|
 |
- Search
| Asian Spine J > Volume 8(6); 2014 > Article |
Abstract
Myxopapillary ependymoma in childhood typically occurs in the central nervous system. There are few surgical cases of myxopapillary ependymoma of the cauda equina in children. We report a case of myxopapillary ependymoma of the cauda equina in a 5-year-old boy, who presented with leg pain and abnormal gait. Subtotal resection surgery was performed. Following the subtotal tumor resection, follow-up magnetic resonance imaging evaluation showed a recurrent tumor. As a result, we performed a second subtotal tumor resection and followed with postoperative radiation therapy. No further evidence of the disease has been noted elsewhere in the patient in over ten years of follow-up. Myxopapillary ependymoma of the cauda equina in a young boy was improved by subtotal tumor resection and postoperative radiation therapy.
Myxopapillary ependymoma was first described as a subtype of ependymoma by Kernohan [1] in 1932. Myxopapillary ependymoma is a tumor that typically arises in the filum terminale and conus medullaris [1,2]. This tumor has a significantly better prognosis than other ependymomas, because it is slow-growing, unlikely to metastasize and does not tend to infiltrate neural tissues [3]. Intracranial ependymomas represent 6%-9% of primary central nervous system neoplasms and generally present in young children, with a mean age of four-year. Spinal myxopapillary ependymomas are rarer than intracranial types. Myxopapillary ependymomas generally present within the spinal canals of adults. Spinal myxopapillary ependymomas in children <5 years requiring surgery are very rare.
Here we describe a rare case of a 5-year-old boy who presented with cauda equina compression due to myxopapillary ependymoma, which was treated with subtotal resection and postoperative radiation therapy.
A 5-year-old boy presented with a history of right popliteal pain and abnormal gait that began after March 2000, four months prior to admission. Three months before admission, the patient visited a neighborhood hospital complaining of right popliteal pain, pain in the right hip and an abnormal gait. A magnetic resonance imaging (MRI) scan of the lumbar spine showed a tumor in the cauda equina. He was referred to our hospital and was admitted for examination. On admission he had no motor, sensory or urinary disturbances. Decreased tone and hyporeflexia in the lower extremities were observed. His medical history indicated no abnormalities. Radiographs revealed wide interpedicular distances in the lower lumbar vertebrae (Fig. 1). T2-weighted sagittal MRI showed a high-signal mass of cauda equina extending from L1 to L4 (Fig. 2). The mass was enlarged compared to that on the MRI performed at the neighborhood hospital. As such we performed subtotal resection with laminoplasty from T12 to L4. Histological findings from the tissue removed during surgery showed myxopapillary ependymoma with a positive margin (Fig. 3). Our attempt to perform radiation therapy could not proceed due to his parents' refusal of the therapy. A vesicorectal disorder occurred immediately after surgery, but it improved naturally over time.
Two years after admission, follow-up MRI revealed a recurrent enhanced tumor from L2 to L4, with a small seeding lesion at the sacral area (Fig. 4). There was a sensory deficit of analgesia from the L2 to L5 area. Leg pain and motor neuron deficits were not observed. We performed subtotal resection with laminectomy from L1 to L4 (Fig. 5). The tumor was tightly adhered to many bundles of the cauda equina, and several bundles were coursing through the tumor. Thus the tumor was only partially removed. Postoperative radiation therapy (45 Gy for the whole brain and spinal cord) was performed. After the second surgery, a urinary disorder occurred, which persists today.
MRI of the spine nine years after the second surgery showed no evidence of regrowth of the residual tumor (Fig. 6). Neutral standing radiographs ten years after the second surgery showed no spinal deformity (Fig. 7). No further evidence of the disease has been noted elsewhere in the patient in the ten-year of follow-up.
The patient and his family provided consent for data in this case to be published.
Myxopapillary ependymomas arise almost exclusively from the conus medullaris, cauda equina and filum terminale [1,2]. The World Health Organization (WHO) classifies ependymomas into the following four categories: subependymomas (WHO grade 1), myxopapillary ependymomas (WHO grade 1), ependymomas (WHO grade 2) and anaplastic ependymomas (WHO grade 3) [4]. Myxopapillary ependymomas are slow-growing tumors that may become very large before clinical detection, occasionally filling and expanding throughout the lumbosacral canal [5].
Myxopapillary ependymomas in children typically occur in the central nervous system. Therefore there are few cases of spinal myxopapillary ependymoma in children. There are some reports on surgical procedures used to treat spinal myxopapillary ependymoma. Nakamura et al. [6] and Quraishi et al. [7] reported the surgical outcomes of this tumor in patients of 14-58 years and patients of 20-50 years, respectively. The 5-year-old boy in the current report was the youngest of patients in the earlier reports.
Complete resection of myxopapillary ependymomas is associated with excellent long-term prognosis. However it is sometimes difficult to completely resect these tumors because of their tight adherence to the spinal cord and cauda equina. Al-Habib et al. [8] reviewed fifteen myxopapillary ependymoma patients (age range, 18-71 years). They reported that 17% of patients developed tumor regrowth requiring reoperations, while none of the patients with total resection developed recurrence.
The role of radiation therapy has not been adequately studied. Radiation therapy is likely warranted in cases of subtotal resection and recurrence of the intradural tumors, but is controversial in cases of total resection and extradural ependymomas [9]. In our case, the tumor recurred after the first surgery in the absence of postoperative radiation therapy. In contrast when postoperative radiation therapy was used following the second surgery, a relapse did not occur. As such radiation therapy is considered effective against myxopapillary ependymomas.
This patient represents a young case of spinal myxopapillary ependymoma of the cauda equina with compression. We successfully treated the patient with subtotal tumor resection and postoperative radiation therapy of the entire brain and spinal cord. No further evidence of the disease has been noted elsewhere in the patient during ten years of follow-up. Spinal deformity is thought to occur when young children undergo laminectomy. However in our case, no spinal deformity occurred in the 5-year-old boy over a ten-year follow-up period.
We reported a rare case of spinal myxopapillary ependymoma with cauda equina compression. Subtotal tumor resection and postoperative radiation therapy of the entire brain and spinal cord were effective, and the patient had a good prognosis.
References
1. Kernohan JW,Primary tumors of the spinal cord and
intradural filum terminale. Penfield W, editors. Cytology & cellular pathology of the nervous system. New York: P.B. Hoeber, Inc; 1932. p.993ŌĆō1025.
2. Sonneland PR, Scheithauer BW, Onofrio BM. Myxopapillary ependymoma. A clinicopathologic and immunocytochemical study of 77 cases. Cancer 1985 56:883ŌĆō893. PMID: 4016681.


3. Schild SE, Nisi K, Scheithauer BW, et al. The results of radiotherapy for ependymomas: the Mayo Clinic experience. Int J Radiat Oncol Biol Phys 1998 42:953ŌĆō958. PMID: 9869215.


4. Louis DN, Ohgaki H, Wiestler OD, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 2007 114:97ŌĆō109. PMID: 17618441.



5. Linssen WH, Davies GA. A giant cauda equina ependymoma. J Neurol Neurosurg Psychiatry 1998 65:71PMID: 9667564.



6. Nakamura M, Ishii K, Watanabe K, et al. Long-term surgical outcomes for myxopapillary ependymomas of the cauda equina. Spine (Phila Pa 1976) 2009 34:E756ŌĆōE760. PMID: 19934795.


7. Quraishi NA, Wolinsky JP, Bydon A, Witham T, Gokaslan ZL. Giant destructive myxopapillary ependymomas of the sacrum. J Neurosurg Spine 2010 12:154ŌĆō159. PMID: 20121349.


8. Al-Habib A, Al-Radi OO, Shannon P, Al-Ahmadi H, Petrenko Y, Fehlings MG. Myxopapillary ependymoma: correlation of clinical and imaging features with surgical resectability in a series with long-term follow-up. Spinal Cord 2011 49:1073ŌĆō1078. PMID: 21647167.


9. Fassett DR, Schmidt MH. Lumbosacral ependymomas: a review of the management of intradural and extradural tumors. Neurosurg Focus 2003 15:E13PMID: 15323470.

Fig.┬Ā1
Plain radiographs revealed wider interpedicular distances in the lower lumbar vertebrae. Lumbar spine alignment was normal. There were no sclerotic lesions or lytic destruction noted.
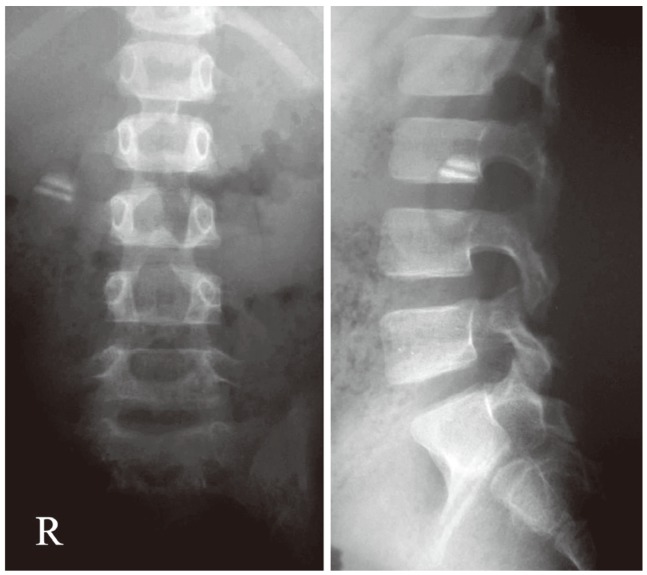
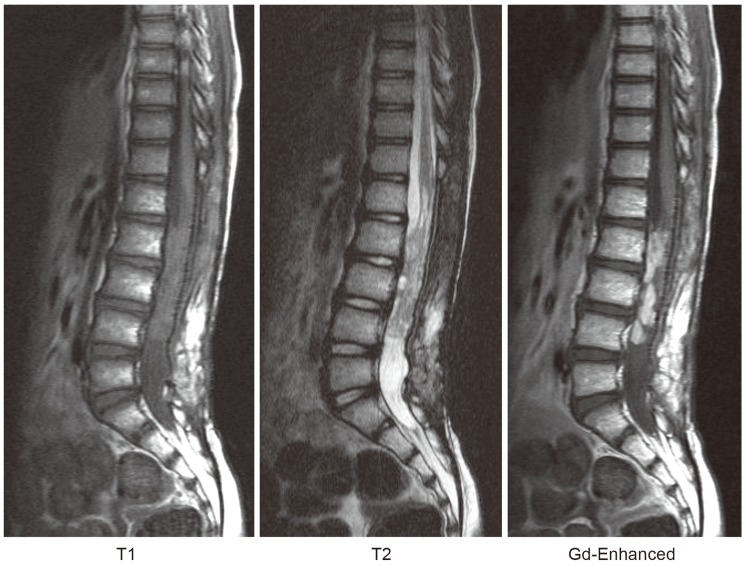
Fig.┬Ā2
Magnetic resonance imaging showed a mass within the cauda equina extending from L1 to L4. The tumor was hypointense on T1-weighted images and hyperintense on T2-weighted images with gadolinium-enhancement. Gd-Enhanced, gadolinium-enhanced.
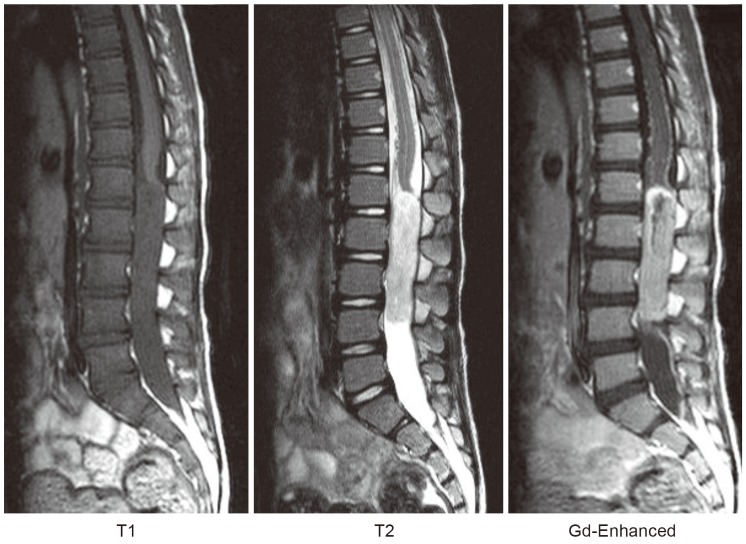
Fig.┬Ā3
Histological examination of the tissue removed during the surgery showed that the myxoid area was positioned between small vessels, around which small tumor cells aggregated. The tumor cells were positive for glial fibrillary acidic protein. (A) H&E, ├Ś100. (B) Glial fibrillary acidic protein, ├Ś100.
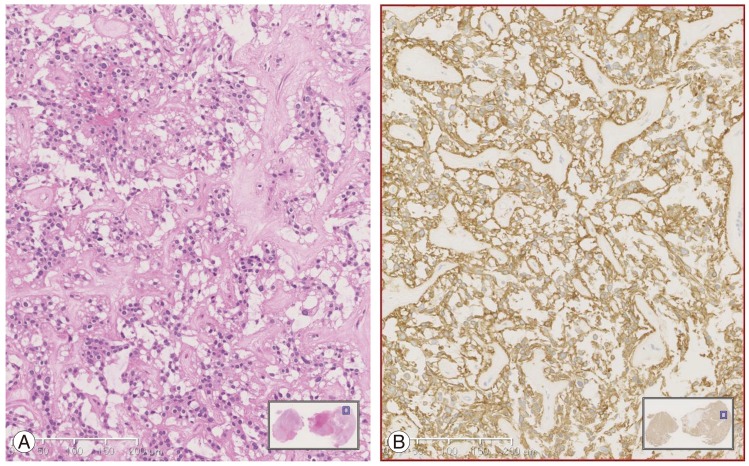
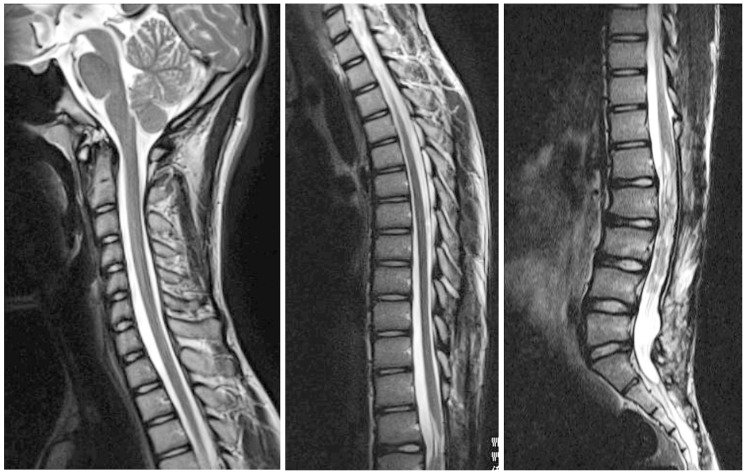
Fig.┬Ā4
Two years after admission, follow-up magnetic resonance imaging revealed a recurrent enhanced tumor from L2 to L4 with a small seeding lesion within the sacral area. Gd-Enhanced, gadolinium-enhanced.

Fig.┬Ā5
Magnetic resonance imaging after the second surgery showed that laminectomy was performed from L1 to L4 to resect the tumor. However the tumor was only partially removed, because it was tightly adhered to many bundles of the cauda equina. Gd-Enhanced, gadolinium-enhanced.