 |
 |
- Search
| Asian Spine J > Volume 10(2); 2016 > Article |
Abstract
Study Design
Retrospective follow-up study on the result of surgical treatment for patients with degenerative lumbar spondylolisthesis (DLS) using cortical bone trajectory (CBT) technique.
Overview of Literature
CBT is a recently advocated, novel, less-invasive technique of lumbar pedicle screw, which provides enhanced screw purchase by maximizing the thread contact with higher density bone surface. Despite the frequent use of CBT technique in the lumbar spine surgery, little is known of the capability of this technique to manage patients with DLS.
Methods
Thirty two consecutive patients (5 males, 27 females) surgically treated with single-level DLS in our institute using CBT were included. All patients were followed up at least 12 months (mean 24 months). Their clinical and radiological features were measured.
Results
Good leg pain relief was achieved in all patients. The mean postoperative percentage slip demonstrated significant reduction with significant neurological recovery when compared with preoperative percentage slip, and it was maintained until the latest follow-up. Loss of correction of more than 3 mm during the follow-up period was observed in 3 cases. Surgical site infection was observed in one case; however, pull-out of PSs or neurological deterioration was not found. No patient needed additional surgery during the follow-up period.
Cortical bone trajectory (CBT) is a recently advocated technique of lumbar pedicle screw (PS) trajectory [1]. This novel technique achieves maximum contact with the cortical bone through the pedicle to the vertebral body by a new trajectory that follows a caudal-to-cephalad path in the sagittal plane and a medial-to-lateral directed path in the transverse plane (Fig. 1). Its medial screw entry point allows minimal soft tissue dissection compared with the traditional trajectory (TT) technique. CBT increases screw purchase with reduced invasiveness [12].
Despite the wide-spread indication of the CBT technique in thoracolumbar spine surgery [345], most reports concerning CBT were biomechanical evaluations [267] or technical notes [345]. No study has exclusively evaluated the capability of this technique to manage patients with degenerative lumbar spondylolisthesis (DLS). In the present report, we evaluated the capability and short-term results of this novel CBT technique for the treatment of patients with DLS, especially from the point of view of effective reduction of slipped vertebra.
Thirty two consecutive patients (5 males, 27 females) with single-level DLS in our institute using the CBT technique from August 2012 to May 2014 were included. All patients were followed up at least 12 months (mean 24 months). Mean age at the time of surgery was 68 years (range, 51ŌĆō84 years). Levels of DLS were L3 in 10 cases and L4 in 22 cases. Twenty patients were Grade I and 12 were Grade II according to the Meyerding criteria [8]. Indication of surgical treatment was neurological compromise, intermittent claudication, and/or intractable lower leg pain with or without low-back pain after adequate conservative treatment. Our Institutional Review Board approved this study.
All procedures were done by two experienced spine surgeons (K.M. and K.N.). Briefly, after exposure of laminae by spinous process splitting, neural decompression with bilateral total facetectomy was done to achieve wide exposure of the disc space and the neural elements to prevent possible nerve root impingements, while preserving the area PS entry. Solera PSs with a diameter of 5.5 mm and length of 35ŌĆō40 mm (Medtronic, Memphis, TN, USA) were placed under fluoroscopy guidance by CBT as described previously [24] with slight modifications. Briefly, the upper corner of the vertebra in the anterior-posterior view and upper endplate of the posterior one-third area was targeted to gain significant medial-to-lateral and caudal-to-cephalad angle under fluoroscopy control. The screw length was measured by a probe inserted along with screw trajectory.
Reduction screws were used for slipped vertebrae. Subsequently, the total discectomy consisted of excision of the anulus and cartilaginous end plate was performed as much as possible, whereas the osseous end plate was preserved. Interbody fusion was then performed by placing the polyetheretherketone (PEEK) cage(s), which were filled by bone chips that had been trimmed from the resected local bones. In the first 10 cases in this series, one boomerang-type Milestone PEEK cage (Medtronic) was used. The OIC PEEK two box-type cages (Stryker, Kalamazoo, MI, USA) were used subsequently. Bilateral rods were fixed PSs inserted to caudal vertebra first, and then the slipped vertebra was gently lifted by tightening the bilateral rods towards the reduction screws inserted to the cranial slipped vertebra. The PSs were compressed to restore the natural lumbar lordosis. Finally, the system was reinforced by cross-linkage and completed posterior lumbar interbody fusion (PLIF). A representative case is shown in Fig. 2. A canvas corset was worn for 2 months after the surgery.
To evaluate the neurological condition of each patient, Japan Orthopaedic Association (JOA) score (range, 0ŌĆō29) [9] was employed. Preoperative, postoperative (one month after the surgery), and latest follow-up JOA scores were assessed.
The magnitude of spondylolisthesis was determined according to prior criteria [8] and the Taillard procedure [10]. Preoperative, postoperative, and latest follow-up percent (%) of slip were measured. In turn, lumbar lordosis (LL, in degrees) at L1 to S1, and lordosis at fused segment (focal lordosis, FL) were determined in relaxed standing position standard radiographs [11]. More than 3 mm of sagittal translation in lateral standard radiographs of lumbar spine were considered as a loss of correction. Apparent nonunion at the time of 12 months after the surgery was determined as more than 3 degrees of rotational instability at the fused segment in dynamic (flexion-extension) lateral standard radiographs of lumbar spine, and an obvious clear zone around PSs or cage(s) on computed tomography (CT).
Good leg pain relief was achieved in all patients without neurological deterioration. The mean postoperative (25┬▒2.0) and latest follow-up JOA scores (25┬▒1.8) were demonstrated significant recovery when compared with the mean preoperative scores (12┬▒4.9) (Table 1).
The mean postoperative % slip (2.7%┬▒4.8%) demonstrated significant reduction when compared with preoperative % slip (23%┬▒5.2%) (p<0.01). This good reduction of slipped vertebrae was maintained until the time of latest follow-up (3.8%┬▒6.7%). In turn, preoperative mean LL (26┬▒10 degrees) and FL (3.0┬▒6.2 degrees) were significantly restored to 40┬▒10 degrees and 10┬▒5.3 degrees, respectively, and were maintained until the latest follow-up (LL, 37┬▒11 degrees; FL, 9.6┬▒5.8 degrees) (Table 1).
Loss of correction was observed in 3 cases (9.4%). However, loss was not associated with clinical symptoms (Fig. 3). All 3 cases developed loss of correction within one month after the surgery; however, bone fusion was confirmed 1 year after surgery. SSI was observed in one case that was completely recovered by one-time debridement and antibiotic therapy without removal of the implants. Pull-out of PSs and pedicle fracture were not found. At the 12-month follow-up, 3 cases (9.4%) of apparent nonunion were evident, i.e., clear zone around cages on CT. They were not associated with clinical symptoms or loss of correction. No patient needed additional surgery during the follow-up period.
The present study reveals that CBT technique is useful to reduce slippage of vertebrae and to maintain the restored alignment with significant neurological recovery for at least 12-months (mean 24-months) postoperatively. Loss of correction exceeding 3 mm during the follow-up period was observed in 3 of the first 10 cases. Apparent loosening of PS was not found in these cases. Follow-up CT 1 year from surgery revealed bone fusion with cage malposition. Cage malposition due to our technical error (osseous endplate violence during the cage placement) was the most likely cause of the loss of correction (Fig. 3). Subsequently, we used two box-type cages with careful cage positioning and did not encounter this problem. Apparent nonunion at 12 months after the surgery evident as a clear zone around cages on CT was found in 3 cases (9.4%). However, this was not associated with clinical symptoms or loss of correction.
It is difficult to directly compare the nonunion rate of the present study with other results because universally approved radiological criteria for interbody fusion have not been established. However the nonunion rate in the present study appears relatively high compared to PLIF by TT technique, which nears 100% [1213]. Three cases (9.4%) with nonunion fulfilled one nonunion criterion (clear zone around cages on CT) 12 months after the surgery. The clear zone around cages evident on CT is a hot topic in this field. The possible impact of the PEEK cage on the clear zone around cages was advocated, even though we used the TT technique [13]. However, the precise mechanism remains unknown. Further studies are warranted to elucidate the cause of clear zone around cages. We continue careful follow-up of our patients to see whether complete bony fusion develops or not.
The optimal surgical treatment of DLS has not been established yet. Decompression surgery without spinal fusion has achieved good clinical results in patients with DLS [1415]. However, it is not always indicated for patients with DLS [16]. A variety of factors including instability and/or disc degeneration of the level of spondylolisthesis, spinal alignment, and severity of spinal canal stenosis can be present. Appropriate surgical treatments including spinal fusion surgeries should be indicated.
Spinal balance, especially sagittal balance, is an important issue for spinal surgeons. Several authors suggested that correction of sagittal imbalance plays a critical role in short- and long-term outcomes in adult spinal deformity [1718]. A positive correlation between improved local lordosis at the fused segment due to the reduction of slippage and recovery rate of JOA score of the patients with DLS managed by posterolateral fusion has been described [16]. Restored sagittal balance contributes to good clinical outcomes in patients with DLS [1219]. In addition, a very recent literature review advocated the significant relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal diseases including DLS [20].
Biomechanical studies using cadaveric spines have shown that local sagittal alignment of fused segment after lumbar fusion surgery appreciably influences the adjacent levels [2122]. Evaluation of the motion of adjacent segments after L4/5 fusion in different sagittal alignment revealed that hypolordortic alignment at L4/5 yielded significantly greater flexion-extension motion at L3/4 compared with intact specimen, in situ or hyperlordortic fixation [21]. In turn, hyperlordortic alignment at L4/5 yielded significantly greater flexion-extension motion at L5/S1 compared with intact specimen but not in situ or hypolordortic fixation. Hypolordosis in the instrumented segment can cause increased loading of the posterior column of the adjacent segments [22]. These clinical and basic findings suggest that we have to pay serious attention to gain appropriate sagittal balance when performing spinal fusion surgeries. In the present study, we could restore both LL and FL by PLIF with the CBT technique.
Alternatively, PSs are the most common and reliable tools for the correction of the spinal deformities as well as spinal fusion. However, screw loosening is a well-known unresolved problem, especially in patients with osteoporosis [123]. CBT has enhanced screw purchase due to its unique screw trajectory promising maximum contact of screw with higher-density bone regions [67]. A cadaveric biomechanical study revealed a 30% increase in uniaxial pullout load of CBT compared with that of the TT [1]. Furthermore, the CBT technique has significantly superior resistance to craniocaudal toggling, which simulates more physiological condition than uniaxial pullout test, compared with that of TT [7]. An in vivo study evaluated the final insertional torque [6], which is a good indicator of initial screw stability [2425] and pullout strength [25]. CBT produced a 2-fold higher insertional torque than TT [6].
In patients with osteoporosis, cortical bone is relatively preserved [26]. In turn, the bone density of the CBT pathway is significantly high [1]. Accordingly, the CBT technique may be most advantageous in patients with poorly trabeculated osteoporotic bone [67]. It is well-known that most of patients with DLS who need surgical treatment are elderly females. In the present study, 27 of 33 patients (82%) were females with a mean age at the time of surgery of 69 years. CBT also has the other several advantages over TT that include safety and reduced invasiveness [67]. Taking all these findings into account, it is rational to prefer the CBT technique for the surgical treatment of DLS.
A hybrid technique of CBT was recently reported for cranial slipped vertebra, whereas TT for caudal non-slipped vertebra is used for the treatment of DLS [5]. Although the study involved a small number of cases (n=6) with only a 3-month follow-up, the authors described that the CBT screwing produced sufficient holding power of the slipped vertebrae [5].
To the best of our knowledge, the present study is the first report of genuine CBT technique indicated for the management of patients with DLS. Even though the present study is also preliminary, with mean 24-month (minimum 12-month) follow-up, we found that this technique is useful for the treatment of DLS.
Limitations of the present study are the short follow-up, limited number of cases, and the lack of a control arm. However, since the CBT technique is a newly-advocated procedure, middle- and long-term results remain to be assessed. Longer follow-up studies are therefore needed to elucidate the clinical utility of the CBT technique.
Conflict of Interest
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
1. Santoni BG, Hynes RA, McGilvray KC, et al. Cortical bone trajectory for lumbar pedicle screws. Spine J 2009;9:366ŌĆō373. PMID: 18790684.


2. Matsukawa K, Yato Y, Nemoto O, Imabayashi H, Asazuma T, Nemoto K. Morphometric measurement of cortical bone trajectory for lumbar pedicle screw insertion using computed tomography. J Spinal Disord Tech 2013;26:E248ŌĆōE253. PMID: 23429319.


3. Matsukawa K, Yato Y, Hynes RA, et al. Cortical bone trajectory for thoracic pedicle screws: a technical note. J Spinal Disord Tech 2014 7 29 [Epub]. PMID: 10.1097/BSD.0000000000000130.


4. Matsukawa K, Yato Y, Kato T, Imabayashi H, Asazuma T, Nemoto K. Cortical bone trajectory for lumbosacral fixation: penetrating S-1 endplate screw technique: technical note. J Neurosurg Spine 2014;21:203ŌĆō209. PMID: 24766288.


5. Takata Y, Matsuura T, Higashino K, et al. Hybrid technique of cortical bone trajectory and pedicle screwing for minimally invasive spine reconstruction surgery: a technical note. J Med Invest 2014;61:388ŌĆō392. PMID: 25264059.


6. Matsukawa K, Yato Y, Kato T, Imabayashi H, Asazuma T, Nemoto K. In vivo analysis of insertional torque during pedicle screwing using cortical bone trajectory technique. Spine (Phila Pa 1976) 2014;39:E240ŌĆōE245. PMID: 24253778.


7. Baluch DA, Patel AA, Lullo B, et al. Effect of physiological loads on cortical and traditional pedicle screw fixation. Spine (Phila Pa 1976) 2014;39:E1297ŌĆōE1302. PMID: 25099320.


8. Meyerding HW. Spondylolisthesis. Surg Gynecol Obstet 1932;54:371ŌĆō379.
9. Inoue S, Izumida S. Assessment of treatment for low back pain: Japanese Orthopaedic Association. J Jpn Orthop Assoc 1986;60:391ŌĆō394.
10. Taillard W. Spondylolisthesis in children and adolescents. Acta Orthop Scand 1954;24:115ŌĆō144. PMID: 13217798.


11. Cobb J,Outline for the study of scoliosis. American Academy of Orthopaedic Surgeons, editors. Instructional course lectures. Ann Arbor, Mich.: J.W. Edwards; 1948. p.261ŌĆō275.
12. Sears W. Posterior lumbar interbody fusion for degenerative spondylolisthesis: restoration of sagittal balance using insert-and-rotate interbody spacers. Spine J 2005;5:170ŌĆō179. PMID: 15749617.


13. Nemoto O, Asazuma T, Yato Y, Imabayashi H, Yasuoka H, Fujikawa A. Comparison of fusion rates following transforaminal lumbar interbody fusion using polyetheretherketone cages or titanium cages with transpedicular instrumentation. Eur Spine J 2014;23:2150ŌĆō2155. PMID: 25015180.


14. Kleeman TJ, Hiscoe AC, Berg EE. Patient outcomes after minimally destabilizing lumbar stenosis decompression: the "Port-Hole" technique. Spine (Phila Pa 1976) 2000;25:865ŌĆō870. PMID: 10751299.


15. Herron LD, Trippi AC. L4-5 degenerative spondylolisthesis. The results of treatment by decompressive laminectomy without fusion. Spine (Phila Pa 1976) 1989;14:534ŌĆō538. PMID: 2727798.


16. Kawakami M, Tamaki T, Ando M, Yamada H, Hashizume H, Yoshida M. Lumbar sagittal balance influences the clinical outcome after decompression and posterolateral spinal fusion for degenerative lumbar spondylolisthesis. Spine (Phila Pa 1976) 2002;27:59ŌĆō64. PMID: 11805637.


17. Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 2005;30:682ŌĆō688. PMID: 15770185.


18. Schwab F, Ungar B, Blondel B, et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976) 2012;37:1077ŌĆō1082. PMID: 22045006.


19. Kim MK, Lee SH, Kim ES, Eoh W, Chung SS, Lee CS. The impact of sagittal balance on clinical results after posterior interbody fusion for patients with degenerative spondylolisthesis: a pilot study. BMC Musculoskelet Disord 2011;12:69PMID: 21466688.




20. Le Huec JC, Faundez A, Dominguez D, Hoffmeyer P, Aunoble S. Evidence showing the relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal diseases: a literature review. Int Orthop 2015;39:87ŌĆō95. PMID: 25192690.


21. Akamaru T, Kawahara N, Tim Yoon S, et al. Adjacent segment motion after a simulated lumbar fusion in different sagittal alignments: a biomechanical analysis. Spine (Phila Pa 1976) 2003;28:1560ŌĆō1566. PMID: 12865845.


22. Umehara S, Zindrick MR, Patwardhan AG, et al. The biomechanical effect of postoperative hypolordosis in instrumented lumbar fusion on instrumented and adjacent spinal segments. Spine (Phila Pa 1976) 2000;25:1617ŌĆō1624. PMID: 10870136.


23. Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K. Influence of bone mineral density on pedicle screw fixation: a study of pedicle screw fixation augmenting posterior lumbar interbody fusion in elderly patients. Spine J 2001;1:402ŌĆō407. PMID: 14588296.


24. Halvorson TL, Kelley LA, Thomas KA, Whitecloud TS 3rd, Cook SD. Effects of bone mineral density on pedicle screw fixation. Spine (Phila Pa 1976) 1994;19:2415ŌĆō2420. PMID: 7846594.


25. Zdeblick TA, Kunz DN, Cooke ME, McCabe R. Pedicle screw pullout strength. Correlation with insertional torque. Spine (Phila Pa 1976) 1993;18:1673ŌĆō1676. PMID: 8235848.


26. Richardson ML, Genant HK, Cann CE, et al. Assessment of metabolic bone diseases by quantitative computed tomography. Clin Orthop Relat Res 1985;(195): 224ŌĆō238. PMID: 3978956.

Fig.┬Ā1
Screw trajectories of traditional trajectory (TT, black arrows) and cortical bone trajectory (CBT, red broken arrows) technique. CBT follows a laterally directed (medial-to-lateral) path in the coronal (A) and axial (C) plane and caudal-to-cephalad path in sagittal (B) plane.
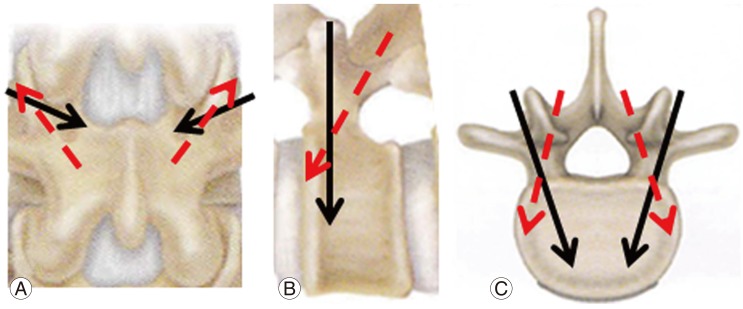
Fig.┬Ā2
Preoperative (A, B) and postoperative (C, D) standard radiographs of 62-year-old female patient with L4 degenerative lumbar spondylolisthesis. Standard radiographs, made 2 years postoperatively, show the good reduction of spondylolisthesis as well as improvement of the lumbar lordosis and focal lordosis of the fused segment.

Fig.┬Ā3
Preoperative (A, B), postoperative (C) and 1-month follow-up (D) standard radiographs of a 78-year-old female patient with L4 degenerative lumbar spondylolisthesis. Postoperative standard radiographs show good reduction of spondylolisthesis as well as overt cage malposition (C). Standard radiographs, made 1 month postoperatively show significant loss of correction with cage subsidence (D).








