 |
 |
- Search
| Asian Spine J > Volume 18(1); 2024 > Article |
|
Abstract
Purpose
To analyze the association between preoperative adjacent facet joint osteoarthritis (FJOA) and outcomes of lumbar interbody fusion (LIF).
Overview of Literature
Whether preoperative adjacent FJOA is associated with the incidence of radiological adjacent segment degeneration (RASD) and low back pain (LBP) relief after lumbar fusion remains unknown.
Methods
The study included patients who underwent LIF. The demographic characteristics and radiographic and surgical data were collected and evaluated. The included patients were divided into control group and FJOA group based on the preoperative adjacent facet joint Pathria grade. Preoperative and last follow-up LBP Visual Analog Scale (VAS) score, leg pain (LP) VAS, Oswestry Disability Index (ODI) and RASD were evaluated and compared. The improvement rates in VAS and ODI were calculated and compared between the two groups. Logistic regression was used to analyze the risk factors of LBP relief and incidence of RASD.
Results
In total, 197 patients (control group, 86; FJOA group, 111) were included, and the median follow-up was 46 months. The VAS and ODI in both groups significantly improved after surgery. At the last follow-up, the FJOA group had higher VAS and lower VAS improvement rates of LBP than the control group (p<0.05). However, no significant difference in the LP VAS and ODI was found between the two groups. The incidence of RASD in the FJOA group was significantly higher than that in the control group (48.6% vs. 30.2%, p=0.034). Multivariate logistic regression analysis showed that preoperative adjacent FJOA was significantly associated with LBP relief (odds ratio [OR], 0.691; 95% confidence interval [CI], 0.498ŌĆō0.958) and the postoperative incidence of RASD (OR, 1.406; 95% CI, 1.020ŌĆō1.939).
The zygapophyseal joints or facet joints are complex biomechanical structures in the spine with complex anatomy, and their mechanical properties affect the overall behavior and health of the spine. Facet joint osteoarthritis (FJOA) may lead to lumbar spondylolisthesis and reduce spinal stability [1,2]. Conversely, osteophytes around the facet joints and inflammatory reactions can compress and stimulate peripheral nerves, resulting in low back and leg pain. Up to 15%ŌĆō40% of patients with chronic low back pain can be attributed to the facet joints [3].
Spinal fusion surgery or interbody fusion has been widely used to treat various degenerative spinal diseases [4]. Spinal fusion is an effective, safe, and reliable treatment. Compared with conservative treatment, surgical treatment can significantly reduce pain and improve functions. However, many complications have emerged with its wide application, including pseudarthrosis, loosening or breaking of the implant, and adjacent segment degeneration [5,6].
Recently, adjacent segment degeneration (ASD) has drawn increasing attention in the long-term care of patients. ASD can be further categorized as radiological ASD (RASD) and clinical ASD (CASD). RASD includes postoperative disc degeneration, osteophyte formation, and spinal stenosis, with incidence ranging from 11%ŌĆō100% [7]. ASD has become the most vexatious complication following lumbar fusion surgeries [8]. Several risk factors may cause ASD, such as age, sex, preoperative adjacent disc degeneration, multilevel fusions, sagittal imbalance, types of fusion, facet tropism, and laminar inclination [9]. Among them, preoperative adjacent segment degeneration is considered a common risk factor that causes ASD following lumbar spinal fusion [10]. A prospective study showed that preoperative adjacent mild spinal stenosis significantly affected efficacy and significantly increased the risk of early postoperative ASD [11]. The degeneration of adjacent facet joints before lumbar fusion will increase the spinal range of motion and decrease spinal stability, which is likely to accelerate ASD progression and affect clinical symptom improvement.
So far, many related studies have examined the effect of adjacent degeneration following lumbar fusion surgery, and a few studies have focused on the effect of preoperative adjacent disc degeneration, spinal stenosis, and other factors on postoperative clinical efficacy. However, relatively no studies have examined the effect of preoperative adjacent FJOA on the clinical efficacy and RASD following lumbar fusion.
Therefore, this study aimed to analyze the association between preoperative adjacent FJOA and clinical efficacy following lumbar fusion and the radiological outcomes. The results of this study will help clarify whether preoperative adjacent FJOA results in worse clinical outcomes and predisposes patients to RASD postoperatively, which can help determine if more fusion constructs may be warranted.
After obtaining the approval of the Ethics Committee of the Third Affiliated Hospital at the Sun Yat-Sen University (ID: 20190218801), we retrospectively reviewed the records of all patients who underwent lumbar spinal fusion surgery of the L1ŌĆōS1 segments for spinal degenerative disease between January 2012 and December 2019. Cases were consecutive and reflected each surgeonŌĆÖs surgical preference. This study included those who had undergone imaging examinations and preoperative physical examinations to confirm that low back pain or leg pain was caused by spinal degeneration. If the diagnosis could not be confirmed in the above-mentioned examinations, nerve root block or computed tomography (CT) myelography was conducted. Informed consent was not required for this type of retrospective study.
The inclusion criteria were as follows: preoperative low back pain or leg pain, imaging suggesting lumbar degeneration, conservative treatment was ineffective, preoperative clear responsibility was L1ŌĆōS1, lumbar fusion surgery was performed, preoperative medical records were complete, and the postoperative follow-up was >2 years.
The exclusion criteria were as follows: lumbar tumors, infectious diseases, vertebral fractures, scoliosis and other congenital spinal diseases, cervical and thoracic diseases, history of lumbar surgery, cognitive impairment or mental illness, no follow-up data, knee and hip joint diseases, and missing preoperative lumbar anteroposterior and lateral X-ray imaging, CT, and magnetic resonance imaging (MRI) (Fig. 1).
Once the diagnoses of all patients were confirmed, vast-experienced spinal surgeons discussed and obtained the surgical plan. Moreover, 3ŌĆō4 surgeons at the deputy director level or higher performed the surgery. The surgery was performed under general anesthesia. The classic posterior lumbar fixation and fusion, pedicle screw internal fixation, laminectomy, and decompression were performed. During the surgery, the nerves, blood vessels, adjacent joints, and joint capsules were protected, and intervertebral, intertransverse, and posterolateral fusion methods were employed. Postoperative antibiotics were routinely used to prevent infection, and hormones were used for three consecutive days. The patients left the bed for mobilization 3 days after surgery and wore a lumbar fixed brace for 3 months.
X-ray, MRI, and CT of the lumbar spine were performed to evaluate the imaging findings of the culprit and adjacent segments before surgery. At the most recent follow-up, X-ray images were acquired. The degeneration grade of the facet joint was evaluated on CT by Pathria grade [12]. The grade of spondylolisthesis and lumbar instability were evaluated via lumbar X-ray images. The T2-weighted sagittal and axial magnetic resonance (MR) images were assessed to evaluate L1ŌĆōS1 disc degeneration by the Pfirrmann grade [13]. All measurements were performed using PACS.
Patients were divided into groups according to the preoperative degree of the facet joints of the adjacent segment, represented by Pathria grade (Fig. 2). To avoid intraobserver bias, images were reviewed by two senior spine surgeons at each center. If they disagreed, a third was invited to make a final decision. Patients without or with slight FJOA (grades 1 and 2) at the adjacent segment were added to the control group, and patients with mild or severe FJOA (grades 3 and 4) at the adjacent segment were added to the FJOA group. The imaging manifestations of the disc degeneration and spondylolisthesis were not used in the grouping of the patients. The preoperative adjacent segment was defined as that above or below the operative segment. If the left, right, upper, and lower facet joint grades were not consistent, the highest one was used for grading.
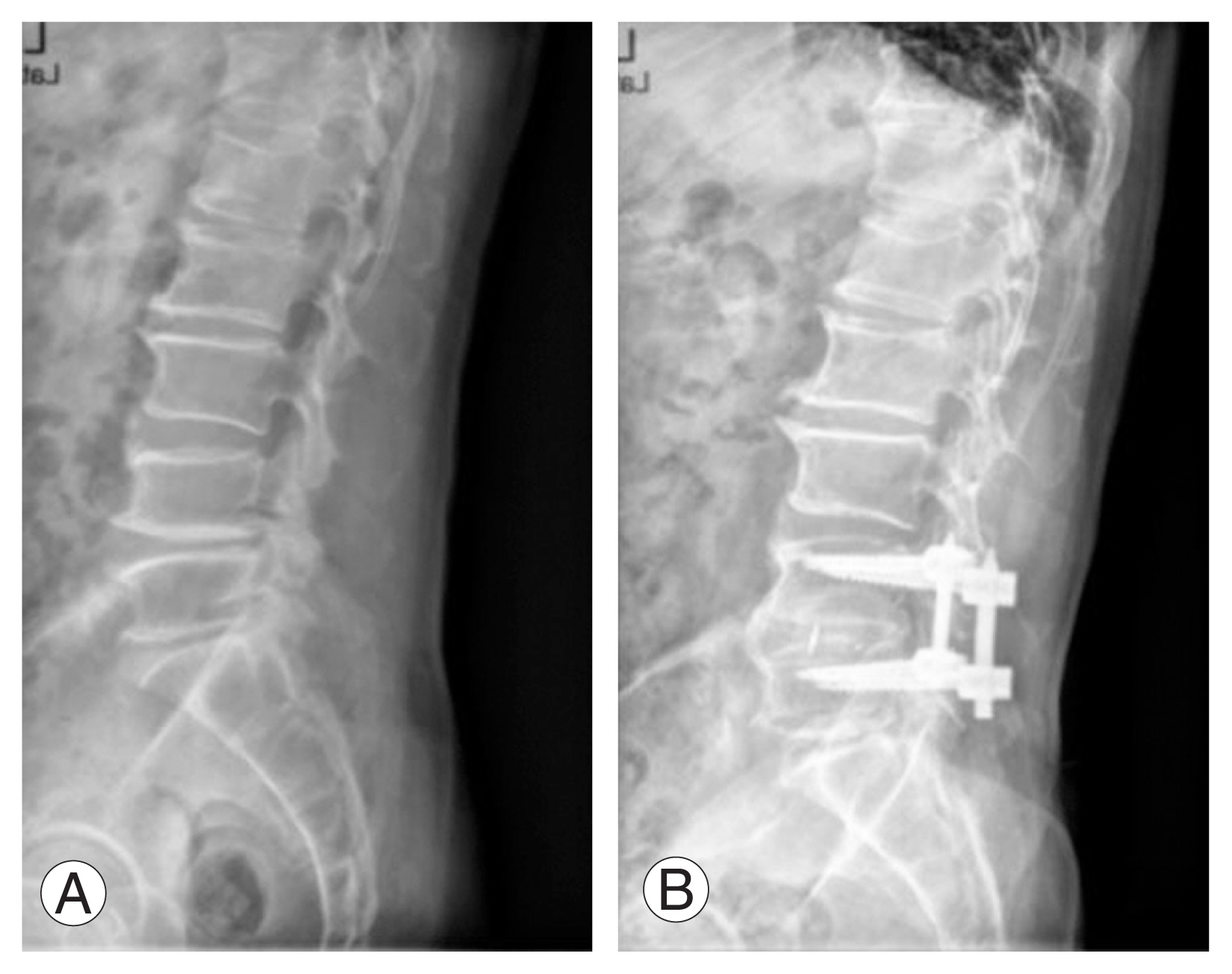
Postoperative RASD, a radiological finding, was defined as follows according to manifestations on plain radiography: (1) progression of 3 mm in vertebral slippage in comparison with preoperative lateral radiographs, a change of 10┬░ in the intervertebral angle on flexion and extension lateral radiograph; (2) endplate sclerosis or scoliosis deformity in the coronal plane; (3) loss of the disc space height by >10%; and (4) new osteophyte formation or increase in existing osteophytes by >3 mm (Fig. 3).
PatientsŌĆÖ age, sex, preoperative body mass index (BMI), hospital stay, and whether they suffered from hypertension, diabetes, or coronary artery disease were collected during hospitalization. Surgical data, including the American Society of Anesthesiologists (ASA) classification of anesthesia, operation time, blood loss, operative segment, surgical method, and severe postoperative complications were recorded. Preoperative clinical function questionnaires, including the Oswestry Disability Index (ODI), and Visual Analog Scale (VAS) scores of the low back and leg pain, were completed on admission for surgery without assistance. At the last follow-up, the VAS scale scores of the low back and leg pain, ODI score, physical function (PF) domain of 36-Item Short-Form Health Survey (SF-36), and modified MacNab criteria of all patients were acquired by phone. Moreover, the VAS improvement rate of the low back and leg pain were defined as follows. Significant relief of low back pain was defined as a VAS improvement rate of the low back pain Ōēź75%. Between January and February 2021, all the enrolled patients were followed up for at least 2 years from the date of surgery. Questionnaires were completed by phone at the final follow-up.
Statistical analyses were conducted using IBM SPSS Statistics ver. 21.0 (IBM Corp., Armonk, NY, USA). A modified Kolmogorov-Smirnov test was used to test for normally distributed data. Measurement data with normal distribution were expressed as mean┬▒standard deviation (SD). The independent sample t-test was used for comparison. Measurement data without normal distribution were expressed as median (interquartile range, IQR). The Mann-Whitney test was used for comparison. The Wilcoxon test was used for the comparison of preoperative VAS or ODI scores and final follow-up ones. Categorical data were expressed as frequency (percentage), and the chi-square test was used for comparison. The Mann-Whitney test was used for the comparison of grades. CohenŌĆÖs coefficient Kappa (╬║) was used to measure interobserver and intraobserver agreements, and the Spearman rank correlation was used to analyze the correlation between the degree of FJOA and degenerative factors such as intervertebral disc and facet joint tropism, and logistic regression was used to analyze influencing factors of postoperative low back pain in significant remission and those of postoperative RASD. Two-sided p<0.05 was considered statistically significant.
A total of 86 patients (38 male and 48 female) were included in the control group. Meanwhile, 111 patients (39 male and 72 female) were included in the FJOA group. The average age of the control group was 56.31 (SD=12.06) years, that of the FJOA group was 62.40 (SD=9.35) years, and the differences were statistically significant (p<0.001). No significant differences were observed in sex, BMI, smoking, alcohol, and whether the two groups suffered from hypertension, diabetes, or coronary artery disease (Table 1). No statistically significant differences were noted between the two groups with respect to the ASA grade, operation time, blood loss, hospitalization stay, follow-up time, and whether the surgical segment had spondylolisthesis or instability (Table 1).
In facet joint Pathria and facet tropism, the interobserver agreement was substantial (╬║=0.806; 95% confidence interval [CI], 0.754ŌĆō0.858; p<0.001; ╬║=0.785; 95% CI, 0.693ŌĆō0.877; p<0.001, respectively). Likewise, the interobserver agreements were substantial in disc Pfirrmann, spondylolisthesis, and spinal stability (╬║=0.746; 95% CI, 0.667ŌĆō0.825; p<0.001; ╬║=0.765; 95% CI, 0.635ŌĆō0.895; p<0.001; ╬║=0.790; 95% CI, 0.587ŌĆō0.993; p<0.001, respectively). On the contrary, the intraobserver agreement ranges from substantial to almost perfect (╬║=0.647ŌĆō0.922; p<0.001).
No significant difference was found in the preoperative clinical pain scores and function scores (Table 2). The median VAS scores and median VAS improvement rates of low back pain in the control group were 0 (IQR=2) and 100% (IQR=57.50%), respectively, which were significantly less than that in the FJOA group (1 [IQR=1] and 66.67% [IQR=40.48%]), respectively, at the final follow-up (p<0.05). The low back pain improvement rate in the FJOA group was lower than that in the control group (40% versus 59%). However, the VAS score and VAS improvement rates of leg pain were not significantly different between the two groups (Table 2). No significant difference was observed in the ODI score, ODI improvement rate, and SF-36 (PF) score at the last follow-up between the two groups. According to the modified MacnabŌĆÖs criteria, 84.9% and 89.2% of the patients were excellent or good in the two groups, respectively, which showed no significant difference (Table 2). Regardless of the grouping, the postoperative VAS scores of low back and leg pain were significantly lower than the preoperative VAS scores (p<0.001). Namely, clinical symptoms in both groups improved after surgery.
Preoperatively, no statistically significant differences were observed in whether the surgical segment had spondylolisthesis or instability between the two groups. On the L2/3 and L3/4 levels, the degenerative grade of the facet joints positively correlated with the disc degeneration grade (R=0.160 and 0.211, respectively). Meanwhile, FJOA positively correlated with facet tropism on the levels L1/2, L2/3, L3/4, and L4/5 (R=0.177, 0.243, 0.152, and 0.149, respectively). However, no significant correlation can be observed between disc degeneration and facet tropism on the L1ŌĆōS1 level.
At the final follow-up, 26 cases (30.2%) of postoperative RASD occurred in the control group and 54 (48.6%) in the FJOA group. The incidence of RASD in the control group was significantly lower than that in the FJOA group (p=0.034). No patients underwent reoperations at the adjacent level.
We divided the preoperative FJOA at the adjacent segment into the preoperative FJOA at the cranial adjacent segment and that at the caudal adjacent segment. Between the two groups at the cranial adjacent segment, significant differences can be observed in both the VAS score and VAS improvement rate of low back pain. Meanwhile, no significant difference was noted either in the VAS score or VAS improvement rate of low back pain between the two groups at the caudal adjacent segment (Table 3). Moreover, improvement rates of low back pain were significantly lower in patients with single-level fusion in the FJOA group than in the control group at the last follow-up (Table 3).
No significant differences in preoperative low back pain VAS, leg pain VAS, ODI, postoperative low back pain VAS, leg pain VAS, ODI, SF-36 functional scores, improvement rates of low back pain VAS, improvement rate of leg pain VAS, and improvement rate of ODI were found between FJOA grades 1 and 2 by Pathria grade (p>0.05). Likewise, no significant differences were observed between grades 3 and 4 in these clinical scores. No significant difference in postoperative RASD was found between grades 1 and 2 by Pathria grade (p>0.05). The difference was not observed in grades 3 and 4.
Multivariate logistic regression analysis was performed by including sex, age, hypertension, fusion number, preoperative adjacent facet joint grade, facet joint tropism, adjacent disc degeneration grade, and other factors. The preoperative adjacent FJOA grade and age >60 years factors influencing whether patients had significant low back pain relief after surgery, with OR (95% CI) of 0.402 (0.212ŌĆō0.762) and 0.691 (0.498ŌĆō0.958), respectively, indicating that old patients with severe preoperative adjacent FJOA were less likely to achieve significant remission of low back pain >2 years after lumbar fusion (Table 4).
Multivariable logistic regression analysis revealed that the preoperative adjacent FJOA grade (OR, 1.406; 95% CI, 1.020ŌĆō1.939; p=0.038) and age >60 years (OR, 1.942; 95% CI, 1.024ŌĆō3.684; p=0.042) were significant risk factors for postoperative RASD (Table 5).
Posterior lumbar fusion is considered the gold standard treatment for lumbar degenerative diseases such as spondylolisthesis, lumbar instability, and lumbar spinal stenosis. However, after lumbar fusion, biomechanical changes can cause degeneration of adjacent facet joints or intervertebral discs, and the resulting ASD often affects the clinical efficacy.
Previously, clinicians have noticed the correlation between preoperative adjacent degeneration and postoperative efficacy of lumbar fusion and postoperative ASD occurrence. Sun et al. [11] found that the degree of adjacent spinal stenosis had no significant effect on the operation time and intraoperative blood loss, but prolonged the hospital stay of patients, and was more likely to have ASD in short-term follow-up. Another prospective study demonstrated that compared with patients without preoperative adjacent degeneration, patients with preoperative adjacent spinal stenosis or disc degeneration had lower JOA scores at follow-up, and the degree of adjacent spinal stenosis was aggravated after surgery, indicating that preoperative adjacent degeneration would significantly affect the early postoperative clinical efficacy of patients and increase the risk of postoperative ASD [14]. At present, most studies have focused on factors such as disc degeneration and spinal stenosis. Pinto et al. [15] and Okuda et al. [9] have confirmed that the preoperative sagittal direction of adjacent facet joints will affect the postoperative clinical efficacy, and when the tendency of bilateral facet joints increases, ASD and more serious clinical symptoms are more likely to occur following surgery. Furthermore, Choi et al. [16] also demonstrated that patients with adjacent degeneration had more severe preoperative FJOA than those without adjacent degeneration.
The results of this study showed that lumbar fusion improved the degree of low back pain, leg pain and ODI functional index; however, compared with the control group, the FJOA group had more severe low back pain and lower remission rates of low back pain >2 years following lumbar fusion and were more likely to experience RASD postoperatively. However, no significant difference was found in the postoperative ODI and SF-36 functional scores between the two groups, which may be because patients had undergone fusion of the main culprit segment during surgery, and postoperative dysfunction had been significantly improved. While the degeneration of the adjacent area could lead to pain, it had little effect on daily living function. On the contrary, no significant difference was found in the preoperative adjacent FJOA group in terms of hospital stay, operation time, and intraoperative blood loss, suggesting that even if the patient had more severe preoperative adjacent FJOA, the operation time may not be prolonged, blood loss may not be increased, and hospital stay will not be prolonged excessively. Interestingly, the severity of the degeneration of the cranial adjacent facet joints had a significant effect on the improvement of low back pain after surgery; however, this phenomenon was not present in the caudal adjacent facet joints, which suggests that surgeons should pay more attention to cranial adjacent degeneration.
The subgroup analysis found no significant difference in the improvement rate of low back pain between the control group and the FJOA group in multilevel fusions, whereas a significant difference in the improvement rates of low back pain was noted between the two groups in single-level fusions. These results suggest that preoperative adjacent segment FJOA has no significant effect on postoperative outcomes of multilevel fusion because the spine tends to be more stable after multilevel fusion, which addresses the symptoms caused by multilevel lesions in patients. Moreover, FJOA leads to facet joint capsule laxity, decreasing vertebral stability, and micromotion, which stimulates neuropathic pain in the sinuvertebral nerves and posteromedial branch of the spinal nerves. The adjacent segment in multilevel fusion is usually the upper lumbar or thoracic or sacral spine with high vertebral stability [17]. Therefore, patients with adjacent segment FJOA did not experience significant low back pain after multilevel fusion, whereas patients with adjacent segment FJOA had not experienced significant improvement in low back pain before single-level fusion.
This study also determined that the grade of degeneration of the adjacent facet joints on preoperative CT was an important factor for whether low back pain was relieved >2 years after lumbar fusion. Preoperative adjacent segment FJOA may predict poor relief of low back pain and is the most important risk factor for RASD. Kim et al. [18] reported facet joint degeneration as a significant factor in predicting postoperative ASD. The presence of adjacent FJOA indicated a possibility of instability. Particularly, the abnormal load and increased instability applied to the adjacent zone after lumbar fusion surgery may explain the occurrence of adjacent zone degeneration. The outcome of FJOA is restabilization, i.e., the progression of a narrow facet joint space with osteophyte proliferation. The severity of FJOA is related to vertebral instability, which accelerates the degeneration of adjacent joints. A previous study showed that facet joint tropism and shearing force on the facet joints of both sides of the lumbar spine were unbalanced, increasing the possibility of patients developing ASD after surgery [19]. However, the facet joint tropism was not statistically significantly associated with ASD in this study, which may be due to the small sample size or selection bias.
However, the incidence of postoperative RASD in this study was 30.2%ŌĆō45%, that is, a relatively moderate level, which was relatively lower than the incidence of postoperative RASD reported to be as high as >50%. On the contrary, we evaluated the postoperative RASD in patients only through the X-ray images of the lumbar vertebra, whereas the definition and diagnosis of RASD have gone beyond simple X-ray indicators and must develop from X-ray, CT, and MRI to comprehensive indicators. If only radiography is used for diagnosis, disc degeneration can be indirectly judged by the narrowing of the intervertebral space or spur formation. However, because radiography cannot estimate the degree of adjacent SCS, the incidence of ASD can be easily underestimated; thus, taking lumbar MR is necessary for further discrimination [20]. However, owing to the difference in the time points of lumbar X-ray reexamination, some patients have not yet experienced imaging ASD during early postoperative radiographic reexamination, resulting in a low incidence of postoperative RASD.
FJOA, as one of the lumbar degenerative changes, is closely related to age, which is also verified in this study, and patients in the preoperative adjacent FJOA group were relatively older than those in the control group. The lumbar spine is a global structure; thus, the degeneration of the intervertebral disc, ligament, vertebral body, facet joint, and other structures is a continuous correlation process. A positive correlation was found between FJOA and intervertebral disc degeneration only in L2/3 and L3/4, which is similar to the conclusion of previous studies [21]. However, the correlation between FJOA and facet joint tropism showed statistical significance at L1ŌĆōL4 levels, whereas Grogan et al. [22] and Boden et al. [23] suggested that lumbar facet joint tropism did not accelerate FJOA. They reported no significant difference in FJOA between facet joints with and without tropism; however, many limitations are associated with this study, which is based on a small number of cadaveric specimens and a smaller number of lumbar facet joints showing facet tropism and does not consider the level at which tropism occurs. The relationship between facet tropism and disc degeneration is debatable. Vanharanta et al. [24] reported no significant correlation between facet joint tropism and disc degeneration. However, Noren et al. [25] suggested that facet tropism could increase the risk of disc degeneration. In the present study, no significant correlation was observed between facet joint tropism and L1ŌĆōS1 disc degeneration.
Based on the results of this study, the postoperative clinical efficacy of patients and the risk of RASD can be evaluated according to the preoperative degree of FJOA adjacent to the fusion segments. Therefore, to improve the postoperative clinical efficacy of patients and prevent postoperative RASD, the overall degeneration of the spine must be evaluated.
This study has several limitations. This retrospective cohort study is limited to data available in the patientŌĆÖs medical records. Only a single center was involved, and the sample size of cases was relatively small. Some patients who lacked corresponding preoperative imaging data were excluded; however, this may lead to reduced generalizability. Additional prospective multicenter large-sample studies are necessary to confirm these results. Moreover, the control group was younger than the FJOA group, which introduced the confounding factor of age. However, this phenomenon can be explained by adjacent degenerative factors related to age. Moreover, some patients had a relatively short follow-up time.
In addition, only postoperative RASD was assessed, not the incidence of CASD, which has a greater effect on the clinical presentation of patients. Because it is difficult for patients to distinguish whether low back and leg pain is new or pre-existing after surgery during follow-up, the incidence of CASD was not discussed in this study.
Preoperative FJOA in adjacent segments can significantly affect the outcomes of lumbar fusion surgery (particularly single-segment fusion), mainly in low back pain. Patients with preoperative adjacent FJOA were more likely to have postoperative ASD at the early follow-up. Thus, spine surgeons should evaluate facet joint degeneration of the operational and adjacent segments of each patient. Appropriate postoperative or intraoperative treatment of adjacent facet joints is necessary, such as intraoperative small joint sealing or postoperative adjuvant physical therapy.
Acknowledgments
The authors would like to acknowledge the CT, MRI Department and Radiology Department of our hospital for their technical supports.
Notes
Author Contributions
LT, XD and RT contributed to the conception and design of the study. LT and RT contributed significantly to analysis and manuscript preparation. LT and XD performed the data analyses and wrote the manuscript; LZ and LR helped perform the analysis with constructive discussions. All authors read and approved the final manuscript.
Fig.┬Ā1
Flow chart of patientsŌĆÖ screening and grouping. MR, magnetic resonance; CT, computed tomography; FJOA, facet joint osteoarthritis.
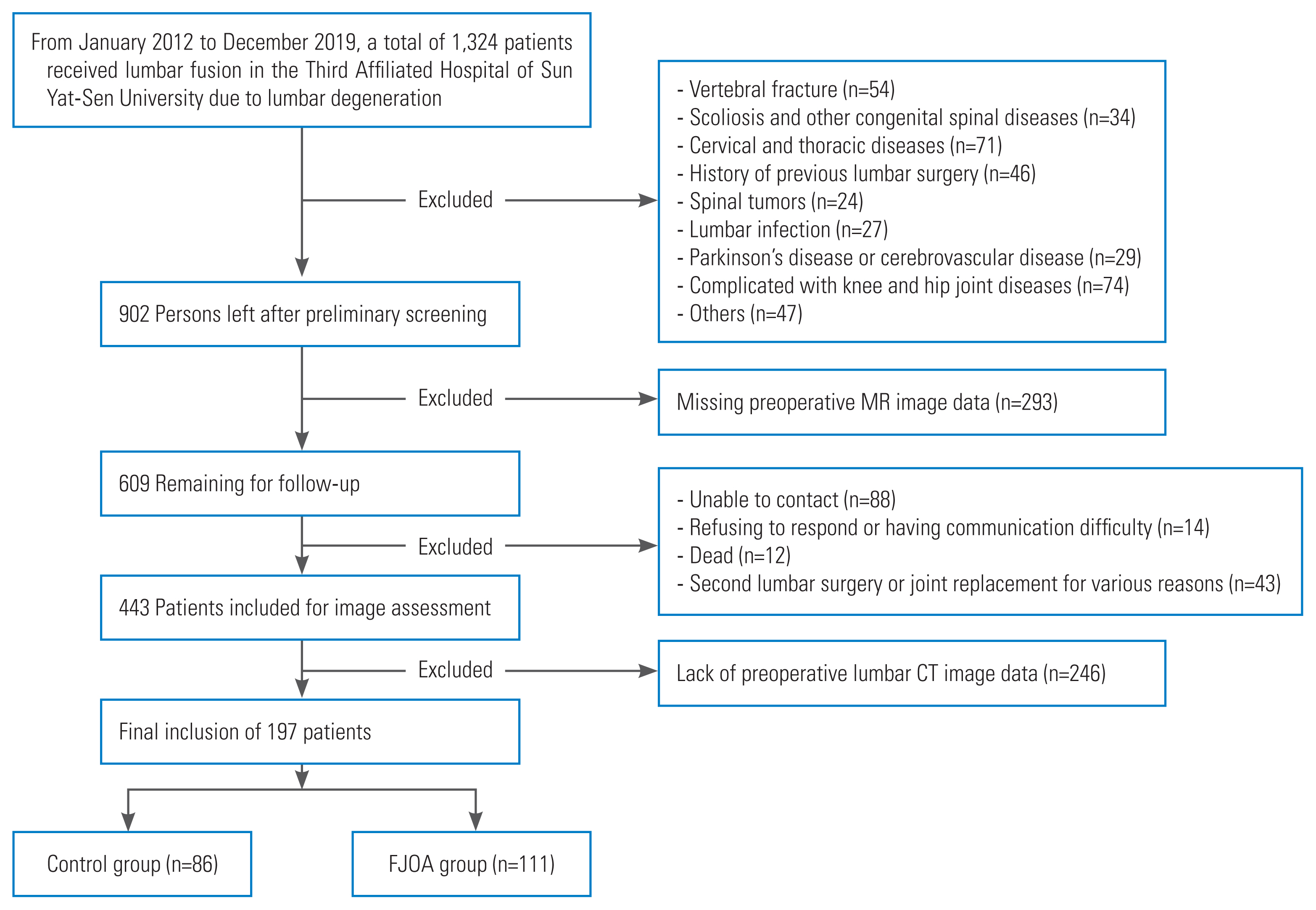
Fig.┬Ā2
Examples of computed tomography-evaluated facet joint osteoarthritis grades. (A) Grade 1 (normal): no joints space narrow (JSN) (2 mm or more); no osteophytes; no facet hypertrophy; no sclerosis or suspected sclerosis. (B) Grade 2 (mild osteoarthritis): JSN (joint space 1ŌĆō2 mm); and/or definite small osteophytes; and/or mild facet hypertrophy; and/or definite sclerosis. (C) Grade 3 (moderate osteoarthritis): JSN (joint space 1 mm); and/or moderate osteophytes; and/or moderate facet hypertrophy. (D) Grade 4 (severe osteoarthritis): severe JSN (bone-on-bone); large osteophytes; severe facet hypertrophy.
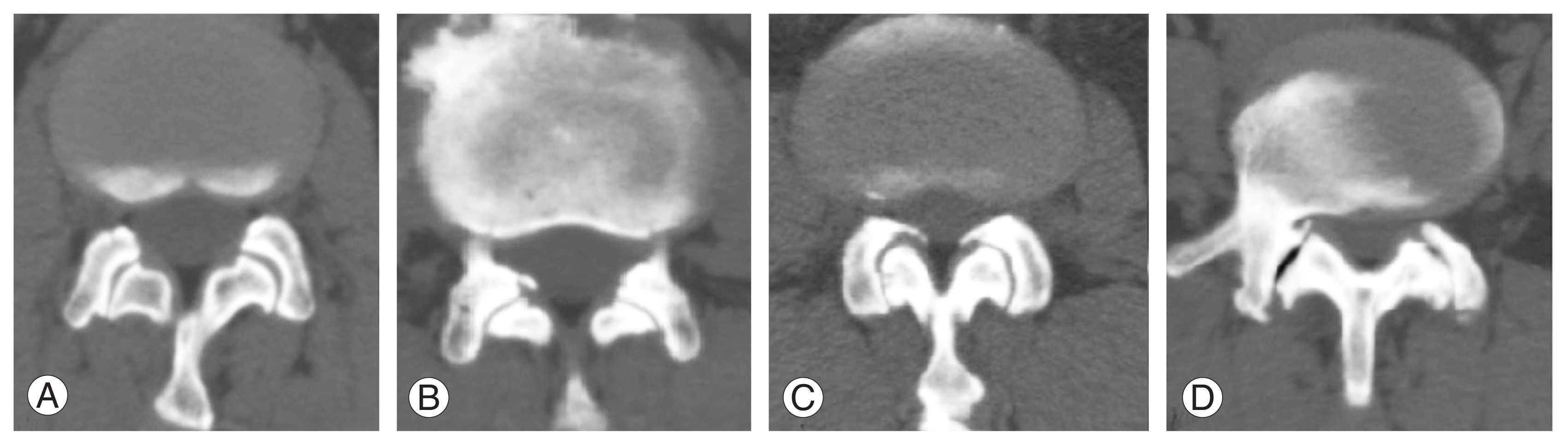
Fig.┬Ā3
PatientŌĆÖs postoperative adjacent segment degeneration on X-ray. Compared with preoperative lumbar X-ray (A), the patientŌĆÖs lumbar X-ray (B) more than 4 years after surgery showed that the upper adjacent intervertebral space was narrowed and the osteophyte was larger.
Table┬Ā1
Demographic characteristics of the patients
| Characteristic | Control group | FJOA group | p-value |
|---|---|---|---|
| Total | 86 | 111 | |
| Sex | 0.197 | ||
| ŌĆāMale | 38 | 39 | |
| ŌĆāFemale | 48 | 72 | |
| Age (yr) | 56.31┬▒12.06 | 62.40┬▒9.35 | <0.001* |
| Body mass index (kg/m2) | 24.73┬▒3.50 | 24.25┬▒3.65 | 0.387 |
| Smoking | 13 (15.1) | 12 (10.8) | 0.368 |
| Alcohol | 7 (8.1) | 2 (1.8) | 0.077 |
| Hypertension | 28 (32.6) | 36 (32.4) | 0.985 |
| Diabetes | 14 (16.3) | 19 (17.1) | 0.876 |
| Coronary artery disease | 5 (5.8) | 7 (6.3) | 0.886 |
| ASA | 0.287 | ||
| ŌĆā1 | 16 (19.8) | 17 (15.9) | |
| ŌĆā2 | 57 (70.4) | 71 (66.4) | |
| ŌĆā3 | 8 (9.9) | 19 (17.8) | |
| Surgical spondylolisthesis | 0.300 | ||
| ŌĆāYes | 44 (51.2) | 65 (58.6) | |
| ŌĆāNo | 42 (48.8) | 46 (41.4) | |
| Surgical instability | 0.887 | ||
| ŌĆāYes | 13 (18.6) | 17 (17.7) | |
| ŌĆāNo | 57 (81.4) | 79 (82.3) | |
| No. of fusion | 0.386 | ||
| ŌĆā1 | 67 (77.9) | 80 (72.1) | |
| ŌĆā2 | 13 (15.1) | 23 (20.7) | |
| ŌĆā3 | 6 (7.0) | 8 (7.2) | |
| Blood loss (mL) | 200 (IQR, 300) | 200 (IQR, 300) | 0.467 |
| Operation time (min) | 241.5 (IQR, 171.8) | 260 (IQR, 138) | 0.578 |
| Hospital stay (day) | 16 (IQR, 7) | 15 (IQR, 9) | 0.973 |
| Follow-up (mo) | 46 (IQR, 34) | 46 (IQR, 32) | 0.671 |
Table┬Ā2
Preoperative and postoperative disease clinical characteristic of the patients
| Variable | Control group | FJOA group | p-value |
|---|---|---|---|
| Preoperative | |||
| ŌĆāVAS score (low back) | 5 (IQR, 3) | 5 (IQR, 2.3) | 0.932 |
| ŌĆāVAS score (leg) | 5 (IQR, 3) | 4 (IQR, 1) | 0.764 |
| ŌĆāODI (%) | 42.86 (IQR, 23.06) | 42.22 (IQR, 24.00) | 0.956 |
| Postoperative | |||
| ŌĆāVAS score (low back) | 0 (IQR, 2) | 1 (IQR, 1) | 0.002* |
| ŌĆāVAS score (leg) | 0 (IQR, 2) | 0 (IQR, 2) | 0.637 |
| ŌĆāODI (%) | 7.33 (IQR, 19.44) | 8.89 (IQR, 17.78) | 0.407 |
| ŌĆāSF-36 (PF) (%) | 95 (IQR, 20) | 95 (IQR, 15) | 0.155 |
| ŌĆāImprovement rate of VAS score (low back) (%) | 100 (IQR, 57.50) | 66.67 (IQR, 40.48) | 0.006* |
| ŌĆāImprovement rate of VAS score (leg) (%) | 100 (IQR, 33.33) | 100 (IQR, 50.00) | 0.651 |
| ŌĆāImprovement rate of ODI (%) | 81.41 (IQR, 37.04) | 77.78 (IQR, 43.62) | 0.300 |
| ŌĆāSignificant relief of low back pain | 0.010* | ||
| ŌĆāŌĆāYes | 49 (59) | 42 (40) | |
| ŌĆāŌĆāNo | 34 (41) | 63 (60) | |
| ŌĆāRadiological adjacent segment degeneration | 0.009* | ||
| ŌĆāŌĆāYes | 26 (30.2) | 54 (48.6) | |
| ŌĆāŌĆāNo | 60 (69.8) | 57 (51.4) | |
Table┬Ā3
Subgroup analysis of improvement rate of low back pain
| Variable | Control group (%) | FJOA group (%) | p-value |
|---|---|---|---|
| Adjacent segment | |||
| ŌĆāCranial adjacent segment | 80 (53.57) | 60 (26.79) | 0.001* |
| ŌĆāCaudal adjacent segment | 71.43 (50.00) | 66.67 (42.86) | 0.349 |
| No. of fusion | |||
| ŌĆāSingle | 91.67 (50.00) | 66.67 (35.12) | 0.034* |
| ŌĆāMultiple | 100 (50.00) | 66.67 (48.21) | 1.000 |
| Fusion segment in single fusion | |||
| ŌĆāL4/5 | 83.33 (50.00) | 66.67 (33.33) | 0.082 |
| ŌĆāL5/S1 | 100 (70.83) | 55 (85.00) | 0.262 |
Table┬Ā4
Univariate and multivariate analysis for significant relief of low back pain more than 2 years after lumbar fusion
| Variable | Univariate | Multivariate | ||
|---|---|---|---|---|
|
|
|
|||
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Older than 60 yr | 0.337 (0.185ŌĆō0.661) | <0.001* | 0.402 (0.212ŌĆō0.762) | 0.005* |
|
|
||||
| Surgical time (/min) | 1 (0.998ŌĆō1.003) | 0.783 | 1.001 (0.998ŌĆō1.004) | 0.654 |
|
|
||||
| No. of fusion | 0.84 (0.522ŌĆō1.350) | 0.471 | 0.87 (0.514ŌĆō1.475) | 0.606 |
|
|
||||
| Follow-up time (/mo) | 1.002 (0.989ŌĆō1.016) | 0.734 | 1.004 (0.99ŌĆō1.019) | 0.56 |
|
|
||||
| Preoperative adjacent FJOA grade | 0.649 (0.479ŌĆō0.879) | 0.005* | 0.691 (0.498ŌĆō0.958) | 0.026* |
|
|
||||
| Preoperative adjacent facet joint tropism | 1.104 (0.754ŌĆō1.615) | 0.612 | 1.194 (0.797ŌĆō1.789) | 0.389 |
|
|
||||
| Preoperative adjacent disc degeneration grade | 0.811 (0.487ŌĆō1.351) | 0.42 | 0.984 (0.560ŌĆō1.729) | 0.955 |
Table┬Ā5
Univariate and multivariate analysis for radiological adjacent segment degeneration more than 2 years after lumbar fusion
| Variable | Univariate | Multivariate | ||
|---|---|---|---|---|
|
|
|
|||
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Older than 60 yr | 2.341 (1.295ŌĆō4.233) | 0.005* | 1.942 (1.024ŌĆō3.684) | 0.042* |
|
|
||||
| Surgical time (/min) | 0.999 (0.996ŌĆō1.001) | 0.321 | 0.992 (0.978ŌĆō1.006) | 0.27 |
|
|
||||
| No. of fusion | 1.06 (0.662ŌĆō1.698) | 0.807 | 0.998 (0.995ŌĆō1.001) | 0.271 |
|
|
||||
| Follow-up time (/mo) | 0.995 (0.982ŌĆō1.008) | 0.452 | 1.089 (0.647ŌĆō1.832) | 0.748 |
|
|
||||
| Preoperative adjacent FJOA grade | 1.496 (1.109ŌĆō2.019) | 0.008* | 1.406 (1.020ŌĆō1.939) | 0.038* |
|
|
||||
| Preoperative adjacent facet joint tropism | 0.943 (0.644ŌĆō1.379) | 0.761 | 0.87 (0.583ŌĆō1.298) | 0.494 |
|
|
||||
| Preoperative adjacent disc degeneration grade | 1.359 (0.827ŌĆō2.235) | 0.227 | 1.069 (0.621ŌĆō1.841) | 0.809 |
References
1. Cohen SP, Raja SN. Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet) joint pain. Anesthesiology 2007 106:591ŌĆō614.



2. Gellhorn AC, Katz JN, Suri P. Osteoarthritis of the spine: the facet joints. Nat Rev Rheumatol 2013 9:216ŌĆō24.




3. Perolat R, Kastler A, Nicot B, et al. Facet joint syndrome: from diagnosis to interventional management. Insights Imaging 2018 9:773ŌĆō89.




4. Guigui P, Ferrero E. Surgical treatment of degenerative spondylolisthesis. Orthop Traumatol Surg Res 2017 103(1S): S11ŌĆō20.


5. de Kunder SL, Rijkers K, Caelers IJ, de Bie RA, Koehler PJ, van Santbrink H. Lumbar interbody fusion: a historical overview and a future perspective. Spine (Phila Pa 1976) 2018 43:1161ŌĆō8.

6. Zhu D, Li W, Chen Z, et al. Analysis of long-term efficacy and influencing factors after decompression, fixation and fusion for lumbar spinal stenosis. Chin J Spine Spinal Cord [Internet] 2013 [cited 2023 Apr 20]. 23:865. ŌĆō71. Available from: https://doi.org/10.3969/j.issn.1004-406X.2013.10.01
7. Nakashima H, Kawakami N, Tsuji T, et al. Adjacent segment disease after posterior lumbar interbody fusion: based on cases with a minimum of 10 years of follow-up. Spine (Phila Pa 1976) 2015 40:E831ŌĆō41.

8. Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 2004 4(6 Suppl): 190SŌĆō194S.


9. Okuda S, Iwasaki M, Miyauchi A, Aono H, Morita M, Yamamoto T. Risk factors for adjacent segment degeneration after PLIF. Spine (Phila Pa 1976) 2004 29:1535ŌĆō40.


10. Hikata T, Kamata M, Furukawa M. Risk factors for adjacent segment disease after posterior lumbar interbody fusion and efficacy of simultaneous decompression surgery for symptomatic adjacent segment disease. J Spinal Disord Tech 2014 27:70ŌĆō5.


11. Sun Z, Li Z, Guo Y, et al. Evaluation of adjacent segment with pre-existing degeneration using the cerebrospinal fluid occlusion sign on MRI before posterior lumbar fusion: a multi-center observational cohort study. Global Spine J 2023 13:745ŌĆō51.




12. Pathria M, Sartoris DJ, Resnick D. Osteoarthritis of the facet joints: accuracy of oblique radiographic assessment. Radiology 1987 164:227ŌĆō30.


13. Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 2001 26:1873ŌĆō8.


14. Sun Z, Li W, Guo Y, et al. Effect of pre-existing adjacent segment degeneration on short-term effectiveness after lumbar fusion surgery. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2019 33:837ŌĆō44.


15. Pinto EM, Teixeria A, Frada R, et al. Patient-related risk factors for the development of lumbar spine adjacent segment pathology. Orthop Rev (Pavia) 2021 13:24915.



16. Choi KC, Kim JS, Shim HK, Ahn Y, Lee SH. Changes in the adjacent segment 10 years after anterior lumbar interbody fusion for low-grade isthmic spondylolisthesis. Clin Orthop Relat Res 2014 472:1845ŌĆō54.



17. Izzo R, Guarnieri G, Guglielmi G, Muto M. Biomechanics of the spine. Part I: spinal stability. Eur J Radiol 2013 82:118ŌĆō26.


18. Kim JY, Ryu DS, Paik HK, et al. Paraspinal muscle, facet joint, and disc problems: risk factors for adjacent segment degeneration after lumbar fusion. Spine J 2016 16:867ŌĆō75.


19. Okuda S, Oda T, Miyauchi A, et al. Lamina horizontalization and facet tropism as the risk factors for adjacent segment degeneration after PLIF. Spine (Phila Pa 1976) 2008 33:2754ŌĆō8.


20. Cheh G, Bridwell KH, Lenke LG, et al. Adjacent segment disease followinglumbar/thoracolumbar fusion with pedicle screw instrumentation: a minimum 5-year follow-up. Spine (Phila Pa 1976) 2007 32:2253ŌĆō7.

21. Bashkuev M, Reitmaier S, Schmidt H. Relationship between intervertebral disc and facet joint degeneration: a probabilistic finite element model study. J Biomech 2020 102:109518.


22. Grogan J, Nowicki BH, Schmidt TA, Haughton VM. Lumbar facet joint tropism does not accelerate degeneration of the facet joints. AJNR Am J Neuroradiol 1997 18:1325ŌĆō9.


23. Boden SD, Riew KD, Yamaguchi K, Branch TP, Schellinger D, Wiesel SW. Orientation of the lumbar facet joints: association with degenerative disc disease. J Bone Joint Surg Am 1996 78:403ŌĆō11.

- TOOLS







