgical invasiveness, percutaneous vertebroplasty (PVP) has been reported for the treatment of ankylosed spinal fractures as a standalone procedure [4,5]. However, indications for standalone vertebroplasty under these conditions remain unclear. The authors viewed that hyperextension injuries of the ankylosed thoracolumbar spine without neurological deficits and without displacement/fractures of the posterior elements (some AO type B3 fractures) are good candidates for standalone PVP [6–9].
The protocol of this single-institution-based retrospective study was reviewed and approved by the institutional review board of Asahikawa Kosei General Hospital (approval code: 2022059). Informed consent for publication was obtained by all participants in this study.
Hyperextension injuries of the ankylosed spine are often associated with preexisting kyphotic deformities of the spine segment, resulting in open fish-mouth-type fractures of the vertebra (AO type B3) [6–9]. PVP for these conditions aims to fill in the intravertebral cleft (fish mouth) with a sufficient amount of polymethylmethacrylate (PMMA) cement. At this point, the reduction of the fracture is not strictly indicated given an appeal to using the fracture to improve preoperative kyphotic alignment. Accordingly, techniques for reducing the fracture such as flexing the surgical table or performing surgery on the lateral decubitus position were not employed [10]. A standard Jackson-type surgical table (Universal Frame; Getinge Group, Göteborg, Sweden) was used.
Practical concerns for these conditions are as follows: (1) possible leakage of the PMMA cement outside the vertebra through the ruptured anterior longitudinal ligament (ALL) and (2) the requirement for a large amount of PMMA cement as the fractured vertebra may enlarge beyond normal vertebral size.
To avoid cement leakage, vertebrography was performed before cement injection as described elsewhere [11]. During surgery, the patient was placed in the prone position on the operation table under general anesthesia. Two needles were inserted through bilateral pedicles. The contrast medium was then injected. In all three cases, the injected contrast medium came out from the other needle through the intravertebral cleft, i.e., without leakage outside the vertebra. The lack of leakage through the ALL is likely attributed to the formation of a hematoma envelope in the fractured vertebra. The intervals between the fracture and PVP procedure were 4 weeks in cases 1 and 2 and 1 week in case 3. The delay in the first two cases was associated with initial attempts of conservative treatment including body casting and that in the third case was with surgical treatment for a coincident femoral fracture.
After washing out the contrast, PMMA cement (HVR; Medtronic Co., Tokyo, Japan) was injected using bone filler devices (Medtronic Co.). Cement injection was started without waiting time (i.e., at the liquid phase) so that the intravertebral cleft could be filled with a sufficiently large amount of cement before thickening. Patients 1, 2, and 3 were injected with 12 mL, 16.5 mL, and 18 mL of cement, respectively (Table 1).
Vertebrography confirmed that cement leakage into the spinal canal was prevented, and the injected contrast medium came out from the other needle through the intravertebral cleft. This preliminary procedure indicated that the liquid-type cement would advance no further posteriorly than the anterior tip of the needles.
Table 1 summarizes the demographics and clinical outcomes of the three patients. Their preoperative and postoperative images are presented in Figs. 1–3 (case 1, Fig. 1; case 2, Fig. 2; case 3, Fig. 3). Computed tomography (CT) showed ossification of the ALL and ankylosis of the spine, whereas bilateral sacroiliac joints and facet joints remain unfused, indicating DISH rather than AS. The ankylosed spine showed kyphotic deformity (Figs. 1A, 2A, and 3A). Each patient had a hyperextension injury that had not propagated to the posterior elements.
Initial treatments with a body cast or hard brace and teriparatide failed to control back pain. Thus, the patients opted to proceed with PVP. Following PVP, the patients wore a custom-molded plastic thoracolumbosacral orthosis (TLSO) (Fig. 4A–C), which is typically used in the treatment of osteoporotic vertebral fractures at Asahikawa Kosei General Hospital, Asahikawa, Japan, for 3 months [12–14]. Mobilization to an erect position was allowed soon after TLSO application. They tolerated sitting up with the orthotic brace, and lateral sitting-supine X-ray images revealed stabilization of the fractured vertebra (Figs. 1D, E and 2E, F). Follow-up CT demonstrated bony consolidation adjacent to the cement and formation of bridging callus over time (Figs. 1F–I, 2G–I, and 3D–H). Eventually, the fracture was healed providing de facto reconstruction of the ankylosed spine.
When discussing the indications of standalone PVP for ankylosed thoracolumbar spinal fractures, AS and DISH must be distinguished first. In patients with AS, ankylosis often involves the facet joints in addition to the sacroiliac joints. Ankylosis involving both vertebral bodies/discs and facet joints represents three-column ankylosis. Vertebrae with such three-column ankylosis are susceptible to three-column injuries in the case of fractures. By contrast, facet joints remain unfused in DISH, typically resulting in two-column ankylosis. Vertebrae injuries with such two-column ankylosis would result in a two-column fracture without involving the posterior column, particularly when caused by minor trauma such as a ground-level fall.
In hyperextension injuries of the ankylosed spine without posterior column involvement, the posterior tension band is spared [6–9], and the resultant vertebral fractures are unstable not in the lateral direction, which would lead to the translation of the fracture, but in the vertical direction. Thus, the risks of translation and subsequent spinal cord injury during positioning on the surgical table would be low. Our patients were positioned in the standard fashion without using a special technique such as the Jackson table turn technique [15]. Vertical instability of the fracture can be stabilized if the open mouth-type vertebral cleft is adequately filled with PMMA cement.
The diagnosis of a posterior column fracture was made based on the presence of a fracture line in the posterior column on sagittal CT images and a high signal lesion in short tau inversion recovery sagittal magnetic resonance images as reported earlier [16]. In that report, four ankylosed thoracolumbar spinal fractures (all three-column fractures) were treated with surgical fixation using spinal instrumentation. In cases of hyperextension injuries of the ankylosed spine involving all three columns, supplemental fixation such as percutaneous pedicle screw instrumentation is indicated in addition to PVP.
For cases 1 and 2, conservative management was initially attempted, given their comorbidities and severe concomitant injuries. In the literature, two cases of hyperextension injuries of the ankylosed spine had been treated conservatively [17,18]. One patient, who was treated with a brace and 8 weeks of bed rest, achieved healing of the fracture [17]. The other patient, who was treated with a brace and teriparatide, but not extended bed rest, had delayed paraplegia and eventually underwent surgical fixation [18]. Since PVP can be performed using local anesthesia [4,5,11], PVP under local anesthesia would serve as a reasonable alternative to conservative management for patients with prohibitively high risks of surgical treatment under general anesthesia.
The small number of cases and short follow-up duration represent serious limitations in this report. Thus, the follow-up of case 3 was unavoidably terminated because of the lethal coronavirus disease 2019 infection. Of note, during these follow-ups, albeit short, all three patients were mobilized without developing delayed paraplegia. This finding, in addition to the CT images showing union processes of the fractures, supports the stabilization efficacy and durability of standalone PVP on the fracture sites.
In our previous study with 14 cases of vertebral pseudarthrosis following vertebral compression fractures [11], PVP with an average of 3.5 mL of PMMA cement led to not only immediate pain relief but also subsequent bony responses including bony spur and callus formation. These findings prompted us to apply PVP to the treatment of hyperextension injuries of these ankylosed spines. Thus, the current PVP is an advanced version of our previous PVP.
In conclusion, standalone PVP with injections of a large amount of PMMA cement can be another surgical option for hyperextension injuries of the ankylosed thoracolumbar spine in patients with preexisting frailty, advanced age, medical comorbidities, and preexisting thoracolumbar kyphotic deformity. With this minimally invasive procedure, both the short-term (immediate pain relief and mobilization) and long-term (fracture healing with reconstruction of the ankylosed spine) goals were achieved.
Fig. 1
Images of case 1 patient. A sagittal image of the computed tomography (CT) scans (A) and a three-dimensional CT scan image (B) show kyphotic deformity of thoracolumbar spine with multiple old vertebral fractures. The T10 vertebral body was fractured with an open fish-mouth deformity along with ossification of the anterior longitudinal ligament from T5 to T12 vertebra. A short tau inversion recovery magnetic resonance image (C) displays high signal in the T10 vertebral body but not in the posterior element. Sitting lateral (D) and supine lateral (E) radiographs taken 2 weeks after percutaneous vertebroplasty (PVP) shows no mobility of the T10 vertebral body. Coronal (F) and sagittal (G) images of the CT scans taken immediately after PVP, and those taken 1 year later (H, I). There is bony consolidation adjacent to the cement with formation of a bridging callus at the T10 vertebral body (H, I).
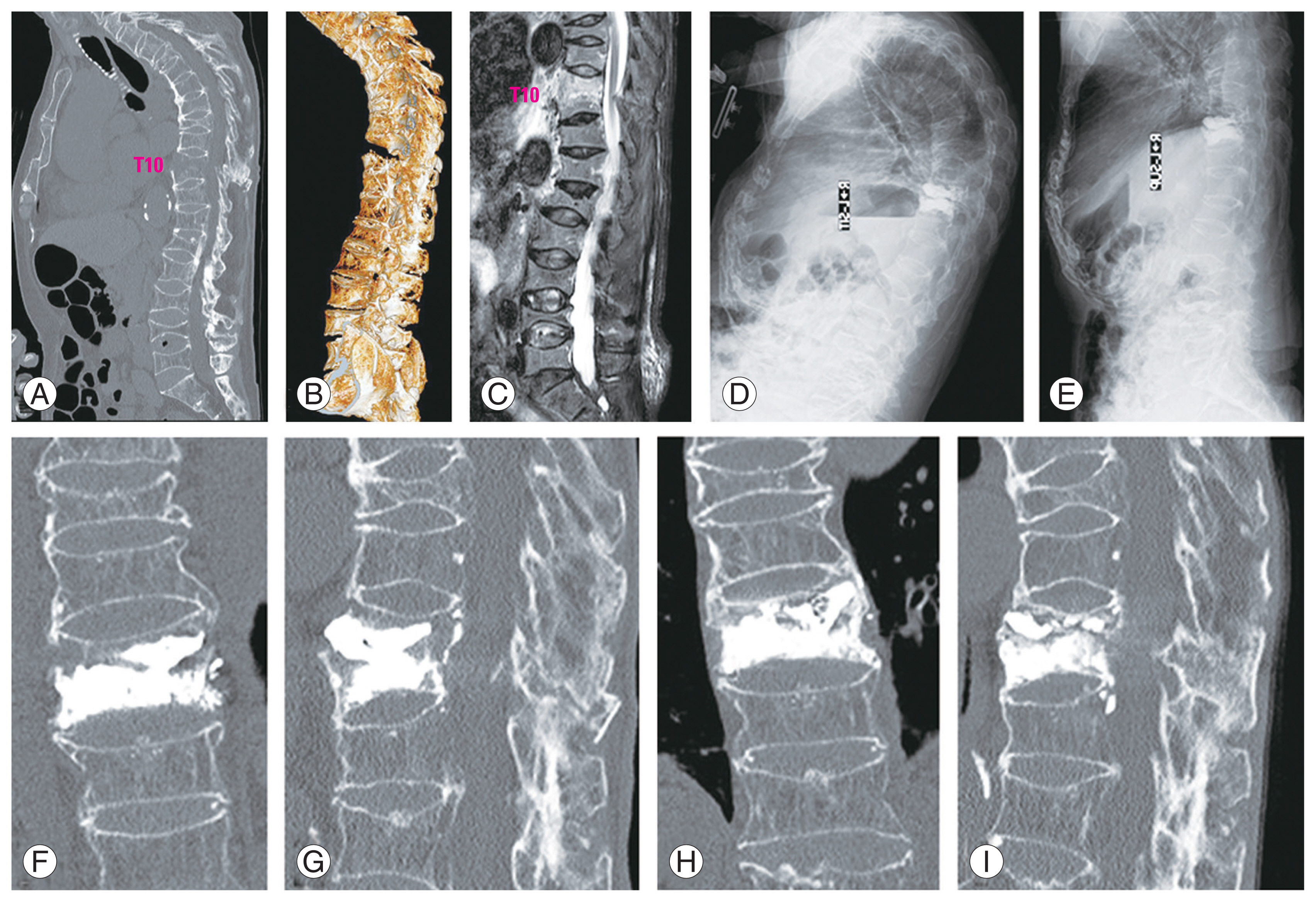
Fig. 2
Images of case 2 patient. A sagittal image of the computed tomography (CT) scans (A), showing sclerosis and compression deformity of T11 and T12 vertebral bodies, and a fracture line at the T12 vertebra. This suggests old fractures of the T11 and T12 vertebrae, and a refracture of the T12 vertebra. A three-dimensional CT scan image (B) reveals ossification of the anterior longitudinal ligament from the T5 to T12 vertebra. Sitting lateral (C) and supine lateral (D) radiographs taken after 3 weeks of conservative treatment show mobility of the T12 vertebral body with an open fish-mouth deformity (D). Sitting lateral (E) and supine lateral (F) radiographs taken 1 week after percutaneous vertebroplasty (PVP) shows no mobility of the T12 vertebral body. Coronal images of the CT scans taken immediately after PVP (G), 6 months later (H) and 1 year later (I). There is bony consolidation adjacent to the cement in (H) and (I). Formation of a bridging callus resulted in an extension of ankylosis from the T5–T12 vertebrae into the T5–L1 vertebrae.
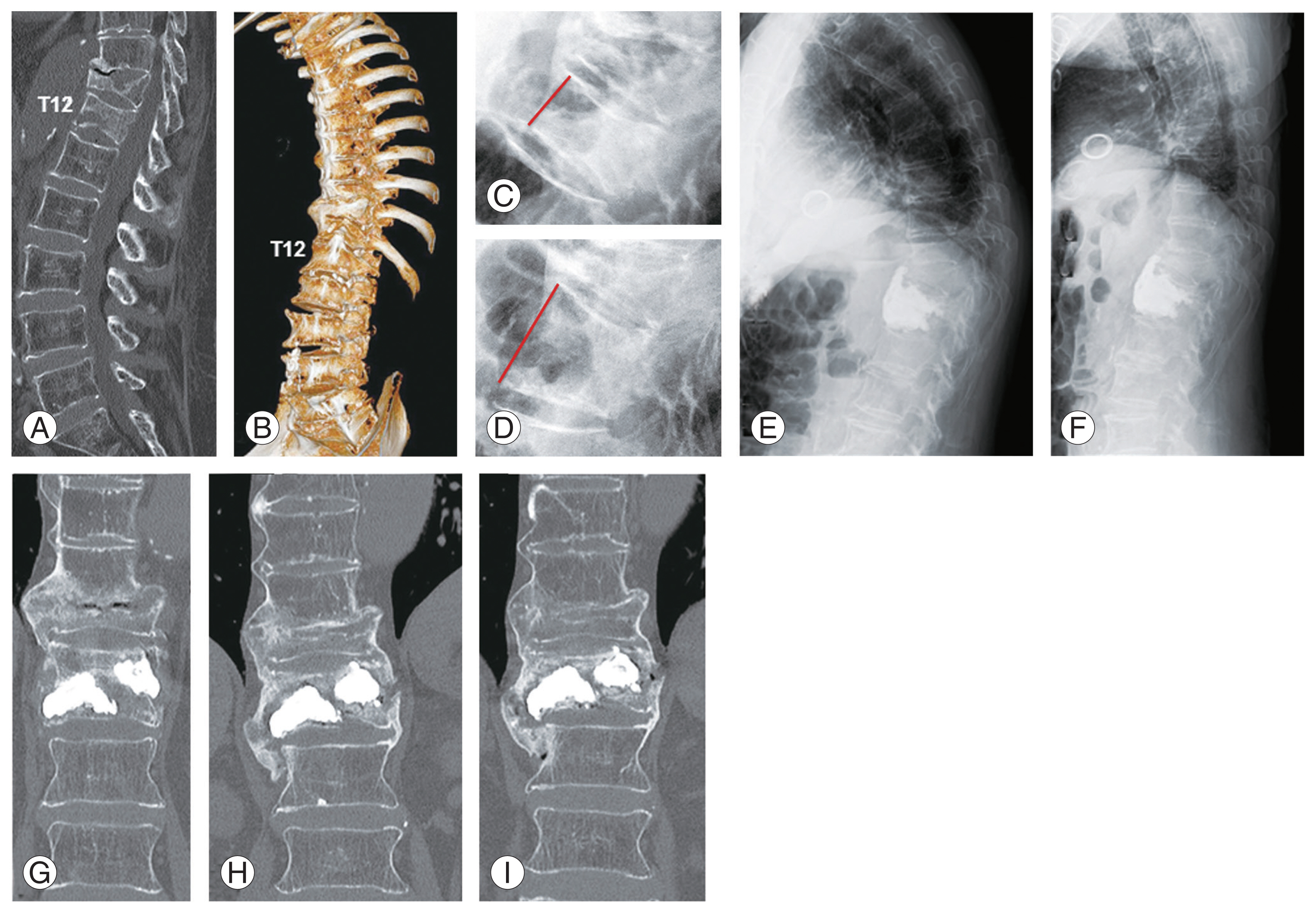
Fig. 3
Images of case 3 patient. A sagittal image (A) and three-dimensional image (B) of the computed tomography (CT) scans shows a fracture and open fish-mouth deformity of the L3 vertebral body along with ossification of the anterior longitudinal ligament from the T12 to S1 vertebra. The short tau inversion recovery magnetic resonance image (C) displays a high signal in the L3 vertebral body, but not in the posterior element. Coronal images of the CT scans taken immediately after percutaneous vertebroplasty (PVP) (D), 2 months later (E), 5 months later (F) and 9 months later (G), as well as a sagittal reconstruction image taken 9 months after PVP (H) reveal bony consolidation adjacent to the cement and the formation of a bridging callus overtime.
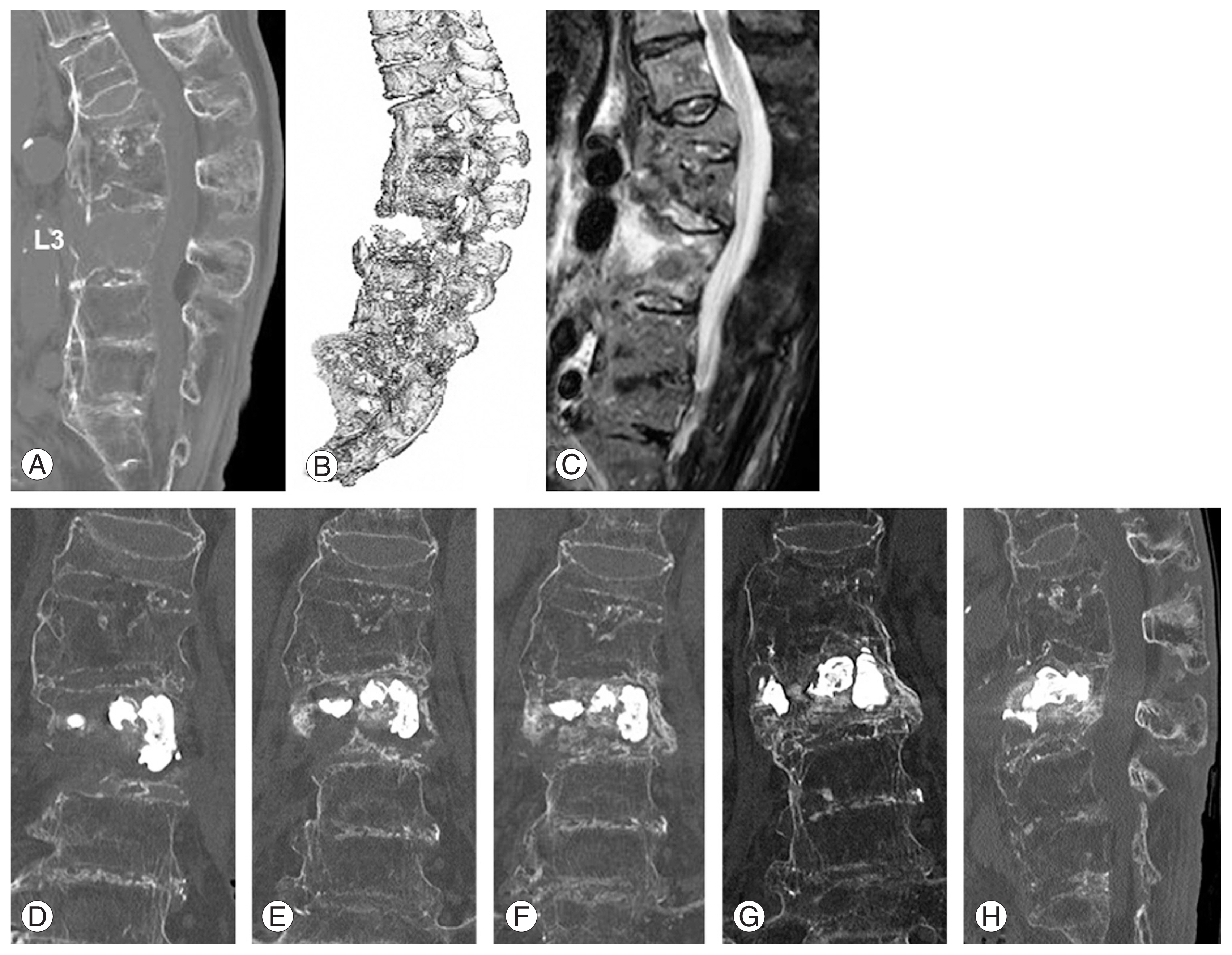
Fig. 4
Picture of a custom molded plastic thoracolumbosacral orthosis. (A) Front view, (B) lateral view, and (C) rear view.
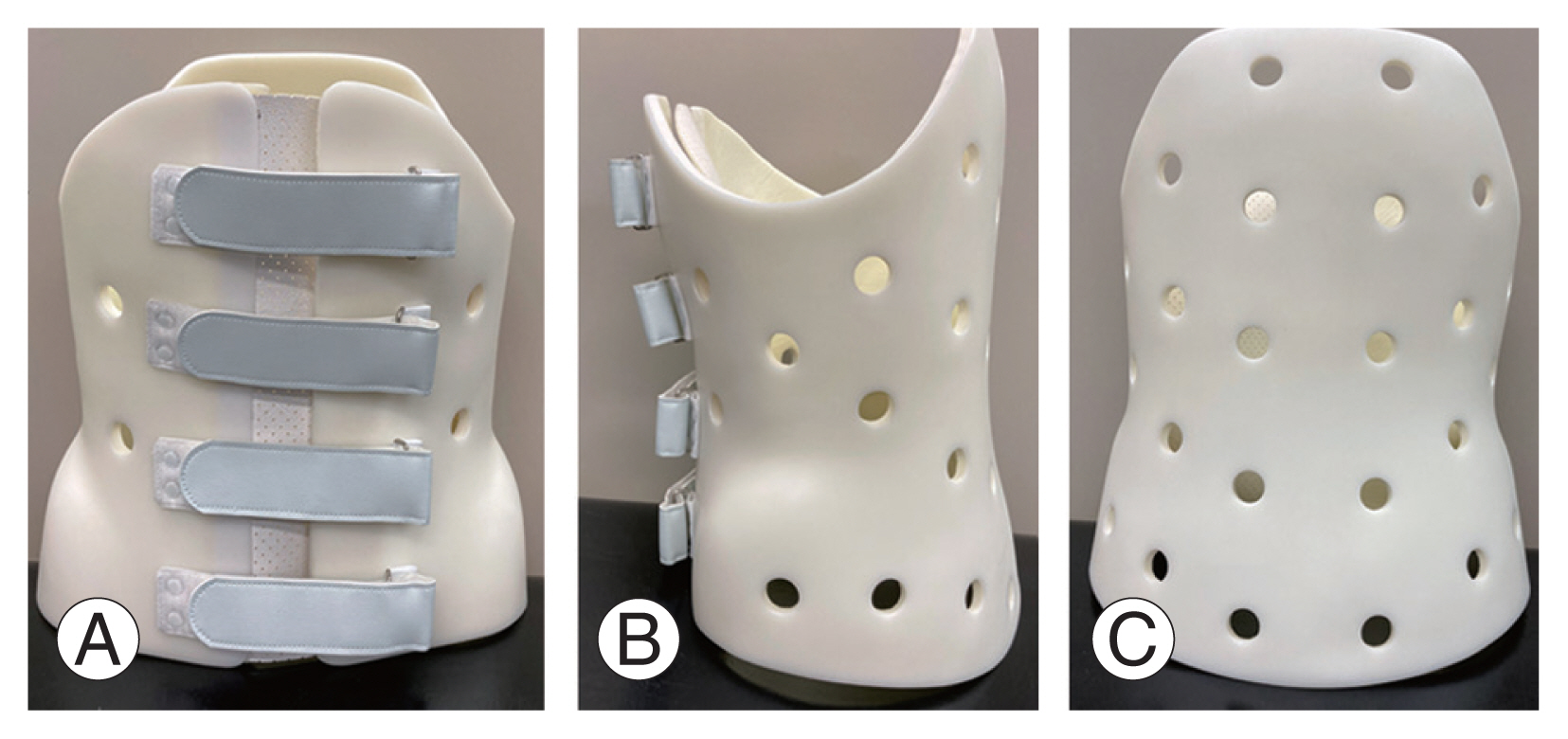
Table 1
Demographics and clinical outcomes of the three patients
References
1. Konopka J, Fogel HA, Diwan A,Inflammatory arthritis. Truumees E, Prather H, editors. Orthopaedic knowledge update spine 6. 6th ed. Rosemont (IL): Wolters Kluwer Health; 2022. p.507–21.
2. Child ZA, Bransford RJ,Fractures in ankylosing conditions. Vialle LR, Bellabarba C, Kandziora F, editors. Thracolumbar spine trauma. New York (NY): Thieme Medical Publishers Inc; 2016. p.141–51.
3. Rustagi T, Drazin D, Oner C, et al. Fractures in spinal ankylosing disorders: a narrative review of disease and injury types, treatment techniques, and outcomes. J Orthop Trauma 2017;31(Suppl 4): S57–74.


4. Kulkarni AG, Agarwal VK, Kumar KcN, Kumar A, Patel A. Is long-segment fixation a rule in fractures associated with ankylosing spondylitis? Int J Spine Surg 2019;13:215–20.



5. Prestat AJ, Gondim Teixeira PA, et al. First intention vertebroplasty in fractures within an ankylosed thoracolumbar spinal segment. Diagn Interv Imaging 2021;102:421–30.


6. Bevevino AJ, Vaccaro AR, Rubenstein R,The AOSpine thoracolumbar injury classification. Vialle LR, Bellabarba C, Kandziora F, editors. Thracolumbar spine trauma. New York (NY): Thieme Medical Publishers Inc; 2016. p.1–8.
7. Joaquim AF, Patel AA, Schroeder GD, Vaccaro AR. A simplified treatment algorithm for treating thoracic and lumbar spine trauma. J Spinal Cord Med 2019;42:416–22.



8. Schnake KJ, Schroeder GD, Vaccaro AR, Oner C. AOSpine classification systems (subaxial, thoracolumbar). J Orthop Trauma 2017;31(Suppl 4): S14–23.



9. Vu C, Gendelberg D. Classifications in brief: AO thoracolumbar classification system. Clin Orthop Relat Res 2020;478:434–40.



10. Ikuma H, Hirose T, Takao S, et al. The impact of the lateral decubitus position in the perioperative period on posterior fixation for thoracolumbar fracture with ankylosing spinal disorder. J Neurosurg Spine 2021;36:784–91.


11. Kawaguchi S, Horigome K, Yajima H, et al. Conversion to hypertrophic vertebral pseudarthrosis following percutaneous vertebroplasty. Eur Spine J 2010;19:901–6.




12. Watanabe G, Kawaguchi S, Kanaya K. Osteoporotic vertebral fractures treated with thoracolumbosacral orthosis: a prospective study. J Spine Res 2011;2:308–10.
13. Murata K, Watanabe G, Kawaguchi S, et al. Union rates and prognostic variables of osteoporotic vertebral fractures treated with a rigid external support. J Neurosurg Spine 2012;17:469–75.


14. Morita T, Watanabe G, Kanaya K. Fracture union and quality of life in patients with osteoporotic vertebral fracture treated with rigid or soft external support. J Spine Res 2015;6:125–31.
15. Moon AS, Cignetti CA, Isbell JA, Weng C, Rajaram Manoharan SR. Traumatic hyperextension-distraction injuries of the thoracolumbar spine: a technical note on surgical positioning. Eur Spine J 2019;28:1113–20.



16. Fukushi R, Kawaguchi S, Watanabe G, Horigome K, Yajima H, Yamashita T. Repetitive vertebral fractures in patients with ankylosing spinal disorders: a report of two cases. Spine Surg Relat Res 2018;3:188–92.



- TOOLS







